The program includes:
- Initial presentation in the clinic
- clinical history taking
- physical examination
- review of medical records
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- indicators of inflammation (CRP, ESR)
- indicators of blood coagulation
- X-ray examination of the hip
- CT scan of the hip
- preoperative care
- endoprosthesis replacement
- symptomatic treatment
- control examinations
- physiotherapeutic procedures
- orthopedic appliances
- the cost of essential medicines and materials
- nursing services
- full hospital accommodation
- explanation of future recommendations
The program includes orthopedic rehabilitation:
- Primary presentation in the clinic
- medical history taking, including family history
- complex neurological and orthopedic examinations
- X-ray examination
- complex neurophysiological examinations
- individual rehabilitation program, which includes:
- Wii Fit training of balance
- neuropsychological therapy
- kinesiotherapy (physiotherapy)
- biocontrol with feedback
- healing deep muscle massage
- acupuncture in spasticity and pain syndromes
- occupational therapy
- psycho-educational classes
- individual physiotherapy
- microcurrent treatment
- fangotherapy / cryotherapy
- antispasmodic drug therapy
- hydrotherapy / massage therapy / reflexology
- training on special trainers
- and etc.
- nurses care
- stay in the hospital with full board
- symptomatic and drug therapy
How program is carried out
Preliminary preparation for surgery: quitting smoking and drinking alcohol 2 weeks before surgery; cancelling non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen); cancelling anticoagulants (warfarin); normalization of body mass, if possible.
Preoperative examination, including consultation with an anesthesiologist and necessary related specialists. X-ray examination and MRI of the hip joint are performed. The examination takes 1-2 days.
Surgical hip endoprosthesis replacement. The operation is performed under general anesthesia and lasts for about 2 hours.
Postoperative care. During the first day after the intervention the patient stays in the intensive care unit, under round-the-clock medical supervision. After that, with a smooth course of the postoperative period, the patient is transferred to a regular ward and the drains are removed. The range of motion expands gradually, from light toes movements to walking. Walking with the use of walking aids is allowed in 3-5 days after the operation. Normal walking without the use of walking aids (crutches, cane) will become possible in 6-12 weeks.
Finally, the attending physician will evaluate the results of control examinations, schedule the date of discharge from the hospital and give you detailed recommendations for further follow-up and treatment.
Rehabilitation. The rehabilitation program begins after the transfer of the patient from the intensive care unit to a regular ward. It includes physical activity (from exercises in bed in the early days to exercises in the gym), physiotherapy, massage (including lymphatic drainage). After discharge from the hospital, the patient is transferred to a specialized rehabilitation clinic for 2 weeks, where he undergoes an advanced rehabilitation course.
Required documents
- X-ray examination of the hip joints
- MRI scan of the hip joints, if available
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
According to the Focus magazine, the Department of Adult and Pediatric Orthopedics, Special Orthopaedic Surgery and Rheumatic Orthopedics at the University Hospital Frankfurt am Main ranks among the top German medical facilities specializing in the treatment of orthopedic diseases in adults and children, as well as in hip surgery!
The department offers the full range of medical services in these medical fields. It carries out both diagnostics and treatment of patients of all age groups, including very elderly patients, with various musculoskeletal diseases. The therapeutic options include both conservative and surgical treatment methods. The department is distinguished by high professionalism of doctors, advanced infrastructure and invaluable experience in the field of its specialization, due to which it occupies leading positions in the European medical arena and guarantees an optimal treatment result. The Chief Physician of the department is Prof. Dr. med. Ingo Marzi.
The department carries out productive research activities, which helps to introduce into clinical practice the very latest therapeutic techniques and thereby restore the function of the musculoskeletal system, including in particularly difficult cases. The goal of each department's physician is to provide the patient with a high-quality and effective long-term treatment outcome.
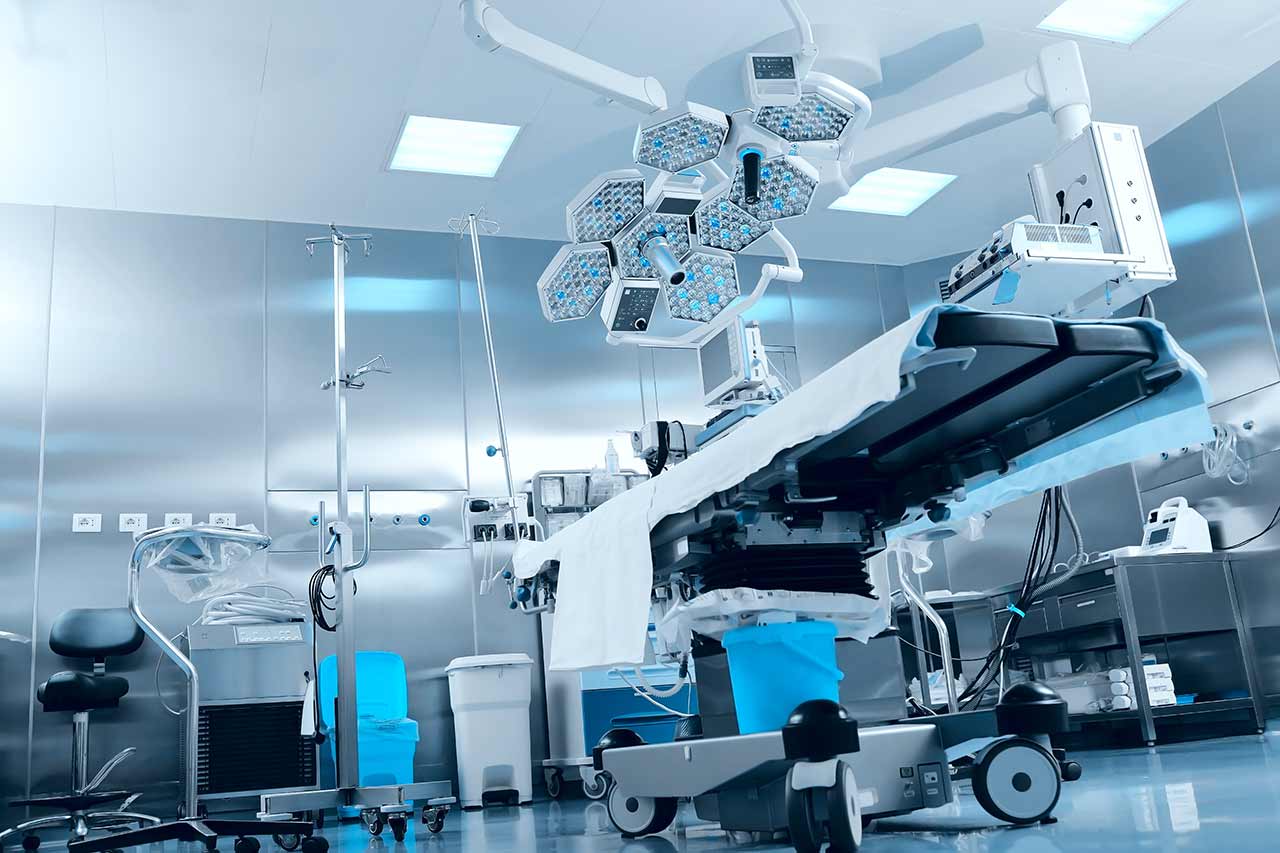
The department offers 88 beds for inpatient treatment and modern operating rooms. It treats more than 4,000 inpatients and about 17,000 outpatients every year.
The department includes Endoprosthetics Center of Maximum Care (EndoProthetikZentrum). It performs operations to partially and totally replace hip, knee, shoulder, elbow, and ankle joints. Due to the use of modern prostheses from the leading world manufacturers, as well as due to the use of the very latest surgical techniques, including minimally invasive ones, the doctors achieve excellent results in this field.
A special focus of the department's orthopedicians is the treatment of musculoskeletal diseases in children. Young patients require special approach to therapy, because their body is still growing. The doctors set themselves the task not only to eliminate the health problem, but also to ensure the proper development of the child's skeleton, joints, muscles and tendons.
The main clinical focuses of the department include:
- Endoprosthetics
- Corrective and remodeling osteotomy in joint deformity or arthrosis
- Treatment of joint lesions due to overloads, for example, after doing sports (arthroscopic interventions, procedures for the regeneration of cartilage tissue, reconstruction of tendons and ligaments)
- Total and partial replacement of all joints (using cement and cementless fixation)
- Replacement using minimally invasive techniques
- Replacement of worn or infected endoprostheses
- Bone tissue transplantation to compensate bone defects
- Treatment using special reconstructive implants
- Closure of massive defects using special implants (so-called individual prostheses)
- Treatment of orthopedic spinal diseases (all modern and classic conservative and surgical techniques are used)
- Cervical, thoracic and lumbar spinal diseases caused by degeneration of the spinal structures
- Spinal disc herniation
- Spinal stenosis
- Arthrosis of small intervertebral joints
- Spinal fractures
- Due to the osteoporosis
- Traumatic fractures
- Due to the tumor lesions (primary tumors and metastases)
- Spinal deformities
- Spinal curvature (scoliosis)
- Vertebral dislocation (spondylolisthesis)
- Infectious lesions of the vertebral bodies (spondylitis)
- Rheumatic diseases
- Cervical, thoracic and lumbar spinal diseases caused by degeneration of the spinal structures
- Pediatric orthopedics
- Conservative and surgical treatment of dysplasia and hip dislocation
- Conservative and surgical treatment of congenital and secondary clubfoot and other foot deformities
- Conservative and surgical treatment of Perthes disease
- Treatment of slipped capital femoral epiphysis
- Congenital and acquired axial deformities and/or lower limb shortening
- Scoliosis and other spinal deformities
- Congenital skeletal/metabolic dysplasias
- Rheumatic joint diseases
- Neuro-orthopedic diseases
- Foot surgery
- Valgus deformity of the great toe (hallux valgus)
- Degenerative arthritis of the first metatarsophalangeal joint of the foot (hallux rigidus)
- Hammer and claw fingers, Morton's neuroma
- Treatment-resistant heel spur, ligament tears, foot and ankle instability
- Foot and ankle arthrosis, foot and ankle fractures
- Injuries and ruptures of the Achilles tendon
- Aseptic bone necrosis (Keller's disease)
- Discomfort caused by additional foot bones (for example, os tibiale externum, os trigonum)
- Foot tumors
- Plantar fibromatosis
- Tarsal tunnel syndrome
- Oncologic orthopedics
- Diagnostics of unclear bone and soft tissue tumors
- Malignant tumors of bones and cartilages (for example, osteosarcomas, chondrosarcomas, Ewing's sarcomas)
- Metastases
- Malignant soft tissue tumors (soft tissue sarcomas, for example, liposarcomas, synovial sarcomas, fibrosarcomas, Ewing's sarcomas, angiosarcomas, malignant tumors of the peripheral nerves, leiomyosarcoma of the extremities)
- Benign bone tumors (for example, enchondromas, exostoses, osteoid osteomas, osteoblastomas)
- Benign soft tissue tumors (for example, lipomas)
- Plasmocytomas
- Tenosynovial giant cell tumors
- Bone cysts
- Giant cell bone tumors (osteoclastomas)
- Chondroblastomas
- Treatment of shoulder diseases
- Rotator cuff tear
- Shoulder replacement
- Shoulder dislocation and instability
- Shoulder fractures
- Clavicle fractures
- Impingement syndrome
- Forearm calcification
- Frozen shoulder
- Shoulder injuries
- Sports orthopedics
- Shoulder injuries
- Elbow injuries
- Hip injuries
- Ankle injuries
- Knee injuries
- Meniscus tears
- Cartilage damage
- Cruciate ligament injury
- Patella dislocation
- Other medical services
Curriculum vitae
Higher Education and Professional Career
- 1977 - 1983 Medical studies at the Johannes Gutenberg University Mainz.
- 1984 - 1985 Captain of the Medical Service in Kastellaun.
- 1985 Thesis defense in Neurology at the Johannes Gutenberg University Mainz.
- 1985 - 1986 Assistant Physician in the Department of Surgery at the St. Marienwoerth Hospital in Bad Kreuznach.
- 1987 - 1988 Research Fellowship from the German Research Foundation (DFG) at the Department of Pharmacology of the University of North Carolina, USA.
- 1986 - 1996 Assistant Physician and Senior Physician in the Department of Surgery at the University Hospital Saarland Homburg.
- 1993 Habilitation in Surgery at the Faculty of Medicine at the Saarland University in Homburg.
- 1996 - 1999 Managing Senior Physician in the Department of Trauma, Hand and Reconstructive Surgery at the University Hospital Saarland Homburg.
- 1998 Extraordinary Professorship at the Faculty of Medicine at the Saarland University in Homburg.
- 1999 - 2001 Acting Head Physician of the Department of Trauma, Hand and Reconstructive Surgery at the University Hospital Saarland Homburg.
- 2001 Professorship at Goethe University in Frankfurt am Main.
- Since 2001 Head Physician of the Department of Adult and Pediatric Trauma, Hand and Reconstructive Surgery at the University Hospital Frankfurt am Main.
- Since 2022 Acting Head Physician of the Department of Adult and Pediatric Orthopedics, Special Orthopedic Surgery and Rheumatic Orthopedics at the University Hospital Frankfurt am Main.
Qualifications
- 1992 Board certification in Surgery.
- 1992 Additional qualification in Emergency Medical Care.
- 1993 Specialization in Trauma Surgery.
- 1996 Additional qualification in Hand Surgery.
- 2000 Additional qualification in Physiotherapy.
- 2005 Board certification in Orthopedics and Trauma Surgery.
- 2010 Additional qualification in Sports Medicine.
Clinical and Research Interests
- Translational research on polytrauma: early diagnosis of systemic inflammatory response syndrome, microcirculation disorders, and organ failure.
- Experimental and clinical trials on bone regeneration and stem cell therapy.
- Wound healing, tissue reconstruction and infection monitoring.
- Injuries in children.
- Spinal injuries.
Memberships in Professional Societies and Organizations
- 2009 - 2014 Head of the Scientific Committee of the German Trauma Society (DGU).
- 2011 President of the Section of Fundamental Research of the German Society for Orthopaedics and Trauma Surgery (DGOU).
- 2011 President of the European Society for Trauma and Emergency Surgery (ESTES).
- 2014 Congress President of the World Trauma Congress (WTC).
- Since 2015 Board Member of the German Trauma Society (DGU).
- 2017 President of the German Society for Orthopaedics and Trauma Surgery (DGOU).
- 2017 President of the German Trauma Society (DGU).
- German Working Group on Arthroplasty.
- German Society of Surgery (DGCH).
- German Interdisciplinary Association for Intensive Care and Emergency Medicine (DIVI).
- Professional Association of German Surgeons (BDC).
- Association of Southern German Orthopedists and Trauma Surgeons (VSOU).
- European Shock Society (ESS).
- European Society for Trauma and Emergency Surgery (ESTES).
- Euroacademia Multidisciplinaria Neurotraumatologica (EMN).
- Association for Orthopedic Research (AFO).
Photo of the doctor: (c) Universitätsklinikum Frankfurt
About hospital
According to the reputable Focus magazine, the University Hospital Frankfurt am Main ranks among the top German medical facilities!
The hospital was founded in 1914 and today is a well-known German medical facility, which combines rich traditions and scientific innovations. A medical team of more than 6,500 employees cares about the health of patients around the clock, ensuring them with the highest standards of medical care and best possible safety.
The hospital has 32 specialized departments and more than 20 research institutes, which have all the necessary resources for the provision of the most effective care for any patient. The hospital has 1,488 beds for inpatient medical care. The medical facility diagnoses and treats more than 51,000 inpatients and about 44,800 outpatients every year. Due to the demonstration of outstanding treatment results, the number of patients seeking medical care here increases significantly annually.
The hospital presents all areas of modern medicine, whereas its special competence lies in neuroscience, oncology, cardiovascular medicine, cardiac surgery and other fields. Many treatment methods available here are unique not only in Europe, but also internationally.
Photo: (c) depositphotos
Accommodation in hospital
Patients rooms
The patients of the University Hospital Frankfurt am Main live in comfortable rooms made in modern design and meeting the highest standards of European medicine. Each room is equipped with an ensuite bathroom with a toilet and a shower. The standard room includes a comfortable, automatically adjustable bed, a bedside table, a wardrobe, a table and chairs for receiving visitors and a TV. If desired, patients can use Wi-Fi. The patients can also stay in the enhanced-comfort rooms.
Meals and Menus
The patient and his accompanying person have a daily choice of three menus. If for any reason you do not eat all the food, you will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to the treatment.
Further details
Standard rooms include:
Religion
Religious services are available upon request.
Accompanying person
During the inpatient program, an accompanying person may stay with you in a patient room or in a hotel of your choice.
Hotel
During the outpatient program, you may stay in a hotel of your choice. Managers will help you choose the most suitable options.