The program includes:
- Initial presentation in the clinic
- Clinical history taking
- Review of medical records
- Physical examination
- Laboratory tests:
- Complete blood count
- General urine analysis
- Biochemical analysis of blood
- Indicators of inflammation (CRP, ERS)
- Indicators of blood coagulation
- Blood pressure measurement
- ECG
- Echocardiography, if necessary, transesophageal one
- Preoperative care
- Catheterization of blood vessels and heart chambers
- Transcatheter implantation of the Mitralign system
- Symptomatic treatment
- Control examinations
- Full hospital accommodation
- Cost of essential medicines and materials
- Nursing services
- Explanation of future recommendations
Indications
- Functional mitral regurgitation (FMR)
- Combination of FMR with tricuspid regurgitation
How program is carried out
Day 1-2. Initial presentation at the clinic. After consultation with the attending physician and physical examination, the patient undergoes the necessary laboratory and instrumental examination.
Day 3. On the 2-3 day of hospital stay, after receiving the examination results and their assessment by the attending physician, the transcatheter implantation of the Mitralign system is performed. In most cases, the operation requires only local anesthesia at the site of catheter insertion. If the patient can not tolerate a probe for an intraoperative transesophageal echocardiography, then general anesthesia may be given.
After insertion into the femoral artery, a guide catheter is moved towards the heart, delivered through the aortic valve and placed on the posterior side of the left ventricle. EchoCG is used to confirm wire placement in the mitral annulus. Pledgets are fixed inside the atrium and ventricle, plicated, pooled together, and locked. Then the same steps are repeated on the other side of the mitral annulus. Pledgets reduce the circumference of the mitral annulus and correct the functional mitral regurgitation. After installing and fixing the Mitralign system, the catheter is removed, and a pressure bandage is applied to the place of its introduction for several hours.
From day 4. The patient stays in the ward of the cardiology department, under the supervision of doctors and nursing staff. Depending on the dynamics of the health condition, the patient is discharged from the hospital in 5-10 days.
Required documents
- Medical records
- EchoCG (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
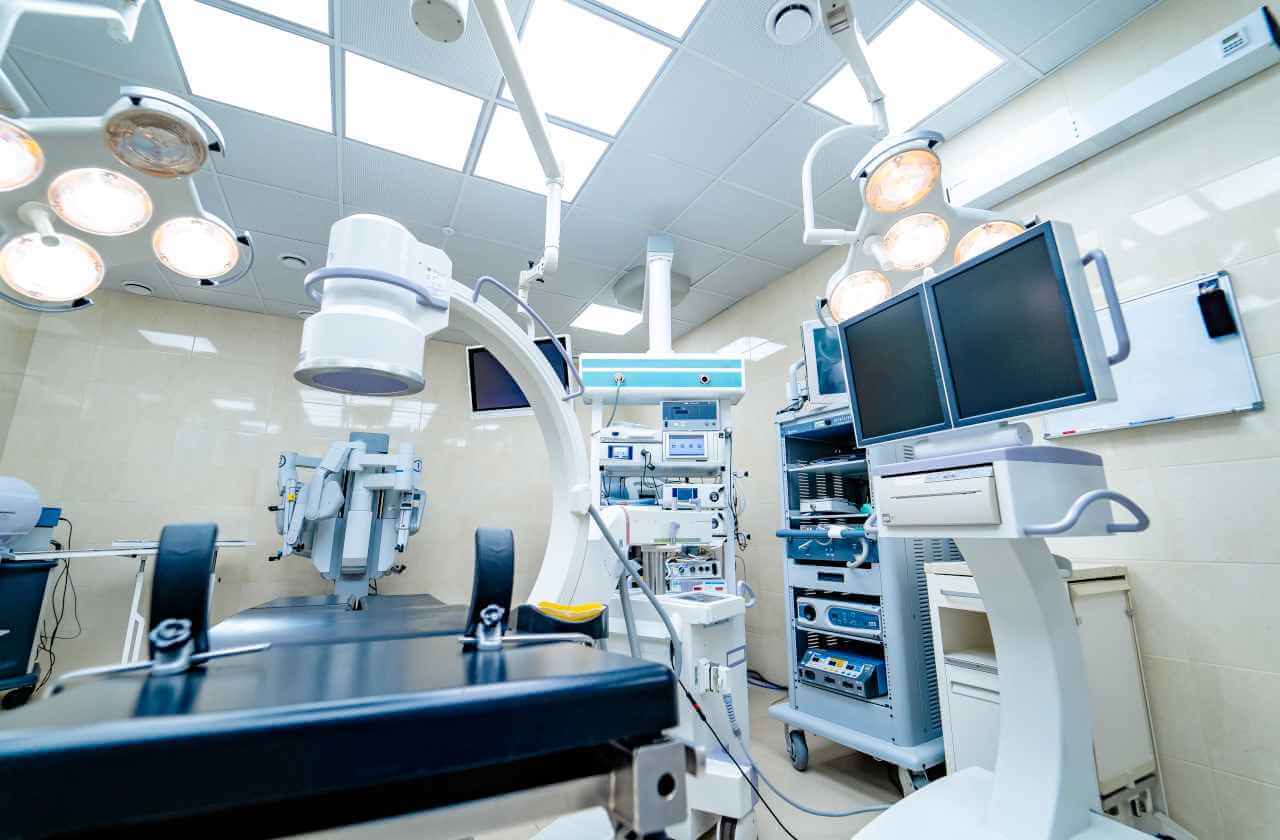
The Department of Cardiac Surgery at the Helios Hospital Siegburg offers the full range of surgical treatment for heart disease, with the exception of chest organ transplants. The medical facility successfully performs operations for mitral, aortic, and tricuspid valve replacement and repair, operations for the implantation of pacemakers, implantable cardioverter-defibrillators, and devices for cardiac resynchronization therapy, operations for thoracic aortic aneurysms and dissection, coronary artery bypass grafting, and operations for the implantation of ventricular assist devices and artificial hearts (VAD and TAH). Most surgical procedures are performed using minimally invasive techniques without opening the chest. The department is part of the Heart Center Siegburg, where cardiac surgeons, cardiologists, and vascular surgeons work together for the benefit of patients. Complex clinical cases are considered by medical boards. This allows physicians to develop the most effective course of treatment for each patient. The Heart Center Siegburg treats over 7,000 patients annually, many of whom undergo cardiac surgery. Along with the use of the latest technologies and treatment methods, the department's cardiac surgeons attach importance to a humane attitude towards patients.
The Head Physician of the department is Prof. Dr. med. Mirko Doss. The specialist is one of the best cardiac surgeons in Germany. He has performed thousands of successful heart surgical procedures. Minimally invasive heart interventions are of particular clinical interest to Prof. Mirko Doss.
Surgery for heart valve disease is among the department's clinical priorities. The department's surgeons almost daily perform operations to repair or replace the mitral, aortic, and tricuspid valves. Whenever possible, repair surgery is preferred to preserve the patient's own valve. Surgical interventions on heart valves are performed using minimally invasive techniques, which significantly reduces surgical risks, and the patient's recovery in the postoperative period occurs quite quickly. Heart valve replacement is indicated for patients with mitral, aortic, or tricuspid stenosis. The department's cardiac surgeons perform operations to implant biological and mechanical prostheses. Biological prostheses are made from animal heart tissue (most often pigs). Due to the relatively short service life of biological prostheses (12-15 years), they are recommended for patients over 65 years of age. Young patients undergo surgery to implant mechanical prostheses that have an almost unlimited service life. The disadvantage of a mechanical prosthesis is the need for lifelong use of anticoagulants.
Coronary artery bypass grafting (CABG) is one of the most demanded operations in the department. The main indication for CABG is coronary heart disease. Cardiopathology develops due to the formation of atherosclerotic plaques in the coronary arteries, which leads to a pronounced narrowing of the lumen of the coronary arteries or a complete cessation of blood flow through the blood vessel. Due to the disruption of the blood supply to the heart, the patient experiences a number of unpleasant symptoms, and if left untreated, coronary heart disease may potentially lead to death. Coronary artery bypass grafting is a last-line treatment. Surgery is prescribed in cases of failure of drug therapy and coronary angioplasty. The essence of CABG is to create a bypass that will allow for blood flow without going through the coronary arteries affected by atherosclerosis. A blood vessel from another part of the patient's body is used as a bypass. Surgeons most often use arteries and veins from the leg or chest wall. The purpose of the operation is to normalize the blood supply to the myocardium. The department's specialists successfully perform both the classic version of CABG using a heart-lung machine and off-pump coronary artery bypass grafting (OPCAB). In 65% of cases, the department's surgeons perform CABG on a beating heart.
The department's cardiac surgeons also specialize in performing revision coronary artery bypass grafting. It may be required if the patient has recurrent coronary artery stenosis and occlusion years after primary CABG. Cardiac revision surgery is more complex and involves high risks for the patient. The department's specialists have impressive experience in performing such operations. Revision CABG success rates are at a very high level here. Revision coronary artery bypass grafting is often performed in a medical facility without the use of a heart-lung machine.
The department is one of the few in Germany that brilliantly performs operations to implant mechanical circulatory support systems in patients with heart failure. This disease affects the pumping function of the heart, making it unable to deliver the required amount of blood and oxygen to organs and tissues. The first-line treatment is drug therapy. If this does not give the desired result, doctors may consider the option of implanting a mechanical circulatory support device. The department's cardiac surgeons perform surgery to implant a ventricular assist device (VAD) and a total artificial heart (TAH). TAH implantation is performed extremely rarely. For example, only 7 such systems were implanted in Germany in 2017, 2 of which were implanted in the Department of Cardiac Surgery at the Helios Hospital Siegburg. It is worth noting that the department was one of the pioneers in Germany and Europe in the implantation of total artificial hearts (TAH).
The department's range of surgical services includes the following:
- Surgery for heart valve diseases
- Mitral valve repair and replacement for mitral valve stenosis and insufficiency
- Aortic valve repair and replacement for aortic valve stenosis and insufficiency
- Tricuspid valve repair and replacement for tricuspid valve stenosis and insufficiency
- Coronary artery bypass grafting for coronary heart disease
- Classic coronary artery bypass grafting with the opening of the chest
- On-pump coronary artery bypass grafting (OPCAB)
- Minimally invasive direct coronary artery bypass grafting (MIDCAB)
- Revision coronary artery bypass grafting
- Surgery for arrhythmias (heart rhythm disturbances)
- Pacemakers and defibrillator implantation
- Catheter ablation for atrial fibrillation
- Surgery for thoracic aortic aneurysms and dissection
- Endovascular procedures
- Classical operations
- Surgery for the implantation of mechanical circulatory support devices for heart failure
- Ventricular assist device (VAD) implantation
- Total artificial heart (TAH) implantation
- Surgery for infective endocarditis
- Reconstructive plastic surgery
- Heart tumor resection surgery
- Minimally invasive surgery
- Other heart surgical procedures
Curriculum vitae
Higher Education
- 2008 PhD, Johann Wolfgang Goethe University Frankfurt.
- 2000 Doctorate in Medicine, University of Ulm.
Professional Career
- Since 06.2021 Head Physician, Department of Cardiac Surgery, Helios Hospital Siegburg.
- 09.2014 - 06.2021 Cardiac Surgeon, Heart Center, Kerckhoff Hospital Bad Nauheim.
- 09.2007 - 08.2014 Consultant, Edwards Lifesciences, Miami, Florida, USA.
- 01.2005 - 12.2012 Cardiac Surgeon, Heart Center Frankfurt.
- 01.1999 - 01.2014 Professor for Cardiac Surgery, Johann Wolfgang Goethe University Frankfurt.
- 10.1996 - 12.1998 Residency, Department of Cardiac Surgery, University Hospital Ulm.
- 03.1993 - 09.1993 Internship, Research Center at California Pacific Medical Center, San Francisco, California, USA.
Clinical Interests
- Minimally invasive mitral valve surgery.
- Minimally invasive aortic valve surgery.
- Catheter-based interventions for heart valve replacement.
- Aortic surgery.
Memberships in Professional Societies
- German Society for Thoracic and Cardiovascular Surgery (DGTHG).
- European Association for Cardio-Thoracic Surgery (EACTS).
- Heart Valve Society (HVS).
Photo of the doctor: (c) Helios Klinikum Siegburg
About hospital
The Helios Hospital Siegburg enjoys an excellent reputation in North Rhine-Westphalia and throughout Germany. The healthcare facility provides comprehensive medical care that meets current clinical protocols and international standards. The hospital has more than 350 beds. The hospital employs a highly motivated team of doctors and nursing staff that consists of more than 850 employees. The hospital treats more than 20,000 inpatients and over 30,000 outpatients.
The healthcare facility represents many areas of modern medicine, including cardiac surgery, general surgery, abdominal surgery, vascular surgery, thoracic surgery, orthopedics, trauma surgery, spinal surgery, cardiology, gastroenterology, pulmonology, and radiology.
The Helios Hospital Siegburg operates one of the best and most progressive Heart Centers in Germany. Cardiologists, cardiac surgeons, vascular surgeons, and anesthesiologists work hand in hand here and brilliantly cope with the treatment of both common and particularly complex heart disease. The specialists at the Heart Center Siegburg annually treat more than 7,000 patients using modern conservative, catheter-based, and surgical techniques.
The medical facility also includes the specialized Bariatric Surgery Center Siegburg, the Hernia Surgery Center Rhine-Sieg, the Thoracic Surgery and Pulmonology Center Bonn-Siegburg, the Spine Surgery Center Bonn-Siegburg, and the Aortic Surgery Center Rhine-Sieg. Each of these centers has a highly professional team of doctors who specialize in the treatment of a specific group of diseases.
The medical staff at the Helios Hospital Siegburg not only monitors the high quality of medical care but also makes every effort to ensure that the patient feels as comfortable as possible during the therapeutic process. Doctors and nursing staff are sensitive to the individual needs and wishes of their patients, are always open to dialogue, and provide moral support at every stage of treatment.
Photo: (с) depositphotos
Accommodation in hospital
Patients rooms
Patients of the Helios Hospital Siegburg live in comfortable single and double rooms. The furnishings of the patient room include an automatically adjustable bed, a bedside table with a pull-out tray, a wardrobe, a table, chairs, and a TV. The patient rooms have access to Wi-Fi. Each patient room has an ensuite bathroom with a shower and a toilet.
Meals and Menus
The patient and his or her accompanying person are provided with three meals a day. Breakfast and dinner are served buffet style, and there is a choice of several set menus for lunch.
If, for some reason, you do not eat all the foods, you will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to your treatment.
Further details
Standard rooms include:
![]() Toilet
Toilet
![]() Shower
Shower
![]() Wi-Fi
Wi-Fi
![]() TV
TV
Accompanying person
Your accompanying person may stay with you in your patient room or at the hotel of your choice during the inpatient program.
Hotel
You may stay at the hotel of your choice during the outpatient program. Our managers will support you for selecting the best option.