The program includes:
- Initial presentation in the clinic
- Clinical history taking
- Physical examination
- Review of medical records
- Laboratory tests:
- Complete blood count
- General urine analysis
- Biochemical blood test (kidney and liver function tests)
- Indicators of inflammation (CRP, ESR)
- Indicators of blood coagulation
- Immunohistochemical and genetic analysis of tumor cells (if indicated)
- Leukapheresis, processing of T-cells and cultivation of CAR T-cells
- Adjuvant chemotherapy
- Infusion of modified CAR T-cells to a patient
- Control examinations
- Cost of essential medicines and materials
- Nursing services
- Full hospital accommodation
- Explanation of future recommendations
Indications
- Acute myeloid leukemia (AML) that is resistant to the conventional therapy
How program is carried out
Days 1-2. Initial presentation at the clinic. The doctor collects the patient's medical history, looks at his medical records and previous examinations. Special attention is paid to previous cancer treatments and their results, since CAR T-cell therapy is indicated only if the conventional treatment protocols are ineffective. Based on the results of the consultation, the doctor administers the examination, which includes a complete blood count with white blood cell count, assessment of liver and kidney function, immunohistochemical and genetic analysis of tumor cells (if indicated) and other studies.
Day 3. Collecting patient’s blood. During the leukapheresis procedure, doctors harvest at least 100 million T-cells, which will subsequently undergo gene modification. If there are certain clinical reasons, and the patient needs to postpone the subsequent stages of CAR T-cell therapy, the harvested T-cells undergo the procedure of cryoconservation. If the patient is able to continue treatment immediately, then the harvested T-cells are transferred to the laboratory.
Days 4-12. Processing and gene modification of the T-cells pool lasts 7-10 days. During this time, the patient is receiving immunosuppressive chemotherapy drugs. The chemotherapy is aimed at suppressing the patient's own immune system, which will allow CAR T-cells to fight the tumor more effectively.
Day 13. Manufactured CAR T-cells are tested for the microbiological safety and functional activity. After the successful testing completion, the solution with CAR T-cells is administered to the patient intravenously.
Day 14 and other days. Control examination and further medical supervision in the hospital are carried out. If there are no side effects of CAR T-cell therapy, a stable tendency towards normalization of blood count is observed and the patient has stable general health condition, the patient is discharged from the hospital. Before the discharge, the patient receives the detailed recommendations for further follow-up during the disease remission.
Required documents
- Complete blood count with white blood cell count
- Biochemical blood test (renal and liver function tests), if available
- Bone marrow biopsy results
- CT scan, if available
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
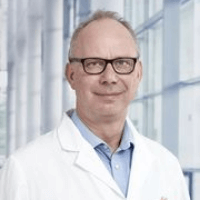
The Department of Pediatric Oncology and Hematology at the University Hospital Ulm provides the full range of medical services in the areas of its specialization. The highly qualified doctors at the medical facility diagnose and treat solid malignant tumors in children, such as brain tumors, neuroblastomas, nephroblastomas, Ewing's sarcomas, osteosarcomas, and soft tissue sarcomas. The department also provides medical care to young patients with malignant blood diseases. Of particular interest is the treatment of leukemia and myelodysplastic syndrome. Medical services are provided in strict accordance with the current clinical protocols and recommendations of the German Society of Pediatric Oncology (GPO). The most effective, proven therapeutic methods are used in clinical practice to achieve long-term results. The department's specialists most often perform chemotherapy and immunotherapy. Autologous bone marrow transplants can also be carried out if clinically indicated. The procedure is performed in a specialized center at the University Hospital Ulm. When treating young patients, the department's oncologists collaborate closely with pediatric surgeons, neurosurgeons, radiation therapists, orthopedists, and other experts. The department has 20 beds available for the hospitalization of children. The department is headed by Prof. Dr. med. Holger Cario.
Brain tumors are the most common malignant solid neoplasms in childhood. The department's team of pediatric oncologists treats young patients with gliomas, medulloblastomas, and ependymomas. The specialists also deal with the management of benign brain tumors, including craniopharyngiomas, meningiomas, and neurocytomas. Tumor growth often leads to increased intracranial pressure, resulting in various unpleasant symptoms in children, such as constant headaches, nausea and vomiting, coordination and gait abnormalities, visual impairment, seizures, etc. The main method of detecting malignant brain tumors is magnetic resonance imaging. The doctors also conduct a physical examination, an assessment of the child's neurological status, laboratory tests, and a biopsy with a follow-up histological examination. The first-line treatment for detected brain tumors is surgery. The surgical intervention is usually supplemented with conservative methods. Pediatric oncologists carry out chemotherapy, targeted therapy, and immunotherapy. Radiation therapy may also be performed if clinically indicated. After the completion of the basic course of treatment, neurological rehabilitation may be required. This is aimed at restoring speech, motor functions, and cognitive abilities. The treatment regimen for brain cancer is developed individually for each child. Such an approach allows the doctors to achieve the best results and eliminate neurological deficits.
The department's clinical focus is the treatment of leukemias, malignant diseases of the hematopoietic system. The main symptoms of this group of diseases include general weakness, fatigue, loss of appetite, fever of unknown origin, immunodeficiency, and symptoms of intoxication. The diagnosis involves a physical examination, extensive laboratory testing, and a bone marrow aspiration (a painless procedure performed under anesthesia). In some cases, imaging examinations such as CT, MRI, ultrasound, and X-ray scans may also be prescribed. With all the diagnostic data, the department's oncologists proceed with the development of the optimal treatment regimen. An individually prescribed course of chemotherapy is mainly carried out to treat leukemia in children. Depending on the particular clinical case, oral or intravenous administration of chemotherapeutic agents is supplemented with targeted therapy and/or radiation therapy. The last-line treatment for leukemia is high-dose chemotherapy followed by a bone marrow transplant. This treatment option is indicated for young patients with a complex course of the disease.
The medical facility also successfully treats myelodysplastic syndromes, which lead to impaired blood cell maturation. Children with this pathology suffer from weakness and fatigue, fever, pale skin, and an increased tendency to bleed. To confirm the diagnosis, the department's pediatric oncologists perform general and biochemical blood tests and a bone marrow puncture. If clinically indicated, genetic tests and imaging examinations may also be required. Treatment tactics depend on the aggressiveness of the disease. In cases of myelodysplastic syndrome with low aggressiveness, the department's specialists carry out chemotherapy in combination with immunosuppressive therapy. In cases of high aggressiveness of the hematologic pathology, effective results can be achieved through chemotherapy and a bone marrow transplant.
The department specializes in the treatment of the following diseases:
- Solid tumors of various locations
- Brain tumors
- Malignant tumors: gliomas, medulloblastomas, and ependymomas
- Benign tumors: craniopharyngiomas, meningiomas, and neurocytomas
- Neuroblastomas
- Nephroblastomas
- Ewing's sarcomas
- Osteosarcomas
- Soft tissue sarcomas
- Brain tumors
- Hematopoietic disorders
- Leukemia
- Myelodysplastic syndromes
- Other diseases
The department's range of diagnostic and therapeutic services includes the following:
- Diagnostic services
- Morphological and immunological examinations of blood, bone marrow, and tumor tissue
- Molecular analysis of blood, bone marrow, and tumor tissue
- Bone marrow puncture with a cytological examination
- Therapeutic services
- Chemotherapy
- Immunotherapy
- Bone marrow transplant
- Other medical services
Curriculum vitae
Higher Education and Professional Career
- 1987- 1994 Medical studies, Faculty of Medicine, Humboldt University of Berlin.
- 1994 Thesis defense, Faculty of Medicine, Humboldt University of Berlin.
- 1995 Internship and Residency, Department of Pediatric and Adolescent Medicine, University Hospital Ulm.
- 2001 Board certification in Pediatric and Adolescent Medicine.
- 2006 Board certification in Pediatric Hematology and Oncology.
- Since 2009 Senior Physician, Department of Pediatric Oncology and Hematology, University Hospital Ulm.
- 2009 Habilitation. Subject: "Molecular basis and clinical manifestations of congenital erythrocytosis and polycythemia in childhood and adolescence."
- 2012 Extraordinary Professorship.
Clinical and Research Focuses
- Anemias, in particular thalassemia, and other congenital and acquired anemias.
- Congenital and acquired erythrocytosis and related pathologies.
Photo of the doctor: (c) Universitätsklinikum Ulm
About hospital
The University Hospital Ulm is an advanced medical complex that provides patients with high-class medical care using the very latest scientific achievements. The medical facility has been performing successful clinical activities for more than 40 years and has long earned an excellent reputation throughout Europe. The hospital regularly demonstrates high treatment success rates, takes an active part in the training of medical students, and works tirelessly on promising research projects.
The university hospital consists of 29 specialized departments and 16 scientific institutes, where more than 7,000 highly qualified employees work for the benefit of their patients. More than 55,000 inpatients and about 300,000 outpatients are treated here every year. The hospital has 1,274 beds. The medical team of the hospital is focused on providing personalized medical services using the most modern and sparing diagnostic and treatment methods.
The University Hospital Ulm is the largest medical complex in the region, and practically all areas of modern medicine are represented here. Transplantology and oncology are among the priority areas of clinical activity in the medical facility. The hospital holds leading positions in the world in bone marrow transplantation. In addition, the hospital has advanced experience in cancer treatment. The Comprehensive Cancer Center is recognized as the leading facility of this kind in the country, and it is certified by the German Cancer Society (DKG). It provides effective treatment for various types of cancer. The center also offers innovative CAR T-cell therapy. In addition, the Cancer Center is actively engaged in research activities to improve available treatment methods and develop innovative therapeutic techniques to fight cancer.
Along with the use of advanced technologies, doctors show respect, understanding, and a humane attitude toward the patient. The medical team includes competent psychologists, who are always ready to provide assistance and support to the patients and their families during the therapeutic process.
Photo: (с) depositphotos
Accommodation in hospital
Patients rooms
The patients of the University Hospital Ulm live in comfortable single and double rooms with a modern design and light colors. All patient rooms have an ensuite bathroom with a toilet and a shower. The patient room furnishings include a comfortable automatically adjustable bed, a bedside table, a wardrobe, a table and chairs, a telephone, a radio, and a TV. Wi-Fi access is also available in patient rooms.
The hospital also offers enhanced-comfort rooms, which additionally have a safe, a refrigerator, and upholstered furniture. The bathroom in the enhanced-comfort room has changeable towels, a cosmetic mirror, a hairdryer, and toiletries.
Meals and Menus
Patients and their accompanying person are offered three meals a day: breakfast, lunch, and dinner. The patient and accompanying person have a choice of three menus every day, including a vegetarian menu. Patients staying in the enhanced-comfort rooms are also offered light snacks, fruits, desserts, and hot and cold drinks in the comfortable lounge area.
If, for some reason, you do not eat all the foods, you will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to treatment.
Further details
Standard rooms include:
![]() Shower
Shower
![]() Toilet
Toilet
![]() Wi-Fi
Wi-Fi
![]() TV
TV
Religion
The hospital has a chapel where Catholic and Protestant services are held weekly. The services are also broadcast on the internal television channel of the hospital. The chapel is open 24 hours a day for visits and prayers.
The services of other religious representatives are available upon request.
Accompanying person
Your accompanying person may stay with you in your patient room or at the hotel of your choice during the inpatient program.
Hotel
You may stay at the hotel of your choice during the outpatient program. Our managers will support you for selecting the best option.