The program includes:
- Initial presentation in the hospital
- Clinical history taking
- Review of available medical records
- Physical examination
- Laboratory tests:
- Complete blood count
- General urine analysis
- Biochemical analysis of blood
- Tumor markers
- Inflammation indicators (CRP, ESR)
- Coagulogram
- Ultrasound scan
- CT scan / MRI
- Preoperative care
- Embolization or chemoembolization, 2 procedures
- Symptomatic treatment
- Cost of essential medicines
- Nursing services
- Elaboration of further recommendations
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examination, such as the assessment of liver and kidney function, ultrasound scan, CT scan and MRI. This will allow the doctor to determine which vessels are feeding the tumor and its metastases, as well as determine how well you will tolerate the procedure.
Chemoembolization begins with local anesthesia and catheterization of the femoral artery. The thin catheter is inserted through a few centimeters long incision of the blood vessel. The doctor gradually moves the catheter to the vessel feeding the primary tumor or its metastases. The procedure is carried out under visual control, an angiographic device is used for this. The vascular bed and the position of the catheter in it are displayed on the screen of the angiograph.
When the catheter reaches a suspected artery, a contrast agent is injected through it. Due to the introduction of the contrast agent, the doctor clearly sees the smallest vessels of the tumor and the surrounding healthy tissues on the screen of the angiograph. After that, he injects emboli into the tumor vessels through the same catheter.
Emboli are the spirals or the liquid microspheres. The type of embolus is selected individually, taking into account the diameter of the target vessel. When carrying out chemoembolization, a solution of a chemotherapy drug is additionally injected into the tumor vessel. Due to the subsequent closure of the vessel lumen with an embolus, the chemotherapy drug influences the tumor for a long time. In addition, the drug does not enter the systemic circulation, which allows doctors to use high doses of chemotherapeutic agents without the development of serious side effects. Chemoembolization leads to the destruction of the tumor or slowing down its progression.
After that, the catheter is removed from the artery. The doctor puts a vascular suture on the femoral artery and closes it with a sterile dressing. During chemoembolization, you will be awake. General anesthesia is not used, which significantly reduces the risks of the procedure and allows performing it on an outpatient basis, avoiding long hospital stay.
After the first procedure, you will stay under the supervision of an interventional oncologist and general practitioner. If necessary, you will receive symptomatic treatment. As a rule, a second chemoembolization procedure is performed in 3-5 days after the first one in order to consolidate the therapeutic effect. After that, you will receive recommendations for further follow-up and treatment.
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
According to the Focus magazine, the Department of Adult and Pediatric Urology at the University Hospital Marburg UKGM ranks among the best German medical facilities for prostate cancer treatment!
The department offers all diagnostic and therapeutic services in the field of its competence and specializes in the treatment of diseases of the genitourinary system in men of all age groups. The department has 46 beds for inpatient medical care. One of the key focuses is prostate cancer treatment (certification of the German Cancer Society as a Prostate Cancer Center). The doctors of the department are also highly professional in the treatment of diseases of the external genital organs in men, pathologies of the kidneys, adrenal glands, ureters, bladder and urethra in men and women. The department is headed by Prof. Dr. med. Rainer Hofmann.
The department’s pediatric urologists are involved in the treatment of malformations and diseases of the kidneys, ureters, bladder and genitals in newborns and children. Of particular interest is medical care for small patients with impaired urine outflow, vesicoureteral reflux, testicular malformations, foreskin stenosis and urinary incontinence, including nocturnal enuresis. Most operations in children with pathologies of the genitourinary system can be performed on an outpatient basis.
The department widely uses sparing minimally invasive surgery, namely laparoscopy and endourology. Laparoscopic interventions are mostly used for kidney and adrenal tumor resection, whereas endourological procedures serve for both invasive diagnostics and treatment of urinary tract diseases with access through the urethra. Today, sparing surgical techniques are the gold standard. They provide minimal trauma to healthy tissues, speedy recovery after surgery and minimal risk of postoperative complications.
The department’s spectrum of medical services includes:
- Diagnostics and treatment of prostate cancer (within the framework of a specialized center certified by the German Cancer Society)
- Diagnostics and treatment of bladder cancer
- Diagnostics and treatment of kidney cancer
- Diagnostics and treatment of testicular cancer
- Diagnostics and treatment of urinary incontinence (urogynecology)
- Stress urinary incontinence
- Urge urinary incontinence
- Overactive bladder
- Mixed urinary incontinence
- Neurogenic bladder dysfunction
- Chronic urinary incontinence
- Extraurethral urinary incontinence
- Chronic pelvic pain
- Conservative treatments
- Physical exercises to strengthen pelvic floor muscles
- Electrostimulation and biofeedback
- Installation of pessaries
- Drug therapy
- Surgical treatments
- Bladder sphincter injections
- Sling procedures
- Burch procedure
- Vaginal prolapse correction
- Artificial sphincter implantation
- Botulinum toxin A injections
- Conservative treatments
- Diagnostics and treatment of urolithiasis
- Extracorporeal shock wave lithotripsy
- Ureterorenoscopy
- Percutaneous nephrolitholapaxia
- Minimally invasive treatment
- Laparoscopy (mostly kidney and adrenal tumor resection)
- Endourological procedures
- Laser therapy
- Treatment of benign prostatic hyperplasia using a Greenlight laser and a holmium laser
- Laser lithotripsy for urolithiasis
- Laser removal of genital warts
- Flexible and rigid ureterorenoscopy
- Removal of urinary tract stones
- Diagnostics and treatment of tumors
- Resectoscopy
- Transurethral resection
- Removal of bladder tumors
- Therapy of benign prostatic hyperplasia
- Cystoscopy (for diagnostic and therapeutic purposes)
- Cystoscopic administration of drugs into the bladder wall (in case of urinary incontinence)
- Ureteral stent placement
- Fluorescence cystoscopy and resection of bladder malignancies
- Ureterorenoscopy and cystoscopy using video/HDTV monitoring
- Percutaneous nephrolitholapaxia for kidney stones
- Percutaneous nephrostomy (in case of urinary retention due to ureteral stenosis, ureteral stones, etc.)
- Laser therapy
- Pediatric urology
- Outpatient surgery
- Circumcision
- Orchidopexy (surgery to correct undescended testes)
- Umbilical hernia repair
- Hydrocele resection
- Treatment of varicocele in children
- Correction of labial fusion
- Diagnostics and treatment of diseases of the external genital organs
- Phimosis
- Inguinal hernia
- Hydrocele
- Cryptorchidism (drug therapy, open surgery, minimally invasive laparoscopic intervention)
- Hypospadias
- Pediatric varicocele
- Labial fusion
- Penile torsion
- Urethral stenosis
- Acute scrotum (testicular pain due to various reasons)
- Diagnostics and treatment of diseases of the lower urinary tract
- Vesicoureteral reflux
- Ectopic ureteral orifice
- Urethral valves
- Diagnostics and treatment of diseases of the upper urinary tract
- Kidney stones
- Ureteropelvic junction obstruction
- Kidney dysfunction
- Partial kidney dysfunction in case of double kidney
- Diagnostics, differential diagnostics and treatment of urination disorders
- Nocturnal enuresis
- Urinary incontinence in children (in the daytime)
- Neurogenic bladder
- Outpatient surgery
- Other diagnostic and therapeutic options
Curriculum vitae
- 1973 - 1979 Study of Human Medicine.
- 1979 Doctoral thesis defense at the Friedrich-Alexander University Erlangen-Nuremberg. Subject: "Protein electrophoresis in polyacrylamide gel - a new device for electrophoretic elution of individual proteins from a gel".
- 1979 - 1980 Work in the Department of Surgery, Sutherland Hospital in Sydney, Australia.
- 1980 - 1981 Department of Surgery, Hospital Bad Windsheim.
- 1981 - 1989 Department of Urology, University Hospital Rechts der Isar Munich.
- 1989 Senior Physician, University Hospital Rechts der Isar Munich.
- 1990 - 1991 Associate Professor of Urology, University of California, San Francisco.
- 1991 Leading Senior Physician, University Hospital Rechts der Isar Munich.
- 1989 Habilitation and Venia legendi. Subject: "Technical development, biological effects and the first clinical experience of laser-induced shock-wave lithotripsy for urinary tract stones".
- 1990 PD title.
- 1996 Extraordinary Professorship.
- 1998 Appointment as Professor for Urology at the Philipp University of Marburg.
- Since 12.1998 Head of the Department of Adult and Pediatric Urology at the University Hospital Marburg UKGM.
- 2007 Additional specialization in the field of tumor drug therapy, Medical Association of the State of Hesse.
Scientific Awards and Honors
- 1984 Mendelian Inheritance Man for work on the subject: "Hereditary autosomal dominant form of men’s bladder diverticulum".
- 1988 Best Report in Experimental Urology, Aachen.
- 1992 Maximilian Nietze Prize of the German Society of Urology.
- 1995 Erwin Fertig Prize, Uro-Oncology.
- 1997 1st Video Prize, World Congress of Urology in Budapest (presentation of video works).
Memberships in Professional Societies
- Student Fund of the German People.
- German Society of Urology.
- Bavarian Society of Urology.
- American Urological Association.
- Working Group on Endourology of the German Society of Urology.
- Urological Research Society.
- Paracelsus Society in Salzburg.
- Hessian Cancer Society.
- Drug Safety Commission A, Federal Ministry of Health.
- European Association of Urology.
Photo of the doctor: (c) UKGM - Universitätsklinikum Gießen und Marburg GmbH
About hospital
The University Hospital Marburg UKGM offers patients modern diagnostics and comprehensive therapy at the international level. As a maximum care hospital, the medical facility specializes in all fields of modern medicine ranging from ophthalmology to traumatology and dentistry. The main areas of specialization of the hospital are surgery, neurosurgery, oncology, nephrology with kidney transplantation and children's medicine.
The hospital is the third largest in Germany. Every year, more than 436,000 patients are treated in two locations of the hospital (Giessen and Marburg): 342,000 in outpatient and 94,000 inpatient settings. The medical facility is the first privatized university hospital in the country.
The hospital staff makes a significant contribution to the development of research activities at the Faculty of Medicine of the Justus Liebig University Giessen and the Philipps University of Marburg. To develop new diagnostic and therapeutic methods, as well as to implement them into clinical practice, the specialists maintain active cooperation in a large number of areas.
The widest range of diagnostic and therapeutic services, the advanced infrastructure and technical base, high quality of treatment and professionalism of health workers contribute to the fact that the medical facility has an excellent reputation not only in Germany, but also far beyond its borders.
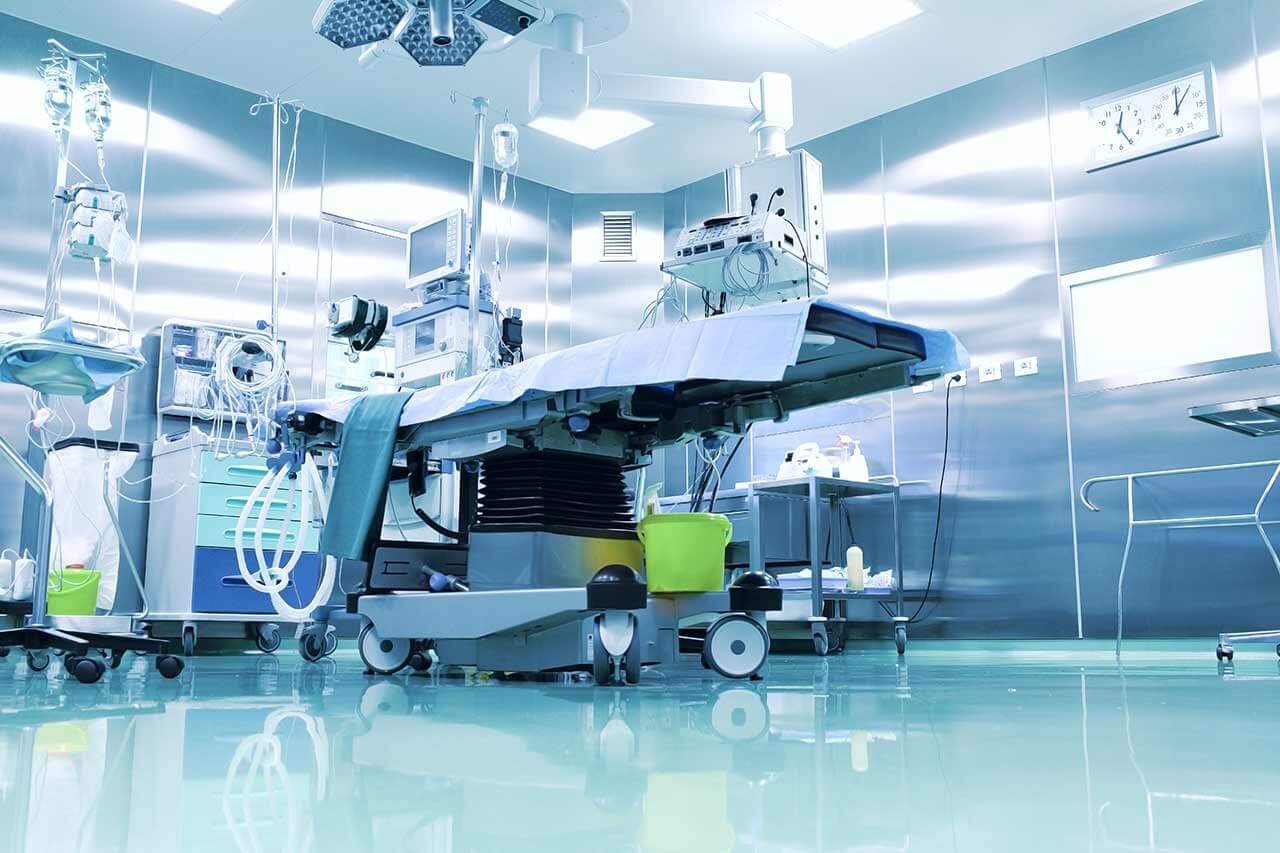
Photo: (c) depositphotos
Accommodation in hospital
Patients rooms
The patients of the University Hospital Marburg UKGM live in comfortable single and double rooms made in a modern design and light colors. Each room has an ensuite bathroom with shower and toilet. The pediatric departments provide patient rooms for the joint accommodation of mother and child. The standard room furnishing includes an automatically adjustable bed, bedside table, wardrobe, TV, telephone.
Meals and Menus
The patients of the hospital are offered balanced, healthy three meals a day: buffet breakfast, lunch and dinner. The private kitchen, certified according to DIN EN ISO 9001: 2000, is responsible for providing patients with food and drinks.
If for some reason you do not eat all foods, you will be offered an individual menu. The hospital also has a cafeteria with a large assortment of hot and cold drinks, snacks and desserts.
Further details
Standard rooms include:
Television
All patient rooms are equipped with TV sets. If you have some questions about TV use, please contact medical personnel.
Religion
Religious services can be provided upon request.
Accompanying person
During an inpatient program, an accompanying person can stay with you in a patient room or in a hotel of your choice.
Hotel
During the outpatient program, you can stay at the hotel of your choice. Our managers will help you choose the most suitable option.