The program includes:
- Initial presentation in the clinic
- clinical history taking
- physical examination
- review of medical records
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- indicators of inflammation
- indicators blood coagulation
- x-ray examination
- CT/MRI scan
- preoperative care
- hip replacement
- symptomatic treatment
- control examinations
- physiotherapeutic procedures
- orthopedic appliances
- the cost of essential medicines and materials
- nursing services
- full hospital accommodation
- explanation of future recommendations
How program is carried out
Preliminary preparation for hip replacement includes quitting smoking and drinking alcohol; cancelling non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen); cancelling anticoagulants (warfarin); normalization of body mass, if possible.
Preoperative examination, including consultation with an anesthesiologist and necessary related specialists, takes 1-2 days. According to its results, the most suitable endoprosthesis is selected.
Hip replacement. The operation is performed under general anesthesia. The patient lies on his side, the affected leg is bent and fixed in this position. The surgeon makes an incision 15-20 cm long, minimally traumatizing the muscles and nerve endings. Through this incision, miniature instruments are inserted to remove the damaged joint structures. Healthy bone is adjusted for further reliable implant fixation.
The surgeon installs a femoral stem in the center of the upper part of the femur. Ball-shaped head of the joint is fixed on it. The surgeon also implants a special liner that facilitates movement of the leg and protects the structures of the prosthesis. After the primary fixation of the prosthesis components, the doctor assesses the joint range of motion, as well as the length and symmetry of the lower limb.
The implant is fixed with cement or cementless method. The doctor treats the operating field with antiseptics, conducts its final revision and sutures the wound layer by layer. A temporary drainage is installed in the joint, and a bandage is applied on top.
Postoperative care. During the first day after the intervention the patient stays in the intensive care unit, under round-the-clock medical supervision. After that, with a smooth course of the postoperative period, the patient is transferred to a regular ward and the drains are removed. The range of motion expands gradually, from light toes movements to walking. Walking with the use of walking aids is allowed in 3-5 days after the operation.
Required documents
- Medical records
- X-ray examination, MRI/CT scan (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
The Department of Orthopedics and Traumatology at the Helios Hospital Hildesheim offers effective treatment for the patients suffering from musculoskeletal diseases and injuries of any severity. The department's doctors have in their arsenal both conservative and surgical treatment methods. The department's operating rooms are equipped with the very latest technology, and therefore most operations on the joints, bones, muscles, ligaments and other anatomical structures of the musculoskeletal system are performed using sparing minimally invasive surgical techniques. Such an approach allows the patients to more easily undergo treatment and recover after surgery as soon as possible. The Chief Physician of the department is Prof. Dr. med. Burkhard Wippermann.
One of the key focuses of the department's clinical practice is joint replacement surgery. The medical facility has the most prestigious certificate in Germany in this field (endoCert) and has the status of the Maximum Care Endoprosthetics Center. The department's surgeons successfully perform surgery to replace hip, knee, shoulder, elbow and ankle joints, as well as revision interventions to replace worn-out endoprostheses. At the stage of diagnostics, an attending physician accurately examines the patient, assesses the degree of joint damage and determines which treatment methods will be the most effective in a particular clinical case. With the timely treatment of the patient in the department, it is possible to avoid invasive therapy, but use only drug therapy and physiotherapy. In the case of arthrosis, the patient begins to experience pain only at the advanced stage, and therefore the department's doctors quite often have to resort to surgery for partial or total joint replacement. To replace joints, the medical facility uses only high-quality prostheses made of durable materials, the service life of which ranges from 15 to 20 years. The replacement of joints eliminates pain, restores the patient's freedom of movement and the ability to lead an active lifestyle. After the intervention, the department's patients undergo a rehabilitation program, the duration of which is 8-10 days. The rehabilitation begins immediately after surgery. The experienced medical staff and physiotherapists who monitor the achieved progress take care of the patient. Whenever required, after discharge from the hospital, rehabilitation treatment can be continued within the specialized Rehabilitation Center.
The department is recognized as a regional Trauma Center – its doctors provide effective treatment for all kinds of injuries, including multiple ones (polytrauma). About 15,000 patients with various injuries are admitted to the department annually. Medical care is provided by a highly professional team of specialists consisting of emergency doctors, general and abdominal surgeons, vascular, spinal, thoracic and plastic surgeons, anesthesiologists and other doctors. The department has a helipad for prompt round-the-clock delivery of patients.
An important area of the department's clinical practice is the treatment of benign and malignant musculoskeletal tumors. Primary tumors of this spectrum develop quite rarely, and therefore, in most cases, the doctors diagnose secondary musculoskeletal tumors caused by breast, lung, prostate, bowel, kidney and other cancers. The optimal treatment regimen is developed at an interdisciplinary tumor board with the participation of orthopedists, oncologists, radiologists, radiation therapists and other specialists. In especially complex cases, the medical team attracts highly qualified doctors from the Hanover Medical School that is one of the best university hospitals in Germany. The classical treatment protocol includes tumor resection surgery, chemotherapy and/or radiation therapy. After completing the main treatment course, the patient is recommended to undergo regular follow-up diagnostic examinations in order to prevent cancer recurrence.
The department's medical team has excellent qualifications in the treatment of shoulder injuries and diseases: impingement syndrome, calcific tendonitis, rotator cuff tear, shoulder instability, shoulder arthritis, etc. The therapeutic options include both conservative and surgical treatments. The department's doctors follow modern clinical protocols, thus achieving high efficiency of therapy. To provide comprehensive medical care, the department's doctors cooperate closely with physiotherapists. This approach allows the patient to recover after the completion of the main treatment, taking into account all his needs and wishes.
The department's main clinical focuses include:
- Partial and total hip, knee, shoulder, elbow and ankle replacement surgery
- Conservative and surgical treatment of injuries of any severity, including multiple injuries (polytrauma)
- Conservative and surgical treatment of hip diseases
- Hip dysplasia
- Rheumatic lesions
- Avascular necrosis of the femoral head
- Perthes disease
- Epiphyseal femoral head fractures
- Femoral head and acetabular fractures
- Pathological hip lesions caused by gout
- Conservative and surgical treatment of knee diseases
- O-shaped and X-shaped deformities of the lower extremities
- Rheumatic lesions
- Knee fractures
- Cruciate ligament tears
- Meniscus tears
- Osteochondritis dissecans
- Pathological knee lesions caused by gout
- Conservative and surgical treatment of shoulder diseases
- Impingement syndrome
- Calcific tendonitis
- Bursitis
- Biceps brachii tendon injuries
- Rotator cuff tear
- Shoulder instability
- Conservative and surgical treatment of musculoskeletal tumors
- Bone tumors
- Muscle tumors
- Ligament and tendon tumors
- Cartilage tumors
- Intervertebral disc tumors
- Other medical services
Curriculum vitae
Higher Education and Professional Career
- March 1977 - April 1978 Study of Medicine at the University of Marburg.
- April 1978 - November 1982 Study of Medicine at the Hannover Medical School.
- September 1980 - April 1981 Study of Medicine at the Mayo Clinic, Rochester.
- February 1982 - May 1982 Study of Medicine in Minnesota, USA (funded by the Rotary Foundation).
- November 1982 Obtaining a license for medical practice after successful state examination at the Hanover Medical School.
- October 1983 Visa Qualifying Examination (VQE).
- March 1985 Doctoral thesis defense. Subject: "Comparative tests with a quantitative assessment of the concentration of lipoproteins in human serum".
- January 1994 Habilitation in Traumatology.
- April 1998 Extraordinary Professorship.
- December 1982 - February 1984 Military service as Military Doctor.
- September 1984 Completion of doctoral thesis.
- October 1984 - September 1986 Resident, Department of Traumatology, Hannover Medical School.
- October 1986 - December 1987 Research Internship at the Biomechanics Laboratory of the Mayo Clinic, Rochester, Minnesota, USA (grant from the German Research Foundation (DFG)).
- 1988 Resident in the Department of Pediatric and Adolescent Medicine at the Hannover Medical School.
- November 1988 - October 1989 Physician, Emergency Care Unit, Hannover Medical School.
- November 1989 - February 1990 Intensive Care Specialist, Department of Emergency Surgery, Hannover Medical School.
- March 1990 - August 1991 Physician in the Department of Surgery at the Hospital Siloah, Hanover.
- September 1991 - December 1995 Resident, Department of Traumatology, Hannover Medical School.
- March 1992 Board certification in Surgery.
- June 1993 Additional certification in Emergency Medicine.
- Since September 1993 Physician in the Department of Trauma Surgery, Hannover Medical School.
- January 1996 - July 2001 Physician in the Department of Trauma Surgery, Hannover Medical School.
- Since August 2001 Head of the Department of Orthopedics and Traumatology at the Helios Hospital Hildesheim.
Clinical Interests
- Joint replacement surgery.
- Correction of limb defects.
- Surgery to remove musculoskeletal tumors.
Photo of the doctor: (c) Helios Kliniken GmbH
About hospital
The Helios Hospital Hildesheim positions itself as an advanced provider of high-quality medical services at the European level. The medical facility is an Academic Hospital of the Hannover Medical School, thanks to which it can successfully introduce the very latest medical achievements into clinical practice. The hospital is distinguished by the excellent quality of diagnostics, highly effective treatment of pathologies of any severity and the best patient care based on understanding and humane attitude. The history of the medical complex dates back to 1838, so it carefully honors traditions, but at the same time the hospital actively uses innovative diagnostic and treatment methods. The medical team of the hospital consists of more than 1,450 people. The hospital employs highly qualified doctors who are rightfully proud of their treatment outcomes.
The medical facility has 579 beds. The team of doctors working at the hospital treats more than 28,000 inpatients and about 80,000 outpatients every year. The patients from foreign countries often undergo diagnostics and treatment in the hospital, which confirms the excellent reputation of the medical center in the international arena.
The hospital offers highly specialized departments with different medical focuses, including oncology, cardiology, gastroenterology, gynecology, dermatology, otolaryngology, general and abdominal surgery, plastic and aesthetic surgery, traumatology, etc. Many medical fields are awarded with prestigious certificates, including German Cancer Society (DKG) certification, IQM certification, and others.
Photo: (с) depositphotos
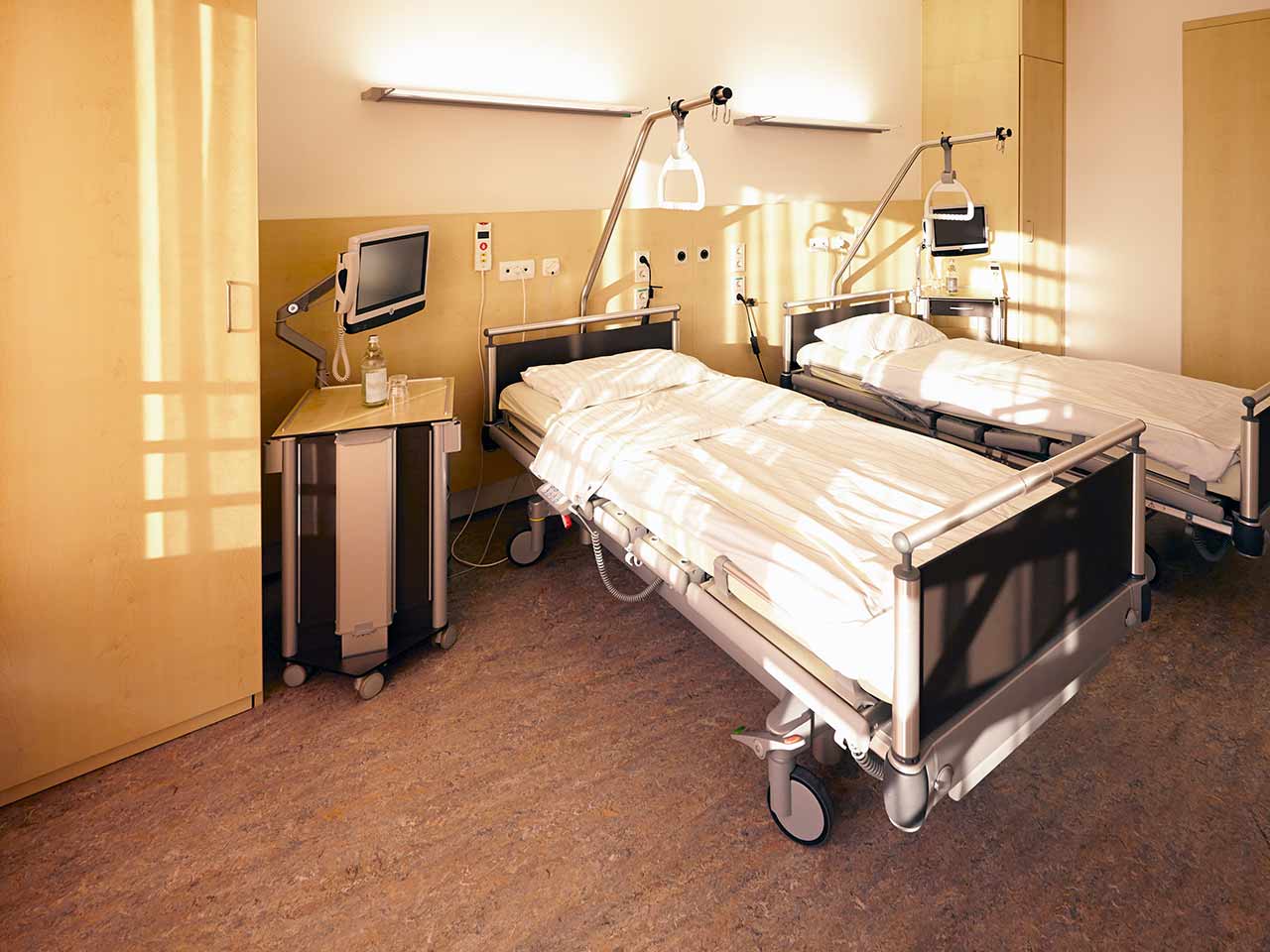
Accommodation in hospital
Patients rooms
The patients of the Helios Hospital Hildesheim live in spacious and light rooms. The furnishings of a standard patient room includes an automatically adjustable bed with an orthopedic mattress, a bedside table, and a wardrobe for storing things. All patient rooms have telephone, radio and TV, as well as free Wi-Fi. For maximum convenience of patients, each room has an ensuite bathroom with shower and toilet.
If desired, the patient can stay in an enhanced-comfort room. Such rooms are distinguished by a more sophisticated design, and are additionally equipped with a safe, a minifridge and upholstered furniture.
Meals and Menus
The patients of the hospital are offered tasty and varied meals. Diet and vegetarian menus are also available. If the patient follows a special diet recommended by the attending physician, he will be provided with food cooked from approved products.
Breakfast is served buffet style: eggs, various types of cheese, sausage, buns, jam, vegetables. There are three set menus to choose from for lunch. Dinner is also served buffet style.
In addition, the hospital has a cozy cafe called Leckeria where one can have a delicious snack. The range of dishes includes light salads, hearty set meals, snacks, sandwiches, cakes, as well as tea, coffee and soft drinks. The terrace is open in the summertime.
Further details
Standard rooms include:
Television
All patient rooms have a TV set. The TV can be used with headphones – the patients can use their own headphones or ask for the headphones from the staff.
Religion
The patient can talk with a Christian priest at any time. Divine services are held every Sunday at 10 am (on the ground floor).
Other religious services are available upon request.
Accompanying person
During the inpatient program, the accompanying person can stay with the patient in a patient room or at a hotel of his choice. Our managers will help you choose the most suitable option.
Hotel
During the outpatient program, the patient can stay at a hotel of his choice. Our managers will help you choose the most suitable option.