Immunotherapy for lung cancer in Germany
Prof. Dr. med. Frank Gansauge - Head Physician of the Department of Oncology, Immunotherapy and Dendritic Cell Therapy, conducts online consultations about the possibility of Dendritic Cell and Immunotherapy for cancer treatment
Order a consultation - 250 EUR (temporary discount, regular price 1 500 EUR!)
Cancer immunotherapy was awarded the Nobel Prize in Medicine in 2018, which facilitated the technique to quickly enter into the expanded treatment protocols, significantly increasing the effectiveness of the treatment of non-small cell lung cancer and pleural mesothelioma. In Germany, immunotherapy treatment for lung cancer can be successfully carried out at different stages of the disease, allowing the patient's immune system to attack a tumor and its metastases. Immunotherapy for metastatic lung cancer is often the only treatment option, and, in the early stages of cancer, doctors combine it with surgery and chemotherapy. German specialists select drugs individually, considering the genetic and molecular characteristics of the tumor in a particular patient.
Content
- When is immunotherapy administered for lung cancer?
- How is immunotherapy different from other lung cancer treatments?
- What are the types of lung cancer immunotherapy?
- Monoclonal antibodies
- Immune checkpoint inhibitors
- Dendritic cell-based vaccines
- Adoptive T cell transfer
- Hospitals and cost of treatment
- Benefits of immunotherapy for lung cancer treatment
- Organization of immunotherapy for lung cancer in Germany
When is immunotherapy administered for lung cancer?
Immunotherapy is a powerful therapeutic option that is mainly used in people with advanced or recurrent cancer. However, modern protocols recommend earlier administration in order to achieve better responses and longer relapse-free periods. Immunotherapy is now indicated in the following cases:
- Advanced or metastatic lung cancer, as a standard treatment option.
- Adjuvant therapy after a surgery aimed at reducing the risk of cancer recurrence. Eligible patients are people with lymph node involvement or large primary neoplasms.
- Neoadjuvant therapy before a surgery in people with large primary tumors. Neoadjuvant treatment makes it easier for surgeons to remove the neoplasm due to its shrinkage. This approach is now being explored in clinical trials.
- Maintenance therapy, in combination with chemotherapy. The aim is to prolong the period of disease control.
In addition, immunotherapeutic agents are being investigated in many ongoing clinical trials. Scientists search for new drugs and their combinations with other treatments.
How is immunotherapy different from other lung cancer treatments?
Immunotherapy differs from other lung cancer treatments in the way it works. Basically, it interferes with the ability of the body's own immune system to fight cancer, i.e. recognize and attack malignant cells. Other treatments focus on removing or killing cancer cells through different mechanisms and do not involve work of the immunity.
Immunotherapy has its own goals. The primary goal is to enhance the body's immune response against cancer, leading to long-term control or even eradication of the disease. Immunotherapeutic agents cannot destroy the primary tumor or targetedly remove metastatic lesions in the spine. They work to control the disease and prevent its progression.
Another difference is the side effects. Unlike chemotherapy or radiotherapy, immunotherapy does not have serious side effects. Common ones include fatigue, rash and diarrhea. The most serious are immune-related side effects, such as immune-related pneumonitis or colitis. Treatment is generally well tolerated.
What are the types of lung cancer immunotherapy?
The lung cancer immunotherapy uses diverse drug groups. Some of them are ready-made substances that substitute certain functions of a patient’s immunity. Others are substances that make it easier for the immune system to work: they remove tumor masking or teach leukocytes to recognize and destroy the malignant cells better.
The main pharmaceuticals are:
- Monoclonal antibodies
- Immune checkpoint inhibitors
- Dendritic cell-based vaccines
- Adoptive immunotherapy, or CAR T-cell therapy
Healthcare professionals choose the most suitable drug or a combination depending on the clinical situation. Below we will look at each group of medicines in more detail.
Monoclonal antibodies
Monoclonal antibodies are protein molecules that exclusively bind to specific tumor targets. Specific antigens on the surface of malignant cells, specific receptors, and molecules of tumor blood vessels act as targets.
Monoclonal antibodies are synthesized in the laboratory, and one or more specific preparations have been developed for each target. For lung cancer treatment, doctors use drugs that suppress vascular endothelial growth factor (VEGF). These do not allow new arteries to form, and a malignant neoplasm dies from a lack of oxygen and nutrients. This type of monoclonal antibody received FDA approval back in 2006. So far, research is ongoing to find other unique targets for monoclonal antibodies for lung cancer.
In fact, a subset of immune checkpoint inhibitors (see below) are also monoclonal antibodies. Due to their special mechanisms of action, they are isolated in a separate group.
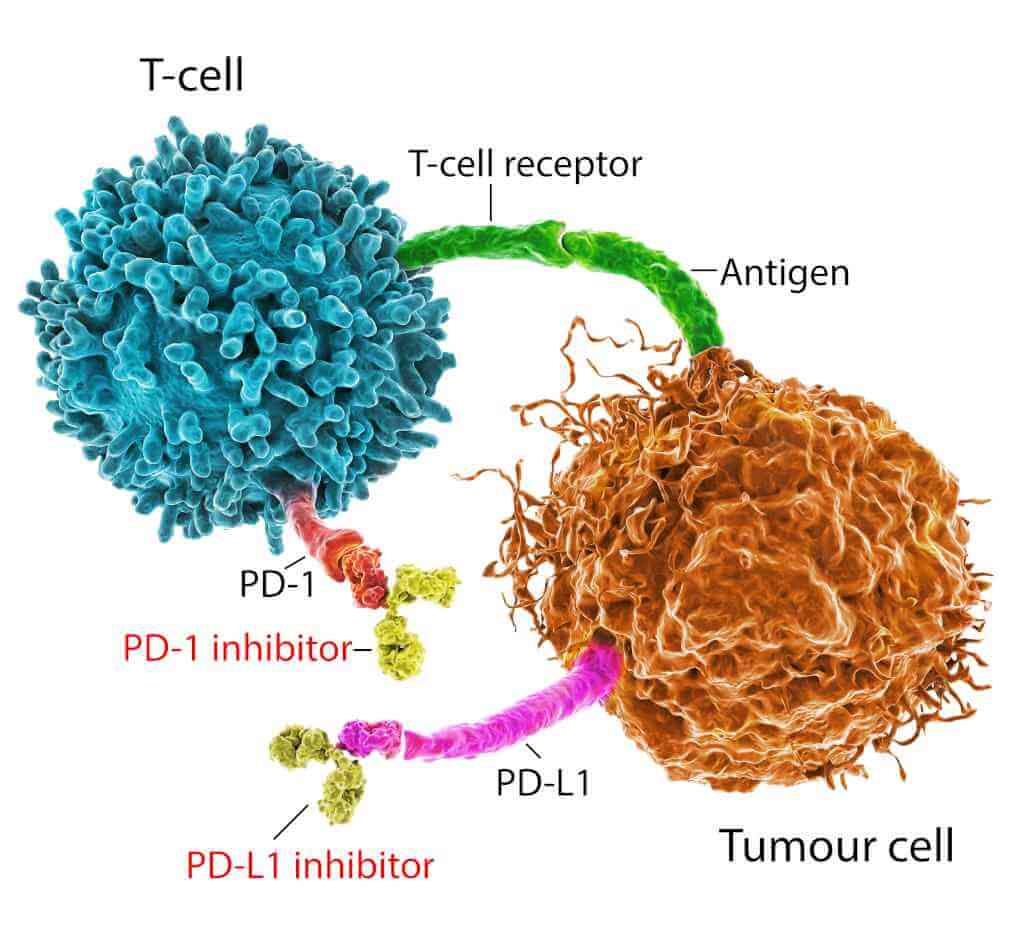
Immune checkpoint inhibitors
The human immune system can destroy several million cancer cells daily. Malignant tumors develop and progress due to the ability to hide or pretend to be normal. Immune checkpoint inhibitors restore anti-cancer immunity by influencing the mechanisms of such masking.
This is the most expansive and most well-studied group of drugs for non-small cell and squamous cell lung cancer, which are actively used in clinics in Germany. This includes the following three types of medications:
- PD-1 inhibitors affect the corresponding protein in T cells (killer cells of the immune system). Normally, PD-1 directs T cells to targets that should not be attacked. Doctors make a neoplasm visible to the immune system by blocking PD-1 on tumor cells;
- PD-L1 inhibitors enhance the process described above. Before starting treatment, doctors conduct tests to check the content of PD-L1 in cancer cells;
- CTLA-4 inhibitors are another option. CTLA-4 is a protein in T cells that regulates their activity. The lower the CTLA-4 levels, the more effective the T cells are at destroying the tumor. CTLA-4 inhibitors can be used together with PD-1 inhibitors and chemotherapy, but not as a stand-alone treatment method.
Immune checkpoint inhibitors suppress the growth of metastases and significantly increase the life expectancy of people with stage 4 and 3 lung cancer.
Dendritic cell-based vaccines
Non-small cell lung cancer can be treated with dendritic cells after a partial or complete surgical tumor removal (adjuvant therapy). Vaccination is equally effective in patients with glandular and squamous cell carcinoma, and clinical studies have proved an increase in the 5-year survival of such patients by 25%.
In most cases, the lung tumor is removed during surgery, and blood monocytes serve as the material for creating an individual vaccine. The finished product is injected subcutaneously. This is well tolerated and does not cause any side effects. A course of 4 injections at an interval of several weeks is required for the formation of a stable antitumor immune response.
In addition to the effect on residual tumors and metastases, vaccination forms immunological memory and prevents the recurrence of oncology in the future.
Another promising application of dendritic cells for advanced lung cancer is their combination with the Newcastle disease virus and γδ T cell-based therapy. This treatment has proved its high success rates in patients with stage 3 and 4 cancer in clinical studies.
Find specialized hospital & treatment
Adoptive T-cell transfer
Adoptive lung cancer immunotherapy, or CAR T-cell therapy, is the most high-tech type of treatment and is carried out only in a few large university hospitals in Germany.
Doctors isolate T-cells from the patient's blood and modify their genetic makeup. This is a complex procedure that gives T-cells the ability to recognize a lung tumor as a prime target for an attack. CAR T-cell therapy overcomes the mechanisms of tumor masking and significantly increases the activity of anti-cancer immunity. At the same time, the size of metastases and the primary tumor decreases, cancer intoxication decreases, and respiratory function improves.
"After completing CAR T-cell therapy, new T lymphocytes retain their ability to attack a lung tumor for a long time."
A simpler variant of adoptive cell therapy is to treat T cells with substances similar in composition to lung tumor antigens. During such contact, T cells "remember" antigens in order to find them in the patient's body in the future and destroy the tumor. Such a treatment option allows physicians to improve a person's health status quickly, and anti-cancer immunity lasts for several months.
DENDRITIC CELL THERAPY - Professor Frank Gansauge
Hospitals and cost of treatment
Lung cancer treatment in Germany is provided by academic and university hospitals. Top-class medical facilities offer their patients minimally invasive surgery, sparing types of radiation therapy, and innovative medicines, including modern immunotherapy.
During the first visit to a hospital, doctors study the results of the patient's diagnostic tests, ask questions about previous treatment, and conduct a clinical examination. They can also carry out additional tests or perform CT/MRI scans if required. All these examinations are followed by a tumor board aimed at developing a customized treatment plan for a patient. If you want to come specifically for immunotherapy, you can first consult with a doctor from the German clinic remotely.
The prices for treatment are determined individually and depend on the clinic, the patient's age, and diagnosis. The average cost of comprehensive diagnostics, including a lung biopsy with a histological examination and the development of a treatment regimen, is about 16,400 €.
Benefits of immunotherapy for lung cancer treatment
Although treatment decisions are always individualized based on the type and stage of lung cancer and the patient's overall health, immunotherapy offers patients several potential benefits, such as:
- Extended survival in advanced or metastatic lung cancer compared to the conventional treatments.
- Improved quality of life during treatment due to a mild side effect profile. Immunotherapy can also be used as a palliative treatment to alleviate symptoms.
- Reduced risk of relapse after potentially curative surgical interventions.
- Long-term disease control, making cancer a chronic rather than a terminal disease.
The addition of immunotherapeutic agents is particularly effective in patients with non-small cell lung cancer that expresses certain biomarkers, such as PD-L1. So the benefits may be more or less substantial, but they are always there.
| Cancer stage | Response to standard treatment protocol | Response to standard treatment protocol + Immunotherapy |
| Stage 3 | 50% | 70% |
| Stage 4 | 20% | 50% |
Organization of immunotherapy for lung cancer in Germany
You are welcome to use the Booking Health service to undergo your immunotherapy or comprehensive lung cancer treatment in Germany. Booking Health is an international medical tourism provider that has been organizing the treatment of people with cancer from 75 countries in leading German hospitals for over 12 years.
Booking Health will help you to:
- select a clinic and a doctor specializing in immunotherapy for lung cancer;
- conduct a preliminary remote consultation with a doctor from a German hospital;
- learn a preliminary treatment regimen;
- make an appointment on the preferred date without a long waiting period;
- communicate with your doctor and medical staff through an interpreter;
- undergo your treatment at a favorable cost and without overpricing for foreign patients (saving up to 50%);
- buy medicines and forward them to your native country to continue your outpatient treatment;
- maintain contact with the hospital after the completion of your treatment;
- control hospital invoices and return unused deposit funds to your bank account;
- obtain medical insurance;
- organize additional diagnostic examinations, treatment, or rehabilitation;
- book the most suitable airline tickets, transfers, and apartments, and obtain a visa and an invitation for treatment, if required.
Doctors and coordinators of the Booking Health company will accompany you at all stages of your cancer treatment. Do not hesitate to contact them for any medical or organizational issues.
Choose treatment abroad and you will for sure get the best results!
Authors:
The article was edited by medical experts, board certified doctors Dr. Nadezhda Ivanisova and Dr. Vadim Zhiliuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
Journal for Immunotherapy of Cancer
Read:
Cancer immunotherapy in Germany
Treatment of stage 4 lung cancer in Germany
Lung cancer treatment with dendritic cells in Germany
TOP 5 Hospitals for Lung Cancer Treatment in Germany