The program includes:
- Initial presentation in the hospital
- Clinical history taking
- Review of available medical records
- Physical examination
- Laboratory tests:
- Complete blood count
- General urine analysis
- Biochemical analysis of blood
- Tumor markers
- Inflammation indicators (CRP, ESR)
- Coagulogram
- Ultrasound scan
- CT scan / MRI
- Preoperative care
- Embolization or chemoembolization, 2 procedures
- Symptomatic treatment
- Cost of essential medicines
- Nursing services
- Elaboration of further recommendations
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examination, such as the assessment of liver and kidney function, ultrasound scan, CT scan and MRI. This will allow the doctor to determine which vessels are feeding the tumor and its metastases, as well as determine how well you will tolerate the procedure.
Chemoembolization begins with local anesthesia and catheterization of the femoral artery. The thin catheter is inserted through a few centimeters long incision of the blood vessel. The doctor gradually moves the catheter to the vessel feeding the primary tumor or its metastases. The procedure is carried out under visual control, an angiographic device is used for this. The vascular bed and the position of the catheter in it are displayed on the screen of the angiograph.
When the catheter reaches a suspected artery, a contrast agent is injected through it. Due to the introduction of the contrast agent, the doctor clearly sees the smallest vessels of the tumor and the surrounding healthy tissues on the screen of the angiograph. After that, he injects emboli into the tumor vessels through the same catheter.
Emboli are the spirals or the liquid microspheres. The type of embolus is selected individually, taking into account the diameter of the target vessel. When carrying out chemoembolization, a solution of a chemotherapy drug is additionally injected into the tumor vessel. Due to the subsequent closure of the vessel lumen with an embolus, the chemotherapy drug influences the tumor for a long time. In addition, the drug does not enter the systemic circulation, which allows doctors to use high doses of chemotherapeutic agents without the development of serious side effects. Chemoembolization leads to the destruction of the tumor or slowing down its progression.
After that, the catheter is removed from the artery. The doctor puts a vascular suture on the femoral artery and closes it with a sterile dressing. During chemoembolization, you will be awake. General anesthesia is not used, which significantly reduces the risks of the procedure and allows performing it on an outpatient basis, avoiding long hospital stay.
After the first procedure, you will stay under the supervision of an interventional oncologist and general practitioner. If necessary, you will receive symptomatic treatment. As a rule, a second chemoembolization procedure is performed in 3-5 days after the first one in order to consolidate the therapeutic effect. After that, you will receive recommendations for further follow-up and treatment.
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
According to the Focus magazine, the Department of Adult and Pediatric Urology at the University Hospital Jena ranks among the top German medical facilities specializing in prostate cancer treatment!
The department offers the full range of advanced methods of diagnostics and treatment of all genitourinary system diseases, including in children. Of particular interest is the treatment of patients with urinary tract and kidney tumors, kidney stone disease, prostate diseases, treatment of urinary incontinence, andrologic disorders and urological problems in young patients. Since 2010, the department has been certified as the Prostate Cancer Center (certified by the German Cancer Society, recertified in 2016). The Chief Physician of the department is Prof. Dr. med. Marc-Oliver Grimm.
In addition to standard treatment methods, the department offers the most advanced therapeutic options, for example, minimally invasive interventions using the da Vinci surgical systems, innovative laser technologies, including the Greenlight XPS laser. Since the department carries out productive research activities, there is a lot of clinical trials on the very latest drugs, which are available for all patients.
The inpatient service range of the department includes:
- Diagnostics and treatment of prostate cancer
- Laparoscopic radical prostatectomy using the da Vinci surgical system
- Open surgery to treat prostate cancer
- Drug therapy
- Treatment as part of clinical trials
- Diagnostics and treatment of andrological diseases
- Erectile dysfunction (impotence)
- Male infertility
- Fibroblastic induration of the penis (Peyronie's disease)
- Diagnostics and treatment of bladder tumors
- Diagnostics and treatment of urethral stricture
- Endoscopic interventions
- Urethral resection under imaging guidance (internal urethrotomy SACHSE) or without it (internal urethrotomy OTIS)
- Urethral dilation using bougienage (in exceptional cases)
- Open intervention
- Elimination of stenosis and the formation of a through urethral anastomosis (in short strictures)
- Urethral plastic surgery using oral mucosa tissues
- Endoscopic interventions
- Diagnostics and treatment of urolithiasis
- Diagnostics
- Ultrasound examinations
- X-ray examinations
- Blood and urine tests
- Therapy
- Extracorporeal shock wave lithotripsy (ESWL)
- Urethroscopy
- Percutaneous nephrolitholapaxy, also, using miniature instruments
- Laser lithotripsy
- Metaphylaxis
- Diagnostics
- Diagnostics and treatment of testicular tumors
- Retroperitoneal lymph node dissection (radical and nerve-preserving)
- Chemotherapy
- Radiation therapy
- Sperm cryoconservation for the preservation of fertility
- Diagnostics and treatment of urinary incontinence
- Diagnostics
- Analysis of the postvoid residual urine volume using ultrasound examination (in full bladder and after bladder emptying)
- Urodynamics ( bladder pressure measurement)
- Cystoscopy
- X-ray examinations
- Therapy
- Drug therapy (especially in imperative urinary incontinence)
- Physiotherapy (especially in stress urinary incontinence)
- Electrotherapy (especially in imperative and reflex incontinence)
- Surgical treatment (especially in stress urinary incontinence)
- Sling procedures
- Botulinum toxin injection therapy
- Neuromodulation
- Diagnostics
- Diagnostics and treatment of kidney cancer
- Radical surgery
- Minimally invasive surgery
- Chemotherapy
- Radiation therapy
- Hormone therapy
- Diagnostics and treatment of penile cancer
- Diagnostics and treatment of benign prostatic hyperplasia
- Laparoscopic interventions, including robot-assisted ones
- Radical prostate removal (prostatectomy)
- Radical / simple kidney removal (nephrectomy)
- Radical bladder removal (cystectomy)
- Partial kidney removal in oncopathology
- Adrenal gland removal
- Removal of lymph nodes in the pelvic region
- Fixation of the kidney in floating kidney syndrome
- Elimination of kidney stenosis (pyeloplasty)
- Colposacropexy
- Varicocele surgery
- Diagnostics and treatment of urological diseases in children
- Vesicoureteral reflux
- Undescended testicles
- Hypospadias
- Other diagnostic and therapeutic options
The outpatient service range of the department includes:
- Diagnostics
- Urinalysis, urinary cytology and fluorescent in situ hybridization (FISH test)
- Uroflowmetry
- Sonography (including Doppler and duplex ultrasonography)
- X-ray examinations (urinary tract imaging, excretory urography)
- Video urodynamics
- Cystoscopy
- Prostate biopsy (under local anesthesia)
- Spermogram
- Therapy
- Drug therapy in oncopathologies
- Urinary diversion (bladder catheterization, ureteral bypass surgery, and renal pelvis catheterization)
- Outpatient interventions
- Hydrocele treatment surgery
- Inguinal hernia surgery
- Surgeries to treat foreskin narrowing (circumcision, postioplasty in phimosis)
- Varicocele surgery
- Urine diversion
- Prostate biopsy (also MRI-guided)
- Other outpatient services
Curriculum vitae
Prof. Dr. med. Marc-Oliver Grimm is the Head of the Department of Adult and Pediatric Urology at the University Hospital Jena. Prior to this, he worked as a Senior Physician at the University Hospital Dresden for four years. He also held a position at the University Hospital Duesseldorf for several years. His priority is prostate cancer treatment. While working at the University Hospital Dresden, he successfully founded the Prostate Cancer Center, which was certified as one of the best in Germany. He was also a member of the steering group and lead author of separate chapters of the prostate cancer treatment guideline.
Photo of the doctor: (c) Universitätsklinikum Jena
About hospital
According to the prestigious Focus magazine, the University Hospital Jena regularly ranks among the top German medical facilities!
The hospital has positioned itself as a multidisciplinary medical facility with a long history of more than 200 years. Since its foundation, the hospital has been constantly developing and modernizing, thanks to which nowadays it offers patients the highest level of treatment in Germany based on the use of innovative technologies and the very latest therapeutic techniques. The hospital consists of 26 specialized departments and 25 research institutes. It treats more than 53,600 inpatients and about 274,000 outpatients every year. The staff of the hospital includes more than 5,600 competent doctors.
The extensive resources of the university hospital, high treatment standards, and the introduction of new research developments provide first-class treatment in Germany meeting the stringent international standards. The hospital has an excellent reputation not only in Germany, but also far beyond its borders, due to which it accepts a large number of foreign patients for the diagnostics and treatment.
Despite the technical progress and the availability of accurate computerized systems, the patient’s physical health and emotional state is the main value of each employee of the hospital, since some diagnoses cause emotional distress in patients. The doctors of the hospital believe that the key to a successful result is a comprehensive and individual approach, so they spend a lot of time talking with patients, listen carefully to all their wishes and support at all stages of the therapeutic process. All this in combination with high-precision diagnostic techniques and the very latest types of therapy forms a solid basis for the achievement of an optimal treatment result.
Photo: (c) depositphotos
Accommodation in hospital
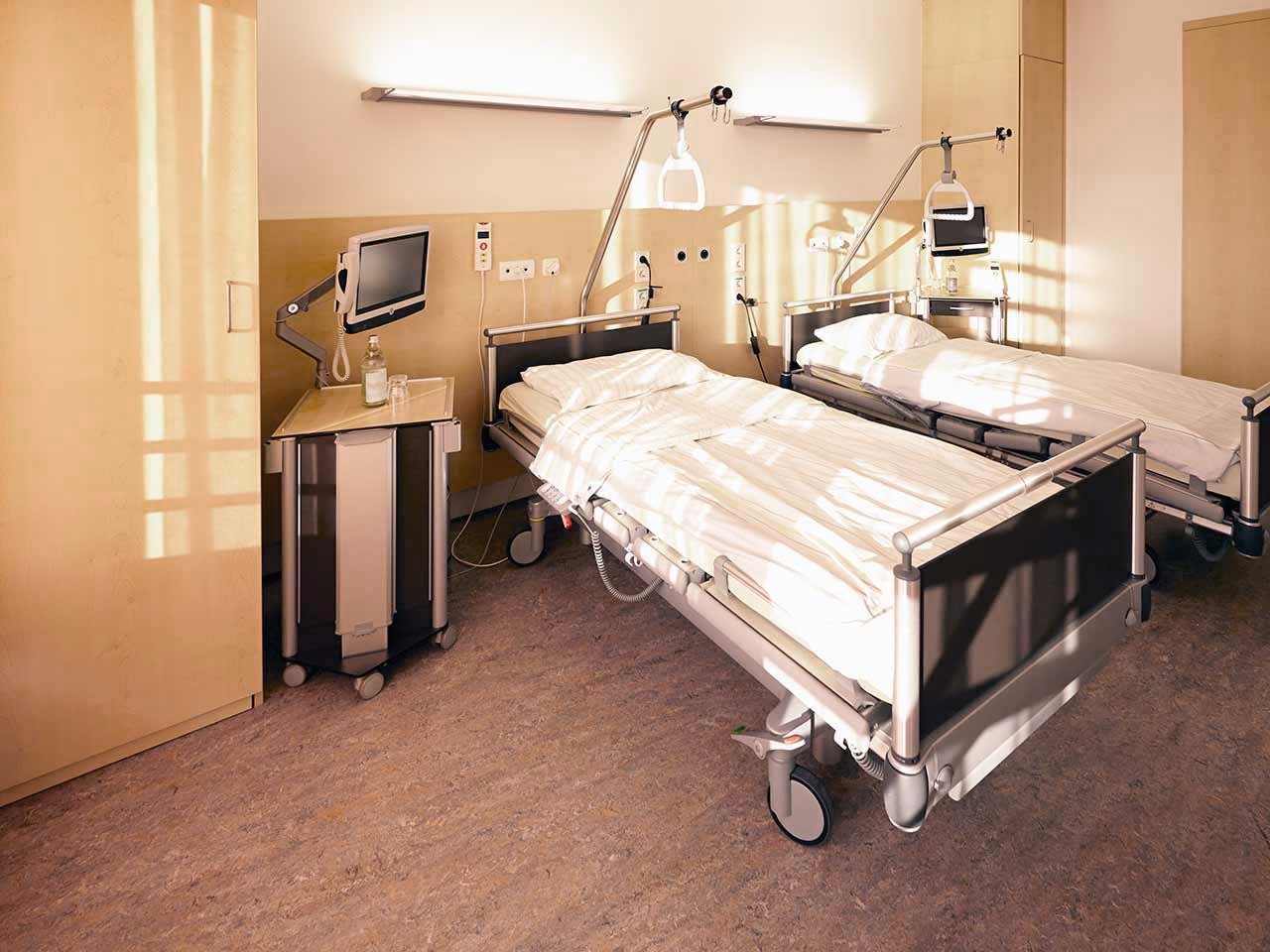
Patients rooms
The patients of the University Hospital Jena live in comfortable single and double rooms made in a modern design. Each patient room is equipped with an ensuite bathroom with shower and toilet. The room has enough space to store personal belongings, as well as a table and chairs for receiving visitors. A bedside table can be converted into a table so that patients can eat right in their bed. Each room has a TV, and there is also access to the Internet. In addition, the hospital offers enhanced-comfort rooms.
Meals and Menus
The patient and his accompanying person have a daily choice of three menus. If for some reason the patient does not eat all the foods, he will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to the treatment.
Further details
Standard rooms include:
Religion
Religious services are available upon request.
Accompanying person
During the inpatient program, an accompanying person may stay with you in a room or at the hotel of your choice.
Hotel
During the outpatient program, you can live at a hotel of your choice. Managers will help you to choose the most suitable options.