The program includes:
- Initial presentation in the clinic
- clinical history taking
- physical examination
- review of medical records
- laboratory tests:
- complete blood count
- biochemical analysis of blood
- TSH-basal, fT3, fT4
- indicators of inflammation (CRP, ESR)
- indicators blood coagulation
- ultrasound/ CT/ MRI
- preparation according to preoperative standard
- lipoma resection
- symptomatic treatment
- control examinations
- the cost of essential medicines and materials
- nursing services
- full hospital accommodation
- explanation of future recommendations
- written statement
Required documents
- Medical records
- US scan (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
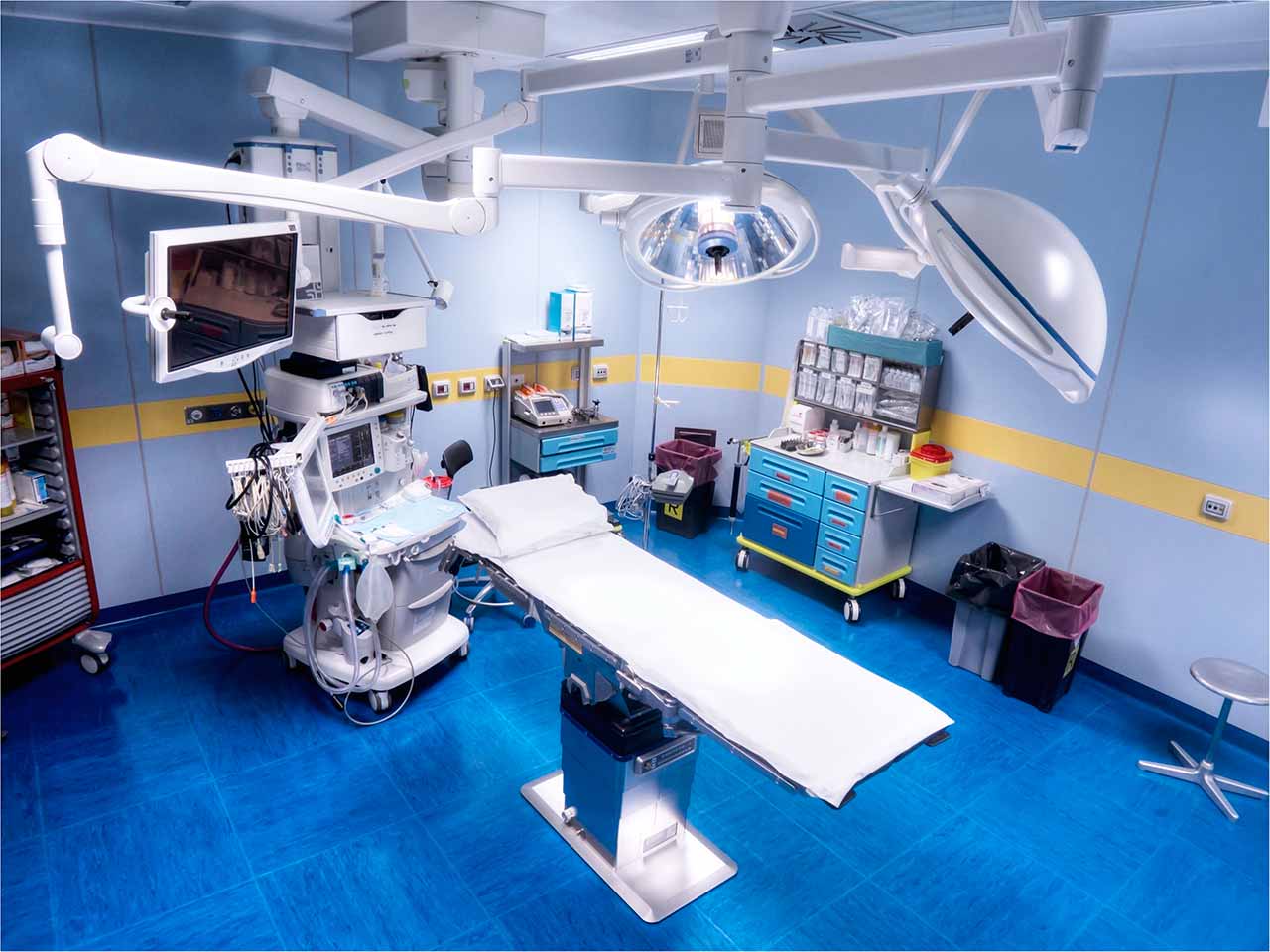
About the department
The Department of General and Abdominal Surgery at the Hirslanden Clinic Meggen offers the full range of surgical treatment for abdominal diseases, including the gallbladder, colon and small intestine, liver, esophagus, bile ducts, stomach, pancreas, endocrine pathologies, as well as proctological diseases. The department has state-of-the-art medical equipment for surgical procedures of any complexity – from major open operations to the most sparing, minimally invasive laparoscopic and laser interventions. After the surgical treatment, each patient receives appropriate care, which contributes to the complete recovery of the body. The Chief Physician of the department is Dr. med. Walter Gantert.
The department's specialists keep pace with innovations in medicine, thanks to which they offer their patients the most effective treatment with minimal trauma to healthy tissues. As of today, one of the most advanced surgical techniques is SILS (single incision laparoscopic surgery). In contrast to the classical laparoscopic surgery, during which the surgeon usually makes 3-5 small skin incisions up to 5-12 mm in size in different parts of the anterior abdominal wall in order to form an access, the SILS technique allows the doctor to carry out an effective operation, performing only one incision of 15-20 mm at the navel. The key advantages of the innovative surgical technique are minimal tissue trauma, rapid postoperative recovery and lack of scars. In addition, the risk of complications and infection is practically equal to zero. The SILS surgery requires a special miniature, about 5 mm in size, optical equipment and laparoscopic instruments. All this is available in the department and is successfully applied for the benefit of patients. One of the most effective fields of application of this technology is the operation to treat gallstones (cholecystectomy).
The department's competence includes the treatment of various types of hernias – inguinal, umbilical, femoral, epigastric, incisional, etc. One of the most common pathologies is an inguinal hernia. To treat it, the department uses a modern, sparing operation TEEP (total endoscopic extraperitoneal hernioplasty). The TEEP technique is ideal for the treatment of primary inguinal hernias, especially in the case of bilateral hernias or recurrent hernia after open surgery. The operation requires only three small skin incisions. The main difference from transabdominal hernioplasty (TAPP) is that during the TEEP operation the peritoneum is not opened – the intervention is performed in the preperitoneal space. Working area is created in the preperitoneal space with the help of a special balloon dissector, where a video camera and two surgical instruments up to 5 mm in size are placed. After the necessary therapeutic manipulations, a mesh is placed at the exit point of the hernia to strengthen the weak areas of the inguinal canal. After gas desufflation, the mesh is firmly pressed in the peritoneum. The main advantage of the TEEP technique is minimal pain during the postoperative period. In addition, the patient can leave the clinic within one day after the operation. Total endoscopic extraperitoneal hernioplasty (TEEP) minimizes the risk of damage to the abdominal organs and the development of adhesions, since the operation is performed outside the abdominal cavity.
The treatment of colon cancer is also one of the priority clinical tasks of the surgeons. The pathology requires accurate diagnostics using colonoscopy and sigmoidoscopy. If colon polyps are detected during colonoscopy, the doctor removes them immediately, as polyps are often precursors of cancer. The removed material is sent for histological examination. If a malignant process is detected, the patient is prescribed surgery. Before the operation, CT or MRI scans of the abdominal organs, as well as chest X-ray are necessarily performed to determine the exact location, size of the tumor, and search for metastases. The purpose of the surgery is the total removal of the bowel tumor. The surgeons remove the intestinal area affected by the cancer process and then form anastomosis (manually or with a medical stapler). In some cases, a minimally invasive intervention is possible. In most cases, the period of hospitalization after the surgery is 5-7 days.
The surgical spectrum of the department includes:
- Endocrine surgery
- Thyroid and parathyroid surgery
- Intraoperative neuromonitoring of the recurrent laryngeal nerves
- Rapid intraoperative parathyroid hormone assay in the blood
- Laparoscopic interventions on the adrenal glands
- Thyroid and parathyroid surgery
- Diagnostic laparoscopy
- Laparoscopic treatment of gastroesophageal reflux disease and hiatal hernia
- Surgical interventions on the stomach
- Open and laparoscopic interventions
- Surgical interventions on the gallbladder and biliary tracts
- Open and laparoscopic SILS cholecystectomy
- Surgical interventions on the liver, pancreas and spleen
- Open and laparoscopic interventions
- Small bowel surgery
- Meckel's diverticulum
- Gastrointestinal neuroendocrine tumors
- Inflammatory bowel disease
- Bowel cancer
- Open and laparoscopic interventions
- Colorectal surgery
- Diverticulitis
- Polyps
- Inflammatory bowel disease
- Colorectal cancer
- Rectal prolapse
- Open and laparoscopic interventions
- Anorectal surgery
- Hemorrhoid
- Longo procedure (stapled hemorrhoidopexy)
- Closed hemorrhoidectomy (Ferguson technique)
- Chronic anal fissures
- Fistulas and abscesses
- Pilonidal sinus
- Hemorrhoid
- Hernia repair surgery
- Inguinal hernias
- Umbilical hernias
- Femoral hernias
- Epigastric hernias
- Incisional hernias
- Total endoscopic extraperitoneal hernioplasty (TEEP)
- Transabdominal preperitoneal hernia repair (TAPP)
- Liechtenstein operation
- IPOM laparoscopic hernia repair surgery
- Rives-Stoppa hernia repair surgery
- Port system placement
- Minor outpatient surgical interventions
- Emergency surgery
- Other surgical options
Curriculum vitae
Professional Career
- 2001 - 2002 Senior Physician in the Department of Surgery at the University Hospital Basel.
- 1998 - 2001 Senior Physician, Department of Surgery A, Cantonal Hospital Lucerne.
- 1996 - 1998 Research Fellow on Clinical Researches in Laparoscopic Surgery and Clinical Trainer, Videoscopic Surgery Center, Department of Surgery, University of California, San Francisco, CA, USA.
- 1995 - 1996 Deputy Senior Physician, then Senior Physician, Department of Surgery, Cantonal Hospital Winterthur.
- 1994 Assistant Physician, Department of Surgery at the Cantonal Hospital Winterthur.
- 1992 - 1993 Assistant Physician in the Department of Surgery at the University Hospital Zurich.
- 1991 Doctor of the Swiss Air Rescue Service in Kloten and at various REGA helicopter bases.
- 1990 Military Doctor, Department of Surgery, District Hospital in Herisau.
- 1988 - 1990 Assistant Physician, Department of Surgery, Regionalspital Interlaken.
Higher Education and Postgraduate Training
- 1997 Board certification in Surgery, Swiss Medical Association (FMH).
- 1996 Doctoral Degree in Medicine, University of Zurich.
- 1998 ECFMG Certificate (Educational Commission for Foreign Medical Graduates).
- 1987 State Examination at the Faculty of Medicine, University of Bern.
- 1980 - 1987 Study of Human Medicine at the Faculty of Medicine, University of Bern.
Clinical Interests
- Abdominal surgery.
- Minimally invasive / laparoscopic and thoracoscopic surgery.
- Cancer surgery.
- Bariatric surgery.
- General surgery.
Memberships in Professional Societies
- Swiss Medical Association (FMH).
- Swiss Society for Surgery (SGC).
- Board Member of the Swiss Association for Laparoscopic and Thoracoscopic Surgery (SALTC).
- Swiss Association of Visceral Surgery (SGVC).
- International Society of Surgery (ISS/SIC).
- Society for Surgery of the Alimentary Tract (SSAT).
- Society of American Gastrointestinal and Endoscopic Surgeons (SAGES).
- European Association for Endoscopic Surgery (EAES).
- International Society for Computer Aided Surgery (ISCAS).
- Swiss Study Group for Laser Surgery (SALC).
- Swiss Society for the Study of Morbid Obesity and Metabolic Disorders (SMOB).
- Swiss Hernia Surgery Working Group (SAH).
Photo of the doctor: (с) Hirslanden Clinic Meggen
About hospital
The Hirslanden Clinic Meggen is a modern multidisciplinary medical facility in Switzerland, where the patient receives top-class medical care according to his individual needs and wishes. Since 2014, the clinic has been part of the prestigious Hirslanden Private Hospital Group, which has an excellent reputation in Switzerland and in many other countries of the world. The cutting-edge medical technologies, the highest quality of treatment, the advanced experience of doctors and nurses at the clinic form a solid basis for successful treatment of both common diseases and rare pathologies, including especially complex clinical cases. The specialists of the clinic admit more than 1,000 inpatients, and also provide their medical services to more than 7,000 outpatients annually.
The specialization of the clinic covers many branches of modern medicine, including general surgery, vascular surgery, hand surgery, maxillofacial surgery, dermatology, gynecology and obstetrics, otolaryngology, ophthalmology, orthopedics and traumatology, urology and others. Each of them is represented by a competent team of doctors who have rich clinical experience, regularly improve their skills undergoing advanced training courses, and also provide medical care according to the latest clinical protocols.
For more than 10 years, the clinic has been implementing the quality control system, which is unified for all medical centers of the Hirslanden Private Hospital Group. This system serves for the assessment of the quality of medical services and the safety of treatment. As part of the monitoring, data on the treatment success rates of the clinic are published annually, which give the patient the opportunity to make sure of the reliability and efficiency of medical service even before contacting the clinic.
An important role is also played by the pleasant and friendly atmosphere, which prevails in the clinic. The attending physicians make every effort to establish contact with the patient, surround him with care and make the stay in the clinic as comfortable as possible. During the medical consultations, patients receive comprehensive information about possible treatment options for their disease. Medical specialists practice an individualized approach, so each treatment regimen is unique and aimed at achieving the optimal result for a particular patient.
Photo: (с) Hirslanden Clinic Meggen, (c) depositphotos
Accommodation in hospital
Patients rooms
The patients of the Hirslanden Clinic Meggen live in cozy rooms with excellent layout and modern design. The standard patient rooms are equipped with a comfortable automatically adjustable bed, a bedside table, a table and chairs for receiving visitors, a wardrobe for storing personal belongings. The patient room also has a TV, a telephone and Wi-Fi. Each patient room includes an ensuite bathroom with shower and toilet.
Meals and Menus
The patient and the accompanying person are offered tasty and balanced three meals a day. If for some reason you do not eat all foods, you will be offered an individual menu. Please inform the medical staff about your food preferences prior to treatment.
Further details
Standard rooms include:
Religion
Religious services can be provided upon request.
Accompanying person
During the inpatient program, the accompanying person can live with the patient in a patient room or a hotel of his choice. Our managers will help you choose the most suitable option.
Hotel
During an outpatient program, the patient can stay at the hotel of his choice. Our managers will help you choose the most suitable option.