A pancreatic pseudocyst is an accumulation of fluid near this organ that develops as a result of acute or chronic pancreatitis. Unlike a true cyst, its wall is non-epithelialized and consists of fibrous and granulation tissue. The disease causes abdominal pain, nausea, and vomiting. The diagnostics of this condition is carried out using ultrasound, CT scans, and endoscopic methods such as ERCP and endoscopic oral pancreatoscopy (POPS). The pathology can be cured with surgery or a minimally invasive procedure. You can undergo your treatment of pancreatic pseudocyst in Germany so that it is safe, non-traumatic, and effective.
Content
- Treatment options
- Endoscopic drainage
- Surgical drainage
- Percutaneous drainage
Endoscopic procedures are usually used because they are safer than open surgery and do not require a long recovery period. Surgical interventions are less often performed, and percutaneous procedures are very rarely used.
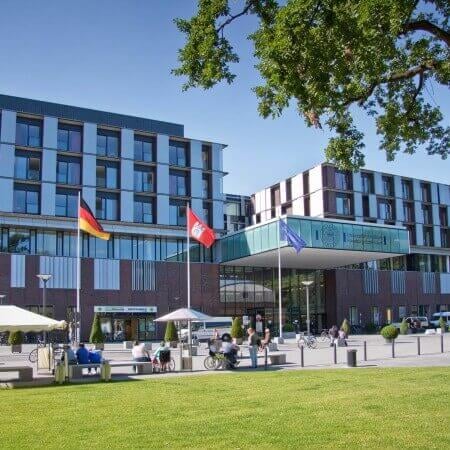
You can undergo your treatment in one of the following hospitals: University Hospital of Ludwig Maximilian University of Munich, University Hospital Duesseldorf, or University Hospital Ulm.
The Booking Health company will take care of the organization of your trip. Our specialists will help you to choose a specialized clinic and a doctor, make an appointment on the preferred date, help you to collect the necessary medical documents and get a visa, and take care of your flights and transfers. The Booking Health doctors will control the treatment process, and the company's coordinators will help you with any medical or organizational issues.
Treatment options
Cysts rarely disappear on their own. At the same time, they cause symptoms, reducing a patient's quality of life and may provoke severe complications. Therefore, most patients require invasive treatment, including surgery. Here are some arguments for its necessity:
- the presence of multiple cysts;
- location near the tail of the pancreas;
- concomitant strictures or calcifications of the pancreatic ducts;
- a progressive increase in the size of a pseudocyst.
Some patients require emergency surgical treatment. This is performed for acute complications of the pseudocyst such as infection, peritonitis, bleeding, or gastric obstruction.
Surgeons perform three types of invasive interventions for pseudocysts. These are percutaneous, endoscopic, and surgical drainage or resection. Ideally, any intervention is performed 6 weeks or more after acute pancreatitis to allow the pseudocyst wall to mature. However, pseudocysts of any size and maturity are treated immediately if they are expected to be a source of severe complications in the near future.
Endoscopic drainage
Endoscopic pseudocyst drainage is considered a first-line treatment in Germany because it is the safest and least traumatic option. The procedure is performed without any abdominal incisions or punctures but through the oral cavity. There are two types of endoscopic drainage, namely transpapillary and transmural. In any case, the goal of the intervention is to create a channel for the outflow of the contents of the pseudocyst into the gastrointestinal tract.
Transpapillary drainage is performed through the major duodenal papilla, the place where the pancreatic duct opens into the intestine. This procedure can be used if:
- there is a communicating tract between the pseudocyst and the main pancreatic duct;
- the pseudocyst is located far from the gastrointestinal tract, making transmural drainage a challenging task.
During the procedure, a catheter is inserted through the pancreatic duct, and a stent is placed in the connecting tract between the pseudocyst and the lumen of the duct under the guidance of ERCP. If the duct is scarred, it may be expanded with an inflatable balloon before stent placement. The main advantage of the transpapillary method is the ability to eliminate strictures in other ducts, which reduces the risk of additional pseudocysts. The effectiveness of the procedure is 81%, and in the best specialized centers in Germany it reaches 94%.
Transmural drainage is carried out through the wall of the stomach or duodenum under the guidance of endoscopic ultrasound or a conventional endoscope. Doctors in Germany prefer to use the ultrasound method for guidance as it allows them to get a safe approach even to a pseudocyst that is not adjacent to the wall of the gastrointestinal tract, as well as masses with a distal location. The procedure also reduces the risk of bleeding due to vascular damage.
During the procedure, a doctor determines the puncture site using endoscopy, inserts a needle into the pseudocyst, and then controls its location using X-ray scans. This place is then dilated and several stents are placed. If the procedure is performed without ultrasound guidance, technical success is achieved in 59% of cases. When using endosonography, the procedure is successful in 95% of cases, with a lower risk of complications (perforation, bleeding, and infection).
Surgical drainage
Open surgery is historically the very first treatment for pancreatic pseudocysts, but it is almost never used in Germany. Surgical drainage is performed only in special situations, namely in the case of technical failure of the endoscopic procedure, a recurrent pseudocyst, or if a malignant process is suspected.
When performing the operation, a doctor forms a channel through which the pseudocyst communicates with the stomach, duodenum, or jejunum.
Even so, this type of treatment in Germany is less invasive compared to the standard technique. Surgical drainage in German hospitals is performed laparoscopically (through short abdominal incisions). The operation is successful in more than 98% of patients, and the risk of cyst recurrence does not exceed 2.5%.
Percutaneous drainage
Percutaneous pseudocyst drainage is a rarely used procedure. This may be performed if the operation is contraindicated due to the high risk of complications.
Doctors in Germany perform this minimally invasive procedure under CT or ultrasound guidance. Through a skin puncture in the abdomen with a needle, a specialist inserts a stent into the pseudocyst.
The advantages of the method are a low risk of complications, a fast rehabilitation, and the possibility of carrying out the procedure in a short time after pancreatitis. Nonetheless, there are more disadvantages, so the procedure is considered a third-line treatment option after endoscopic and surgical methods. The stent is often clogged, so doctors have to change its position, which causes discomfort for a patient. The method is not applicable in the presence of pancreatic duct strictures.
You are welcome to use the Booking Health website to find the cost of medical services in different clinics in Germany and make your treatment appointment at the best price. Our company's employees will help to organize your trip abroad.
Authors:
The article was edited by medical experts, board-certified doctors Dr. Vadim Zhiliuk and Dr. Sergey Pashchenko. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Sources:
Verywell Health
MedlinePlus