The program includes:
- Initial presentation in the clinic
- clinical history taking
- review of medical records
- physical examination
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- TSH-basal, fT3, fT4
- tumor markers
- inflammation indicators (CRP, ESR)
- indicators of blood coagulation
- full course of the chemotherapy and radiation therapy
- nursing services
- consultations of related specialists
- explanation of individual treatment plan
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of previous laboratory tests and instrumental examinations. After that, you will undergo an additional examination, including complete blood count, laboratory assessment of liver and kidney function. Based on the received results, the physician will elaborate the chemotherapy regimen, conduct radiotherapy planning with the help of CT or MRI, make the permanent tattoo marks on the skin and conduct CT simulation in order to assess the accuracy of the rays and the radiation dose. If necessary, related medical specialists will be involved in the elaboration of a treatment regimen (tumor board).
Chemotherapy and radiation therapy are carried out as the day hospital procedure, without mandatory admission to the hospital. At each visit, the physician will assess your general condition and the marks on the skin. After that, you will be placed in a shielded radiation therapy room, on a special table.
Each radiation therapy session lasts less than half an hour (including preparation). All this time, doctors and nurses are monitoring your condition, you can communicate with them through a loudspeaker. The procedure is completely painless. Depending on the planned course of treatment, you will visit the hospital from 1 to 3-5 times a week.
During the chemotherapy session, after the placement of a venous catheter, you will stay in a comfortable ward. An infusion system will be connected to the catheter, through which the required drug or a drug combination will be administered. All drugs are administered by intravenous drip, slowly, so the total duration of the infusion can be up to several hours. All this time, doctors and nurses will monitor your health condition closely.
After the completion of the chemotherapy and radiation therapy course, you will undergo control examinations aimed at assessing your condition and efficacy of treatment. After that you will receive the medical report with detailed recommendations regarding further follow-up and treatment. In the future, you will be able to have a distant consultation with your attending physician and schedule the next course of treatment, if necessary.
Required documents
- Medical records
- MRI/CT scan (not older than 3 months)
- Biopsy results (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
According to the the Focus magazine, the Department of Radiation Therapy and Radiation Oncology at the University Hospital Jena ranks among the top German medical facilities specializing in radiation therapy!
The department offers all types of modern radiation therapy for the treatment of malignant neoplasms of various localization. The availability of the cutting-edge radiation therapy technologies, the close cooperation with the specialists from all related disciplines, as well as the experience and competence of doctors provide patients with the individualized treatment and the best therapy results. The department is also part of the Jena University Cancer Center, which employs outstanding professionals who are ready to provide medical care even in the most difficult clinical cases. The department is headed by Prof. Dr. med. Andrea Wittig.
During the radiation therapy, the same type of radiation is used as in the X-ray machine, but it is 50-100 times more powerful. Due to such a high power, the radiation penetrates into the body and reaches the tumor, while the superficial healthy tissues do not receive a large dose of radiation. Despite the fact that only a small amount of energy reaches the irradiated tissue, it is enough to destroy DNA. Consequently, the irradiated cell dies and cannot give rise to daughter cells. Thus, in the case of irradiation of a sufficient number of cancer cells, the tumor shrinks and may even disappear completely. The radiation therapy is divided into therapeutic and palliative one. Prior to radiation therapy, it is necessarily planned with the help of CT, followed by radiation and the subsequent patient care.
The service range of the department includes:
- Tomotherapy. It is a type of radiation therapy, in which the radiation is delivered to the tissues in layers. The tomotherapy device forms a combination of fan beam radiation with a radius of 360° with intensity modulation (IMRT) and megavolt CT (MVCT). Tomotherapy is a gold standard for targeted irradiation of complex tumors. During the therapy, the linear accelerator repeatedly rotates 360° around the patient, passing through the central opening of the system.This device allows the doctor to irradiate thousands of narrow single fields, which are individually optimized and aimed at the target tumor. This ensures the best possible distribution and homogeneity of the dose, while the load on healthy tissues is minimized.
- Intensity-modulated radiation therapy. This type of therapy has been used in the department since 2001. The department has long experience and holds leading positions in the application of this technique for the treatment of upper respiratory tract tumors, prostate and anal cancers, gynecologic oncopathologies. In the case of this therapy, the intensity of the radiation dose is "modulated", namely, various areas in the radiation field are irradiated with different intensity. In addition to better protection of the radiation-sensitive healthy tissue, which surrounds the tumor, this therapy also allows the doctor to increase the radiation dose in certain areas (integrated amplification).
- Stereotactic radiosurgery. This type of treatment is a unique high-precision irradiation of brain metastases. In many cases, the stereotactic interventions can help to avoid surgery, regardless of the tumor origin; in other cases, they complement traditional surgical treatment. In all cases, it is very important to accurately detect the localization of the pathological focus (mask, vacuum cushion, infrared positioning system), as well as the corresponding positional examination of the target area before each exposure. All this is provided thanks to the Conebeam CT system. During the rotation around the target area, the flat panel detector takes several 2D images, which are converted into a set of 3D images. These data are compared with the reference CT images, after which the position deviations are corrected.
- Gating. This therapy is a particularly sparing treatment method of lung cancer. The irradiation can be adapted to the respiratory movements using modern procedures in such a way as to minimize damage to healthy lung tissues. The therapy is carried out using 4D-CT, which allows the doctor to receive a section images in separate respiratory phases. With such information, a lung tumor can be irradiated only in specific respiratory phase. This type of therapy is an excellent alternative to open lung surgery, which is associated with serious surgical risks.
- Brachytherapy. In the case of this type of radiation therapy, the radiation source is inserted into the affected organ. Brachytherapy can be used in both therapeutic and palliative procedures, and can also be combined with radiation therapy on a linear accelerator (percutaneous radiation). There are such types of brachytherapy as intracavitary brachytherapy (for example, vaginal and uterine tumors), interstitial brachytherapy (for example, breast carcinoma, ENT tumors, lymph node metastases, anal tumors), superficial brachytherapy (for example, skin tumors), intrathecal tumors, anal tumors, superficial brachytherapy (for example, skin tumors), intraoperative brachytherapy (for example, sarcomas, recurrences of pelvic and thoracic wall tumors) and intraluminal brachytherapy (for example, esophageal or respiratory tract tumors).
- Irradiation using 4D-CT. Most often, this type of therapy is used in metastases and tumors of the lungs and liver. With the help of 4D-CT, the doctor can record the movement of organs during respiration, and then restore the exact location of the tumor for individual cycles of breathing.
- High-precision prostate irradiation. In many cases, such therapy is an alternative to surgery with equal long-term chances for recovery. The prostate irradiation is performed using a tomotherapy device. This allows the doctors to significantly increase the dose of radiation for the tumor compared to conventional methods, as well as better preserve healthy organs adjacent to it, such as the bladder and rectum. The gold "seeds" are previously implanted into the prostate gland for targeted irradiation of the tumor, regardless of the natural displacement of the prostate and the filling of the bladder and rectum. They are clearly visible in computed tomography and play the role of a specific tumor marker. Thus, before each irradiation, the prostate gland can be precisely positioned by imposing golden markers on each fraction using the original CT scan.
- Other types of radiation therapy
Curriculum vitae
Prof. Dr. med. Andrea Wittig holds the position of the Head of the Department of Radiation Therapy and Radiation Oncology at the University Hospital Jena. Dr. Wittig studied Human Medicine at the University of Essen, where she received Doctoral Degree and underwent a procedure of habilitation on ion-radiation therapy. After her board certification in radiation therapy in Germany and the Netherlands, she worked as a Senior Physician at the University Hospital Essen, and then held a position in the Department of Radiation Therapy and Radiation Oncology at the University Hospital Giessen and Marburg. Here she also received the title of Professor of Radiation Therapy (Philipps University of Marburg), and then she held a senior position at the University Hospital Giessen. While working in the international research organizations, Prof. Wittig always successfully combined fundamental researches and clinical practice. When she was a student, she worked on her own research project for one semester in the United States at the Brookhaven National Laboratory and then in research projects in the European Union.
Photo of the doctor: (c) Universitätsklinikum Jena
About hospital
According to the prestigious Focus magazine, the University Hospital Jena regularly ranks among the top German medical facilities!
The hospital has positioned itself as a multidisciplinary medical facility with a long history of more than 200 years. Since its foundation, the hospital has been constantly developing and modernizing, thanks to which nowadays it offers patients the highest level of treatment in Germany based on the use of innovative technologies and the very latest therapeutic techniques. The hospital consists of 26 specialized departments and 25 research institutes. It treats more than 53,600 inpatients and about 274,000 outpatients every year. The staff of the hospital includes more than 5,600 competent doctors.
The extensive resources of the university hospital, high treatment standards, and the introduction of new research developments provide first-class treatment in Germany meeting the stringent international standards. The hospital has an excellent reputation not only in Germany, but also far beyond its borders, due to which it accepts a large number of foreign patients for the diagnostics and treatment.
Despite the technical progress and the availability of accurate computerized systems, the patient’s physical health and emotional state is the main value of each employee of the hospital, since some diagnoses cause emotional distress in patients. The doctors of the hospital believe that the key to a successful result is a comprehensive and individual approach, so they spend a lot of time talking with patients, listen carefully to all their wishes and support at all stages of the therapeutic process. All this in combination with high-precision diagnostic techniques and the very latest types of therapy forms a solid basis for the achievement of an optimal treatment result.
Photo: (c) depositphotos
Accommodation in hospital
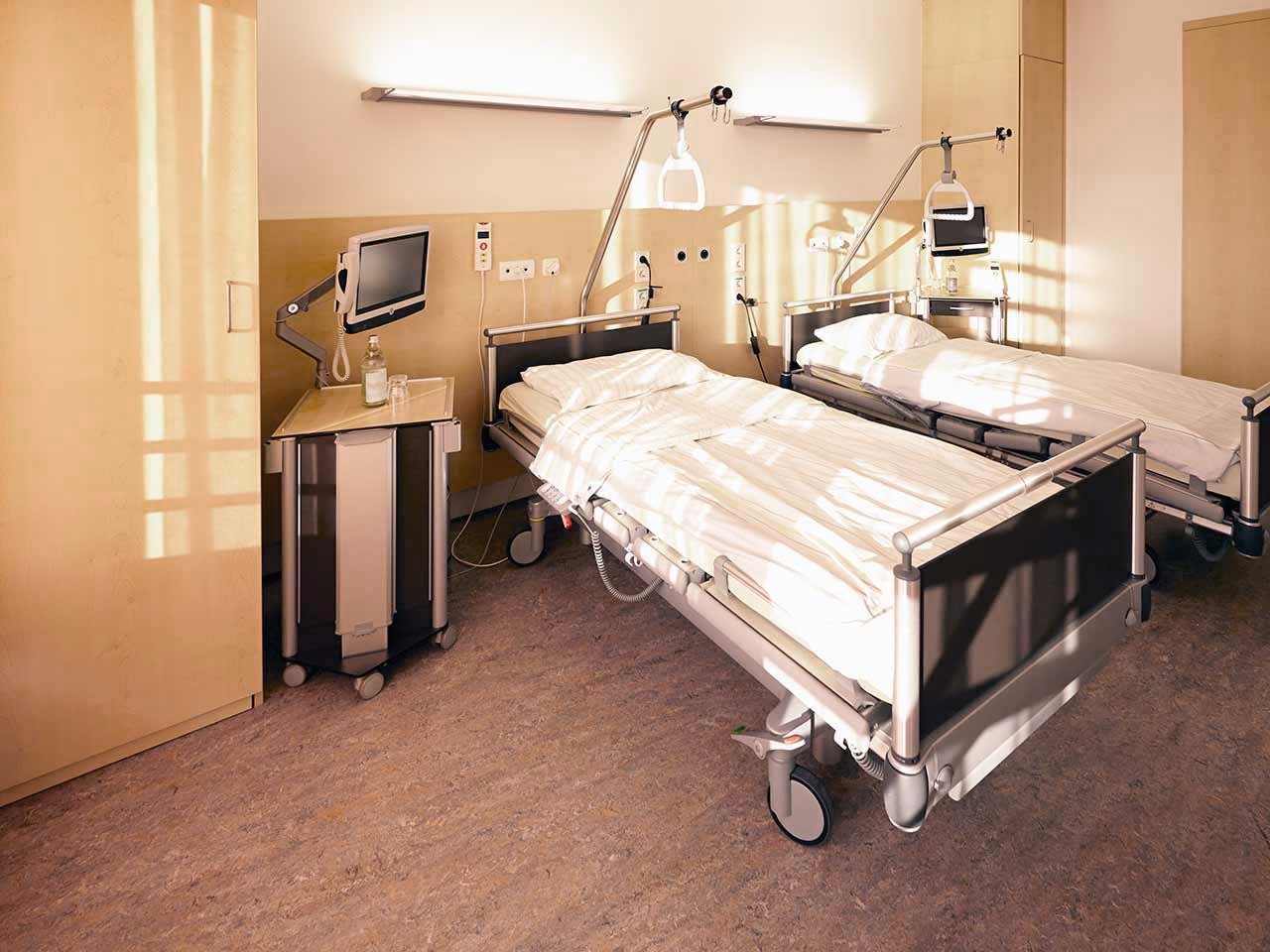
Patients rooms
The patients of the University Hospital Jena live in comfortable single and double rooms made in a modern design. Each patient room is equipped with an ensuite bathroom with shower and toilet. The room has enough space to store personal belongings, as well as a table and chairs for receiving visitors. A bedside table can be converted into a table so that patients can eat right in their bed. Each room has a TV, and there is also access to the Internet. In addition, the hospital offers enhanced-comfort rooms.
Meals and Menus
The patient and his accompanying person have a daily choice of three menus. If for some reason the patient does not eat all the foods, he will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to the treatment.
Further details
Standard rooms include:
Religion
Religious services are available upon request.
Accompanying person
During the inpatient program, an accompanying person may stay with you in a room or at the hotel of your choice.
Hotel
During the outpatient program, you can live at a hotel of your choice. Managers will help you to choose the most suitable options.