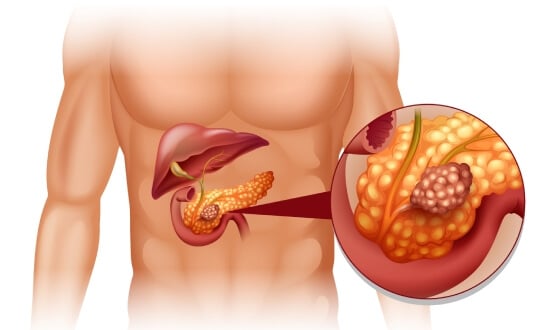
Pancreatic cancer (PanCa) is a dangerous illness with a severe clinical course and a typically negative prognosis. It is known to have one of the lowest 5-year survival rates, around 7% [1]. The majority of patients are diagnosed at advanced stages and die within a year after the diagnosis.
Stage 4 pancreatic cancer is extremely difficult to manage due to the tumor's specific features and chemoresistance. As a result, 5-year survival rates at this stage rarely exceed 5%. This underscores the need for novel treatment approaches, which has led to extensive research and the implementation of advanced therapies in clinical practice. This guide provides an extensive review of both conventional treatment methods and innovative therapies for the management of stage IV pancreatic cancer.
Conventional Treatment for Metastatic Pancreatic Cancer (mPC)
The treatment of stage 4 pancreatic cancer is very challenging due to the nature of the malignant tissue itself because it stimulates the development of specific fibrous tissue. This fibrous matrix "deceives" the patient's immune system and does not allow for easy penetration of drugs. Above that, at this stage, malignant cells have already disseminated to other distant organs, which typically excludes surgical resection of the tumor [2]. Consequently, chemotherapy is the number one option for stage 4 pancreatic cancer. Both monotherapy and combined therapy can be used at this stage, with the exact combination depending on the patient's ECOG performance status (Toxicity And Response Criteria Of The Eastern Cooperative Oncology Group) [3] and bilirubin levels.
Molecular and genetic testing are highly recommended because they allow for additional treatment options for stage 4 pancreatic cancer, such as chemoradiation for BRCA1/2 or PALB2-positive patients [4]. At this stage, palliative therapy and pain management become priorities alongside systemic treatments. Patients with duodenal or biliary obstruction may benefit from stent placement. However, none of these methods provide substantial survival benefits or significant improvements of desired daily living. Therefore, there is an urgent need for new treatments for pancreatic cancer stage 4.
Novel Ways to Manage Stage 4 Pancreatic Cancer
The need for innovative therapies for stage 4 pancreas cancer is evident, which is why several novel methods are gaining traction. Modern treatments for pancreatic cancer are now represented by minimally invasive procedures such as transarterial chemoembolization, ablation, dendritic cell therapy, and hyperthermia.
Percutaneous Ablation in Stage 4 Pancreatic Cancer
Thermal ablation techniques, specifically radiofrequency ablation (RFA) and microwave ablation (MWA), are being increasingly recognized as adjunctive treatments for stage 4 pancreas cancer treatment. Both of the methods use high temperatures to precisely target and destroy tumor tissue, opening new doors for patients who are not candidates for surgery.
Radiofrequency ablation is a minimally invasive technique that delivers electric-driven heat energy to the tumor site [5]. When inserted into the tumor, the electrodes cause local tissue necrosis and subsequent decrease of the tumor mass. Although RFA is not a standard option in clinical oncology guidelines, this procedure has demonstrated encouraging results in stage 4 pancreas cancer treatment. Studies report significant tumor regression of up to 80% among patients with unresectable pancreatic cancer. In addition, RFA proved to increase overall survival rates, especially when accompanied by standard systemic therapy. Because it is well tolerated by patients and has a good safety profile, RFA is a preferred option for treating unresectable tumors.
Microwave ablation is another thermal ablation method, which is increasingly used among stage 4 pancreatic cancer treatments. Recent prospective studies report radiologic tumor control and local response rates ranging from 60% to 75% within 6 to 12 months of treatment. In addition to tumor suppression, MWA has proven to be an irreplaceable tool for managing palliative symptoms, such as intractable abdominal pain. Therefore, MWA may suggest a positive impact on the quality of life.
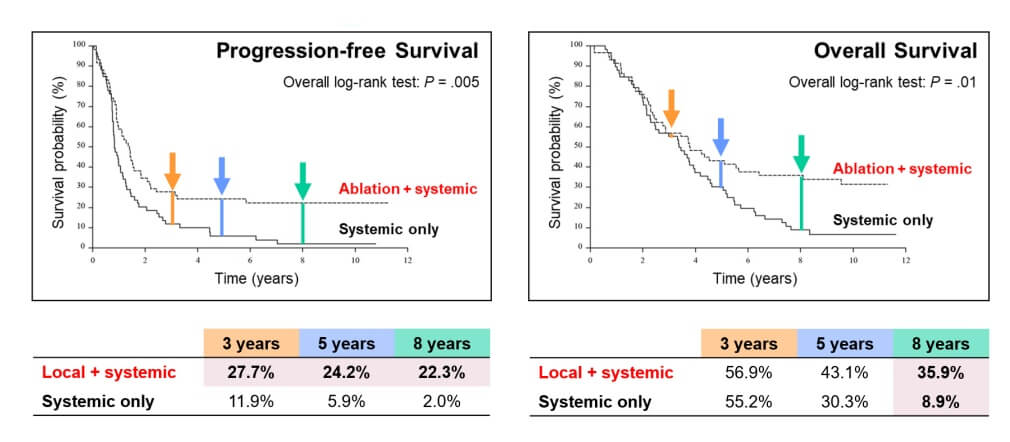
Cryoablation is an alternative modality that uses extreme cold to induce tumor necrosis via intracellular ice formation. It has also gained traction among 4 stage pancreatic cancer treatment options, especially for tumors located near critical anatomical structures, such as the portal vein. Its ability to preserve surrounding tissue makes it invaluable in complex anatomical regions. Recent data suggest a progression-free survival rate of approximately 66% at six months for patients with unresectable pancreatic cancer following cryoablation. Moreover, cryoablation has been used effectively in select cases of metastatic pancreatic ductal adenocarcinoma, particularly when surgical intervention is contraindicated. Cryoablation is generally well tolerated and shows a low incidence of complications, such as postoperative pain or indigestion.
Electrochemotherapy (ECT) treatment for pancreatic cancer stage 4
Reversible electroporation – the foundation of electrochemotherapy – transforms how medications penetrate cancer cells. Brief electrical pulses create temporary membrane pores, allowing chemotherapeutic agents to flood inside at concentrations impossible through standard delivery. For pancreatic tumors stage 4 notorious for treatment resistance, this represents a critical breakthrough.
Clinical data reveals impressive outcomes. Early-phase trials report response rates up to 65% in recurrent pancreatic malignancies – particularly those with high vascular involvement. Prof. Aigner's extensive experience demonstrates even more dramatic results: an 80% tumor reduction achieved within days in certain cases. The technique proves especially effective when tumors invade surrounding structures, making surgical removal impossible. [8]
The procedure itself involves precise electrode placement around the tumor's perimeter under general anesthesia. Needle spacing of 2.5-3 centimeters creates overlapping electrical fields while computer systems coordinate pulse delivery with cardiac rhythm – preventing any interference with heart function. Treatment typically requires two sessions spaced three weeks apart, with imaging assessment between procedures.
What sets ECT apart? In addition to direct cytotoxic effects, the electrical pulses trigger immunogenic cell death – this releases tumor antigens and activates the immune system. Dual mechanism has substantial advantages when combined with immunotherapy protocols, particularly crucial for metastatic disease where systemic immune activation matters most.
Patients should understand that the cost of electrochemotherapy varies significantly by institution and geographic location. When evaluating electrochemotherapy cost, consider that electro-chemotherapy may achieve tumor control in chemotherapy-resistant cases – potentially reducing overall treatment expenses and preserving quality of life.
Electrochemotherapy Explained: Why This "New Kid on the Block" is Changing Cancer Treatment
Transarterial Chemoembolization (TACE) in Stage 4 Pancreatic Cancer
Transarterial chemoembolization, or TACE, is an innovative treatment method that enables the targeted delivery of chemotherapeutic agents while simultaneously cutting off the tumor's blood supply to enhance the therapeutic effect. For stage four pancreatic cancer, TACE is considered as an adjuvant and palliative treatment option [6]. Above all, it is the best treatment for pancreatic cancer stage 4, which is especially effective for those with liver metastases. Studies with drug-eluting beads, which extend local release of chemotherapeutic agents into the tumor tissue, showed that TACE improves local disease control by up to 70%. In addition, progression-free time also extended for up to 12 months. TACE is known to offer a survival benefit, with more than 80% of patients living more than 1 year. Regional chemotherapy delivery avoids systemic exposure and high toxicity, which is crucial for fragile patients. If you are eager to find out more about this innovative procedure, including how it is performed, what are the contraindications, and what to expect after it, please watch an interview with Prof. Attila Kovács.
Prof. Kovács: When to Use DEB-TACE, Conventional TACE, or Radioembolization (TARE)
Regional chemotherapy in the treatment of advanced pancreatic cancer
Advanced pancreatic cancer demands radical solutions. When tumors spread beyond surgical reach – stage IV disease affecting 280 patients in Prof. Aigner's comprehensive study – regional chemotherapy offers hope where conventional approaches fail. [8]
The regional chemotherapy treatment for stage 4 pancreatic cancer bypasses the fundamental limitation of systemic treatment: drug dilution. Standard chemotherapy disperses medications through 5-7 liters of blood before reaching the tumor. Regional delivery achieves the opposite – concentrations of 60,000 ng/mL directly at the cancer site while keeping systemic exposure remarkably low.
Two approaches exist for advanced disease. Intra-arterial infusion via celiac axis catheters represents the foundational method, delivering concentrated medications through precisely positioned catheters over four consecutive days. The more intensive isolated upper abdominal perfusion with chemofiltration (UAP-F) takes this further – balloon catheters temporarily isolate the entire upper abdomen, creating a closed circuit where medications reach maximum potency before 45-minute blood filtration removes remaining drugs.
Stage IV results with this novel treatment for stage 4 pancreatic cancer speak volumes. Patients receiving UAP-F achieved 8.7 months median survival versus 6.6 months with standard arterial infusion. One-year survival? 37% with UAP-F compared to just 20.3% with conventional regional delivery. Even at three years, 7.7% of UAP-F patients remained alive. The technique also resolved severe ascites in 33 of 36 cases – providing immediate symptom relief alongside survival benefits. [8]
Toxicity stayed minimal throughout – predominantly WHO grades I-II, with serious side effects occurring only in heavily pretreated patients. Prof. Aigner discusses his pioneering experience with these techniques in the interview that follows.
Dendritic Cell Vaccination in Stage 4 Pancreatic Cancer
Dendritic cell therapy represents a cutting-edge advancement in immunotherapy. According to some reports, it is the best treatment for stage 4 pancreatic cancer. Dendritic cell therapy is a form of personalized therapy, which harnesses the body's immune defense mechanisms through dendritic cells. As immune "scouts," dendritic cells detect abnormal cells and orchestrate the activation of immune killers by recognizing and presenting the abnormal cells to them.
Dendritic cell therapy is gaining traction in treating the fourth stage of pancreatic cancer. Clinical data suggest that this therapy leads to the stabilization of the disease in up to 50% of patients alongside notable improvements in symptom management, including reduced fatigue, improved appetite, and alleviated pain. Dendritic cell therapy has a favorable safety profile with few to no side effects, making it a preferred option for elderly patients or those weakened by prior treatments. Additionally, early studies have indicated that dendritic cell vaccines can grant a survival benefit of several months to over a year when combined with other therapeutic modalities, such as chemotherapy or ablation techniques.
The technique involves:
- Obtaining a patient's dendritic cells
- Maturing them in laboratory conditions under the influence of various nutrients
- Introducing them to tumor-associated antigens
- Reintroducing them into the patient's bloodstream
Once inside the body, these reprogrammed cells initiate an immune response against malignant pancreatic cells. Dendritic cell therapy, awarded the 2011 Nobel Prize in Physiology or Medicine, has opened a new frontier in treating tumors considered unresponsive to conventional therapies [7]. To gain deeper insight into how dendritic cell therapy is transforming 4 stage pancreatic cancer treatment, please watch an interview discussion with Professor Frank Gansauge, a leading immunotherapy expert in Germany. In this interview, he explains the scientific foundations behind the dendritic cell therapy and shares firsthand data on treatment outcomes and the overall procedure of dendritic cell therapy.
"Every Patient Deserves an Individual Approach": Interview with Renowned German Immunologist Prof. Gansauge
Hyperthermia in Stage 4 Pancreatic Cancer
Hyperthermia is part of an integrative pancreatic cancer treatment, which was previously known as a supportive treatment to alleviate symptoms. However, it is currently being rediscovered as a valuable tool for stage 4 pancreatic cancer treatment. Hyperthermia works by increasing tissue temperature and causing disruption of local regulatory pathways apart from direct cytotoxic effect. As a result, malignant cells may be cut off from the nutrition elements they obtain from the bloodstream and decay.
Pancreatic cancer, including pancreatic adenocarcinoma (PAC), is known to develop a special fibrous matrix that protects the tumor and preserves its microenvironment. However, recent research demonstrated that magnetic hyperthermia (heat generated by magnetic nanoparticles in an electric field) can lead to decrease of tumor volume and stimulate programmed cell death. Additionally, mild hyperthermia disrupts the tumor cell membrane, which enhances permeability of the tumor and its sensitivity to systemic therapy. Mild hyperthermia, especially when induced by photothermal therapy, can also activate an immune response aimed at disrupting the tumor microenvironment and making stage IV pancreatic cancer more susceptible to immunotherapy.
In a Nutshell: Stage 4 Pancreatic Cancer Treatments in Numbers
Feel free to study the comparative tables provided below in order to compare various treatments.
| Characteristics/Therapy type | 2-Year Survival Rate | Response Rate | Duration | Side Effects |
|---|---|---|---|---|
| Standard Treatment | ~25% for advanced cancer | Less than 10% | Several cycles | Severe (nausea, fatigue, hair loss, immunosuppression, skin irritation) |
| Innovative Methods | ~60% for advanced cancer | 45-65% | Up to 4 sessions | Mild (localized discomfort) |
* Booking Health data
Comparative table of prices for standard and innovative treatment methods in Germany, Great Britain, and the USA
| Treatment Method | GERMANY* | GB | USA |
|---|---|---|---|
| Standard Treatment | €80,000 - €150,000 full course | €90,000 - €165,000 full course | €100,000 - €180,000 full course |
| Innovative Methods | €25,000 - €60,000 full course | €70,000 - €120,000 full course | €100,000 - €150,000 full course |
* The estimated costs are approximate and may vary depending on the country, medical facility, treatment protocol, number of sessions, and individual patient needs.
Not a Sentence: How Dendritic Cell Therapy Helps to Battle Advanced Pancreatic Cancer
In early 2024, Robert Franklin Smith from the United States faced a devastating diagnosis: pancreatic cancer with liver metastases. As a devoted husband and father, he knew that time for him and his family was working against them. They immediately initiated standard therapy protocol. After undergoing liver surgery and beginning rounds of chemotherapy, the Smith family was determined to leave no stone unturned in their search for the most advanced treatments available.
Despite the best efforts of his doctors, the family felt they had reached a plateau. However, a new path opened during this time when Robert's wife began researching treatment abroad and came across dendritic cell therapy in Germany. That search led them to Booking Health company, a medical tourism operator renowned for its expertise in organizing treatment abroad.
From the first inquiry, Booking Health offered more than just logistical support. They provided clarity, compassion, and a sense of hope. "They handled everything: accommodations, translators, transfers, and medical documentation. They took care of every detail so we could focus on what mattered most: Robert's health," Mrs. Smith recalls. Their destination was the treatment of 4 stage pancreatic cancer in Germany, specifically at LDG Laboratories in Berg. It is a medical center run by Dr. Gansauge, a world-renowned specialist in immunotherapy. Dendritic cell therapy, a cutting-edge treatment that was not yet available in the United States, was available in Germany. So Robert grasped that opportunity and underwent treatment. The procedure, designed to stimulate the immune system to recognize and attack a patient's cancer cells, gave the family a renewed sense of control.
"What stood out was not only the level of care, but the human connection," Mrs. Smith shared. "Dr. Gansauge combined deep expertise with genuine warmth and humor. It gave us strength in a time we needed it most." As a valuable complementary tool to protocol treatment, dendritic cell therapy offered hope and brought back the living Robert and his family were looking for. It gave the sense of control by reducing recurrence and stabilizing disease course. Exceptionally well-tolerated with almost zero adverse effects, dendritic cell therapy enabled Robert Smith to accumulate extra power after exhausting chemotherapy and even rebuilt his health.
Today, as Robert continues his treatment journey, the Smiths speak openly about the turning point they experienced in Germany. Determination, persistence, and an openness to innovations paved the way for a new beginning, even for advanced cases of pancreatic cancer.

Hope in the Face of Advanced Pancreatic Cancer: a Novel Approach
Many believe that a diagnosis of stage 4 pancreatic cancer is somewhat "the end of the road." Standard therapies often offer limited results with survival remaining low and often coming at the cost of quality of life. For many patients, pancreatic cancer metastasis is synonymous with bleak prognoses and fading hope. However, this situation doesn't have to remain unchallenged. There is a growing body of evidence and real-world experience suggesting that even in the most advanced stages of cancer, there are viable and evolving options worth exploring.
Around the world, nations are making significant investments in cutting-edge medical research and the development of innovative therapeutic tools. One of the most promising developments in end-stage pancreatic cancer management is the adoption of a personalized, integrative approach. This involves tailoring therapies to the patient's unique clinical situation by combining novel immunotherapies, precision-targeted treatments, advanced imaging technologies, and minimally invasive procedures. These strategies aim not only to prolong overall survival, but also to enhance quality of life during treatment. While complete remission may yet remain unreachable, new strategies can offer improved daily functioning.
There is a growing body of evidence and real-world experience suggesting that even in the most advanced stages of cancer, there are viable options worth exploring. In the hands of experienced oncology specialists, modern multimodal therapeutic plans can stabilize the disease progression and even restore part of your previous daily routine. Seeking care in international medical centers with a reputation for breakthrough medical innovations can open up possibilities that standard protocols may not include. Whether through clinical trials or access to evidence-supported treatments or multidisciplinary approaches, patients often discover options that grant them renewed control over their treatment journey.
Taking the first step to explore other opinions, investigate medical centers abroad, and be open to new therapies can be a critical turning point. In many cases, what appears to be a closed door at home could be an open gateway abroad. For those battling advanced pancreatic cancer, persistence and hope are the key. Although a universal cure may not yet exist, those willing to search for it can find meaningful ways to extend life, stabilize disease, and improve well-being.
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. After undergoing multiple treatment sessions, consulting numerous specialists, and trying various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized, innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex cancer management programs in each case. As a reputable company, Booking Health offers personalized stage 4 pancreatic cancer treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you on the way of pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for metastatic pancreatic cancer with leading specialists in this field.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
Frequently Asked Questions About Stage 4 Pancreatic Cancer
Send request for treatmentAdvanced pancreatic cancer may present various symptoms, including unexplained weight loss, changes in appetite, and abdominal discomfort. Early detection can be challenging as symptoms often appear gradually.
Diagnosis involves comprehensive medical examination and staging procedures, including imaging tests (CT, MRI) and biopsy.
Best treatment for stage 4 pancreatic cancer includes the following:
- Innovative methods:chemoembolization, immunotherapy, and interventional radiology techniques
- Traditional approaches: chemotherapy and chemoradiation. The choice depends on individual cases and overall health condition.
While stage 4 pancreatic cancer is considered metastatic, modern treatment methods focus on extending life expectancy and improving quality of life. Research continues to advance treatment possibilities.
Life expectancy varies significantly based on individual factors. Recent medical advances, including targeted therapies, have shown promise in extending survival rates beyond traditional expectations.
While surgery is less common in advanced cases, some patients may benefit from surgical interventions, especially after undergoing innovative treatment like ablation or chemoembolization.
Treatment effects vary by individual. Common side effects include:
- fatigue,
- nausea and vomiting,
- lack of appetite and indigestion,
- blood disorders,
- persistent headache and dizziness.
Modern approaches aim to minimize discomfort while maximizing effectiveness through personalized treatment plans.
At this stage, cancer may spread to other organs, particularly the liver. Treatment strategies address both the primary tumor and any metastatic sites.
While complete remission is rare, innovative treatments have shown promising results in managing the disease and extending survival rates.
Yes, ongoing research continues to develop new treatment methods. Modern medical centers offer access to advanced therapies and innovative approaches, including dendritic cell therapy, chemoembolization, and ablation.
Pain management is an essential part of treatment, utilizing various medical and interventional methods to ensure patient comfort and maintain quality of life.
Survival rates have improved with modern treatments. While traditional statistics show lower rates, innovative therapies are showing more promising outcomes.
Pancreatic adenocarcinoma is the most common type of pancreatic cancer, arising from the exocrine cells that produce digestive enzymes. It tends to be aggressive, grows quickly, and often presents at an advanced stage.
Pancreatic neuroendocrine tumors (PNETs), on the other hand, originate from the hormone-producing cells of the pancreas. They are much rarer, usually grow more slowly, and may produce specific hormones that cause distinct clinical syndromes.
Yes, metastatic spread can occur to various organs with the liver being the most common metastatic site. Treatment strategies address both the primary tumor and the potential spread to other areas.
For stage 4 pancreatic cancer, the 2-year survival rate with standard chemotherapy is around 25%. In turn, innovative methods (e.g., dendritic cell therapy, TACE, or ablation) can raise survival to about 60%.
What response rates are observed in stage 4 pancreatic cancer with standard and innovative therapies?
In stage 4 pancreatic cancer, standard treatments typically provide a response rate below 10%. In contrast, innovative approaches (e.g., dendritic cell therapy, electrochemotherapy, or TACE) can achieve 45-65%.
Standard treatment for stage 4 pancreatic cancer often involves multiple chemotherapy cycles over several months. On the other hand, innovative methods (e.g., TACE, dendritic cell therapy, or ablation) are generally completed in up to four sessions.
Standard chemotherapy for stage 4 pancreatic cancer often causes severe side effects such as nausea, fatigue, and immune suppression. However, innovative therapies (e.g., cryoablation, TACE, or dendritic cell therapy) are typically well tolerated, causing only mild, localized discomfort with faster recovery.
Stage 4 pancreatic cancer is treated with palliative intent. Systemic therapy remains the backbone while interventional radiology is used for local tumor control (or management of complications); dendritic cell therapy may be considered as an adjunct immunological approach; hyperthermia can be applied to enhance treatment sensitivity.
Optimal care requires centers experienced in advanced pancreatic cancer management. Hospitals capable of integrating systemic therapy with interventional radiology, immune-based treatments and supportive procedures are preferred – as they allow individualized treatment decisions (beyond standard chemotherapy protocols).
Germany is frequently selected due to availability of extended treatment strategies. Patients can access interventional radiology, dendritic cell therapy and hyperthermia within regulated clinical settings – enabling personalized approaches for advanced pancreatic cancer (when standard options are limited).
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] American Cancer Society. Survival Rates for Pancreatic Cancer. https://www.cancer.org/cancer/types/pancreatic-cancer/detection-diagnosis-staging/survival-rates.html
[2] NIH, National Cancer Institute. Pancreatic Cancer Treatment (PDQ®)–Patient Version. https://www.cancer.gov/types/pancreatic/patient/pancreatic-treatment-pdq
[3] NIH, National Library of Medicine. Toxicity and response criteria of the Eastern Cooperative Oncology Group. https://pubmed.ncbi.nlm.nih.gov/7165009/
[4] NIH, National Library of Medicine. BRCA1, BRCA2, PALB2, and CDKN2A mutations in familial pancreatic cancer: a PACGENE study. https://pubmed.ncbi.nlm.nih.gov/25356972/
[5] American Cancer Society. Ablation or Embolization Treatments for Pancreatic Cancer. https://www.cancer.org/cancer/types/pancreatic-cancer/treating/ablative-techniques.html
[6] PubMed Central. Efficacy of transcatheter arterial chemoembolization for liver metastases arising from pancreatic cancer. https://pmc.ncbi.nlm.nih.gov/articles/PMC5503649/
[7] PubMed. The 2011 Nobel Prize in physiology or medicine. https://pubmed.ncbi.nlm.nih.gov/22053831/
[8] Aigner, K.R., Gailhofer, S., Selak, E. et al. Intra-arterial infusion chemotherapy versus isolated upper abdominal perfusion for advanced pancreatic cancer: a retrospective cohort study on 454 patients. J Cancer Res Clin Oncol 145, 2855–2862 (2019). https://doi.org/10.1007/s00432-019-03019-6. [DOI]
Read:
Pancreatic Cancer Treatment: Guideline for Treatment Options
Germany offers dendritic cell-based immunotherapy for pancreatic cancer
Article menu:
- Conventional Treatment for Metastatic Pancreatic Cancer
- Novel Ways to Manage Stage 4 Pancreatic Cancer
- In a Nutshell: Stage 4 Pancreatic Cancer Treatments in Numbers
- Not a Sentence: How Dendritic Cell Therapy Helps to Battle Advanced Pancreatic Cancer
- Hope in the Face of Advanced Pancreatic Cancer: a Novel Approach
- A Medical Journey: Every Step of the Way With Booking Health
- Frequently Asked Questions About Stage 4 Pancreatic Cancer
Don't know where to start?
Contact Booking Health