The program includes:
- Initial presentation in the clinic
- clinical history taking
- review of medical records
- physical examination
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- TSH-basal, fT3, fT4
- tumor markers (AFP, CEA, СА-19-9)
- inflammation indicators (CRP, ESR)
- indicators of blood coagulation
- abdominal ultrasound scan
- CT/MRI of abdomen
- preoperative care
- percutaneous embolization (coiling) or chemoembolization
- symptomatic treatment
- cost of essential medicines
- nursing services
- elaboration of further recommendations
Indications
- Inoperable liver metastases
- Poor response to systemic chemotherapy
Treatment is not indicated in:
- Presence of extrahepatic metastases
- Affection of more than 70% of the liver
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examination, such as the assessment of liver and kidney function, ultrasound scan, CT scan and MRI. This will allow the doctor to determine which vessels are feeding the tumor and its metastases, as well as determine how well you will tolerate the procedure.
Chemoembolization begins with local anesthesia and catheterization of the femoral artery. The thin catheter is inserted through a few centimeters long incision of the blood vessel. The doctor gradually moves the catheter to the vessel feeding the primary tumor or its metastases. The procedure is carried out under visual control, an angiographic device is used for this. The vascular bed and the position of the catheter in it are displayed on the screen of the angiograph.
When the catheter reaches a suspected artery, a contrast agent is injected through it. Due to the introduction of the contrast agent, the doctor clearly sees the smallest vessels of the tumor and the surrounding healthy tissues on the screen of the angiograph. After that, he injects emboli into the tumor vessels through the same catheter.
Emboli are the spirals or the liquid microspheres. The type of embolus is selected individually, taking into account the diameter of the target vessel. When carrying out chemoembolization, a solution of a chemotherapy drug is additionally injected into the tumor vessel. Due to the subsequent closure of the vessel lumen with an embolus, the chemotherapy drug influences the tumor for a long time. In addition, the drug does not enter the systemic circulation, which allows doctors to use high doses of chemotherapeutic agents without the development of serious side effects. Chemoembolization leads to the destruction of the tumor or slowing down its progression.
After that, the catheter is removed from the artery. The doctor puts a vascular suture on the femoral artery and closes it with a sterile dressing. During chemoembolization, you will be awake. General anesthesia is not used, which significantly reduces the risks of the procedure and allows performing it on an outpatient basis, avoiding long hospital stay.
After the first procedure, you will stay under the supervision of an interventional oncologist and general practitioner. If necessary, you will receive symptomatic treatment. As a rule, a second chemoembolization procedure is performed in 3-5 days after the first one in order to consolidate the therapeutic effect. After that, you will receive recommendations for further follow-up and treatment.
Required documents
- Medical records
- Abdominal ultrasound (if available)
- MRI/CT scan of the abdomen (if available)
- Biopsy results (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
The Department of Adult and Pediatric Neurosurgery, Spinal Surgery at the Westpfalz Hospital Kaiserslautern offers the full range of diagnostics and surgical treatment of diseases of the central and peripheral nervous system. The department's specialists regularly provide assistance to patients with spinal cord and brain tumors and injuries, nerve ending lesions, functional disorders of the nervous system, vascular diseases and cerebral malformations, herniated intervertebral discs, spinal stenosis. As for the common diseases in young patients, it is worth highlighting hydrocephalus and meningomyelocele, as well as various malignant neoplasms. The department has at its disposal advanced diagnostic and therapeutic equipment, and the long-term experience of the medical staff allows high-precision diagnostics and subsequent surgical treatment with minimal risks. The treatment of children and adolescents is carried out by a specially trained team of experts. The department is headed by PD Dr. med. Kajetan von Eckardstein.
The department has excellent diagnostic capabilities, including computed tomography, magnetic resonance imaging, a neurophysiological laboratory for electroencephalography, electromyography, evoked potential testing and transcranial Doppler ultrasonography of the cerebral vessels. Since any surgical intervention on the brain or spinal cord is associated with a high risk of injury to vital areas of these organs, the specialists always pay special attention to planning each stage of the surgical intervention. If required, the specialists in the field of traumatology and orthopedics, neurology, pediatrics, radiology and others are involved in the therapeutic process. Close cooperation with doctors of various specialties guarantees a comprehensive approach to diagnostics and treatment, as well as subsequent rehabilitation.
To minimize the risk of trauma to nearby anatomical structures, almost all surgical interventions on the brain and spinal cord are performed using modern surgical microscopes. Whenever required, intraoperative fluorescence can be used. This technique allows for imaging the vessels of the operating field. An integral part of operations is the use of neuronavigation for the most accurate execution of surgical incisions, intraoperative control of the functions of the nervous system and exclusion of trauma to the healthy tissues. Spinal stabilizing surgeries are performed using neuronavigation and under the guidance of 3D X-ray. All these technical capabilities, combined with the professionalism of the department's neurosurgeons, make it possible to heal even the most complex pathologies of the nervous system.
Most surgical interventions on the brain, spinal cord and peripheral nervous system are performed using minimally invasive surgical techniques. In some cases, endoscopic techniques can also be used. This approach contributes to minimal pain in the postoperative period and significantly reduces the risks to the patient's health. At the end of the treatment, patients undergo a comprehensive rehabilitation program, which is developed individually for each clinical case. During the rehabilitation process, experienced doctors, physiotherapists and other specialists work with patients. The medical staff strives to give the patient the opportunity to return to their usual way of life in the shortest possible time and with the best results.
The main department's clinical focuses include:
- Surgical treatment of oncological and benign diseases of the brain and spinal cord
- Meningioma
- Pituitary adenoma
- Acoustic neuroma
- Pineal tumors
- Brain metastases
- Glioma
- Astrocytoma
- Oligodendroglioma
- Ependymoma
- Glioblastoma
- Surgical treatment of cerebrovascular pathologies
- Brain aneurysms
- Arteriovenous malformations
- Cavernomas
- Dural arteriovenous fistulas
- Surgical treatment of functional pathologies of the nervous system
- Trigeminal neuralgia
- Hemifacial spasm
- Surgical treatment of pathologies of the peripheral nervous system
- Peripheral nerve compression syndromes
- Tumors of the peripheral nervous system
- Surgical treatment of spinal diseases
- Facet syndrome
- Herniated discs
- Spinal stenosis
- Spondylolisthesis
- Scoliosis
- Spinal injuries
- Surgical treatment of diseases of the nervous system in children
- Hydrocephalus
- Meningomyelocele
- Brain tumors
- Surgical treatment of other diseases of the nervous system
The department's surgical options include:
- Minimally invasive surgery
- Endoscopic procedures
- Microsurgical procedures
- Awake brain surgery (for example, for brain tumor resection)
- Other surgical techniques
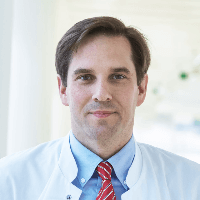
Curriculum vitae
PD Dr. med. Kajetan von Eckardstein is a board certified neurosurgeon, and specializes in vascular neurosurgery, functional neurosurgery, complex interventions on the spine and peripheral nerve endings. After completing his studies in Berlin, the doctor worked as an assistant physician at the Helios Hospital Berlin-Buch, where he later served as a senior physician. From 2006 to 2008, Dr. Kajetan von Eckardstein worked as a neurosurgeon at the Mayo Clinic, Rochester, Minnesota, USA. Since 2008, he has held the position of senior physician at the University Hospital Goettingen, where he has also served as managing senior physician since 2011. Currently, Dr. med. Kajetan von Eckardstein is the head physician of the Department of Adult and Pediatric Neurosurgery, Spinal Surgery at the Westpfalz Hospital Kaiserslautern. The doctor's area of expertise also includes deep brain stimulation. In recent years, Dr. von Eckardstein has been actively involved in scientific activities. His research focuses on the implantation of neurostimulants and the surgical treatment of movement disorders due to neurological diseases, including Parkinson's disease.
Photo of the doctor: (c) Westpfalz-Klinikum GmbH
About hospital
The Westpfalz Hospital Kaiserslautern is a modern maximum care medical facility, which guarantees a patient high professionalism, impeccable quality of medical care and a humane attitude. The hospital has more than 25 specialized departments and institutes, whose tasks include accurate diagnostics and effective treatment of almost all diseases. The hospital has about 1,400 beds for inpatient treatment. Many diagnostic and therapeutic measures are also provided on an outpatient basis. The medical staff of the hospital employs over 4,000 staff members and admits about 160,000 patients annually.
The patient's health is in the hands of a highly qualified team of doctors and nursing staff, who regularly attend advanced training courses and have great opportunities for improving their knowledge in the field of the latest advancements in medicine. The specialists of the hospital apply in their practice the very latest internationally recognized treatment methods and work with advanced medical equipment, which guarantees an optimal result. They also devote sufficient time to personal communication with patients and their relatives. The treatment tactics are planned on the basis of the patient's specific clinical data. Whenever possible, the most sparing therapeutic procedures are used.
It should be noted that the hospital has implemented the strictest quality control system, which serves as a tool for maintaining a high level of organization of the work of its employees. This system allows for close monitoring of the structural organization of work (equipment, types of therapy), the quality of work of employees and the final treatment result, which is the main indicator of the effectiveness of the work of doctors.
Photo: (с) depositphotos
Accommodation in hospital
Patients rooms
The patients of the Westpfalz Hospital Kaiserslautern live in comfortable single, double and triple rooms with the necessary amenities to ensure a comfortable environment throughout their stay in the hospital. The standard patient room furnishings include a comfortable automatically adjustable bed, a bedside table, a telephone, a radio and a TV. The phone also has a radio and TV control function.
If desired, the patient may stay in an enhanced-comfort room, which additionally includes a mini fridge, a safe, a hairdryer and toiletries.
Meals and Menus
The clinic offers a healthy and balanced diet, which is selected for each patient individually, depending on the clinical indications. Breakfast is served buffet style, and there is a choice between two set menus for lunch and dinner. The menu features vegetarian options and specialties for certain faiths. All dishes are prepared from high quality, fresh ingredients, while special steam kitchen appliances ensure maximum retention of nutrients.
Further details
Standard rooms include:
Accompanying person
Your accompanying person may stay with you in your patient room or at the hotel of your choice during the inpatient program.
Hotel
You may stay at the hotel of your choice during the outpatient program. Our managers will support you for selecting the best option.