The program includes:
- Initial presentation in the clinic
- clinical history taking
- physical examination
- review of medical records
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- indicators of inflammation (CRP, ESR)
- indicators blood coagulation
- x-ray examination of the hip
- MRI scan of the hip
- preoperative care
- hip replacement (hip endoprosthesis)
- symptomatic treatment
- control examinations
- physiotherapeutic procedures
- orthopedic appliances
- the cost of essential medicines and materials
- nursing services
- full hospital accommodation
- explanation of future recommendations
The program includes orthopedic rehabilitation:
- Primary presentation in the clinic
- medical history, including family history
- complex neurological and orthopedic examinations
- X-ray examination
- complex neurophysiological examinations
- individual rehabilitation program, which includes:
- Wii Fit training in the use of the balance
- neuropsychological therapy
- functional therapy of the upper extremities (ArmeoSpring)
- kinesitherapy (physiotherapy)
- biocontrol with feedback
- healing deep muscle massage
- acupuncture of spasticity and pain syndromes
- occupational therapy
- psycho-educational classes
- Individual physiotherapy
- microcurrent treatment
- fangotherapy / cryotherapy
- antispasmodic drug therapy
- mobilization of limb joints
- hydrotherapy / massage therapy / reflexology
- training on special trainers
- and etc.
- nurses care
- stay in the hospital with full board
- symptomatic and drug therapy
How program is carried out
Preliminary preparation for hip replacement includes quitting smoking and drinking alcohol; cancelling non-steroidal anti-inflammatory drugs (diclofenac, ibuprofen); cancelling anticoagulants (warfarin); normalization of body mass, if possible.
Preoperative examination, including consultation with an anesthesiologist and necessary related specialists, takes 1-2 days. According to its results, the most suitable endoprosthesis is selected.
Hip replacement. The operation is performed under general anesthesia. The patient lies on his side, the affected leg is bent and fixed in this position. The surgeon makes an incision 15-20 cm long, minimally traumatizing the muscles and nerve endings. Through this incision, miniature instruments are inserted to remove the damaged joint structures. Healthy bone is adjusted for further reliable implant fixation.
The surgeon installs a femoral stem in the center of the upper part of the femur. Ball-shaped head of the joint is fixed on it. The surgeon also implants a special liner that facilitates movement of the leg and protects the structures of the prosthesis. After the primary fixation of the prosthesis components, the doctor assesses the joint range of motion, as well as the length and symmetry of the lower limb.
The implant is fixed with cement or cementless method. The doctor treats the operating field with antiseptics, conducts its final revision and sutures the wound layer by layer. A temporary drainage is installed in the joint, and a bandage is applied on top.
Postoperative care. During the first day after the intervention the patient stays in the intensive care unit, under round-the-clock medical supervision. After that, with a smooth course of the postoperative period, the patient is transferred to a regular ward and the drains are removed. The range of motion expands gradually, from light toes movements to walking. Walking with the use of walking aids is allowed in 3-5 days after the operation.
Rehabilitation. The rehabilitation program begins after the transfer of the patient from the intensive care unit to a regular ward. It includes physical activity (from exercises in bed in the early days to exercises in the gym), physiotherapy, massage (including lymphatic drainage), exercises in the water. The rehabilitation program is constantly being adjusted according to the needs of the patient.
Required documents
- X-ray examination of the hip joints
- MRI scan of the hip joints, if available
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
The Department of Adult and Pediatric Trauma, Hand, Reconstructive Surgery at the University Hospital Jena offers all modern surgical interventions in these medical fields. The department specializes in the treatment of patients with polytrauma, pelvic surgery, endoprosthetics, cancer, reconstructive surgery and hand surgery. The department has 62 beds for inpatient treatment and 3 high-tech operating rooms for both planned and emergency operations. The prestigious certificates of the Interregional Trauma Center of the German Society of Traumatology and the EndoCert certificate testify to the outstanding quality of medical services.The Chief Physician of the department is Prof. Dr. med. Gunther Hofmann.
In addition to the surgical treatment, the department’s arsenal includes conservative treatment methods, for example, drug therapy, physiotherapy and occupational therapy. All of these measures also play a key role in achieving an optimal treatment outcome. After the surgery, during a hospital stay, the patient undergoes an individually developed rehabilitation program aimed at the best possible mobilization. The rehabilitation is indicated for patients after accidents and their complications, as well as after surgical treatment of congenital and acquired pathologies.
As a certified Endoprosthetics Center (EndoCert), the department provides the full range of partial and total knee, hip, shoulder, elbow, wrist, and finger joint replacement surgeries. Also, the department's surgeons have exceptional experience in the field of revision interventions on the joints, for example, in degenerative processes, infection, etc. The minimally invasive techniques and navigation systems are widely used in joint replacement surgeries, which contributes to sparing treatment and faster recovery of the patient.
Another important focus of the department’s work is hand surgery. In this field, it offers all modern interventions, including microsurgery of the vessels, nerves and tendons, plastic surgery in soft tissue defects. The department's surgeons provide primary and specialized medical care for hand injuries of varying severity. The department has a specialized hand replantation team, which works around the clock. The department also specializes in surgery to treat severe hand injuries and congenital hand defects.
The department's competence also includes the treatment of injuries of varying severity (certification as a supraregional Trauma Centre). It is worth noting that the department has achieved outstanding results in this field and guarantees the highest quality of treatment even in the most complex clinical cases.
The main clinical focuses of the department include:
- Treatment of injuries of varying severity, including polytrauma
- Treatment of pelvic bone injuries and their complications
- Surgical navigation
- Pelvic bone surgery
- Femoral fracture surgery
- Joint replacement surgery
- Surgery using 3D image conversion system
- Comminuted ankle fracture
- Fracture of the upper articular surface of the tibia
- Complicated foot fractures
- Complicated wrist fractures
- Ankle bone fractures
- Calcaneal fractures
- Hand surgery and replantation surgery
- Emergency surgery
- Amputation
- Fractures and dislocations of the hand and wrist of all degrees of severity
- Injuries to the vessels, nerves and tendons
- Hand infections (soft tissue and bone infections)
- Secondary reconstructive interventions
- Plastic surgery to close soft tissue defects (plastic surgery using free, tube grafts)
- Tandon surgery
- Arthrolysis, tenolysis, tendon plastic surgery
- Corrective osteotomy of the hand and forearm
- Aseptic bone necrosis therapy (for example, lunate bone, scaphoid bone)
- Treatment of finger, wrist osteoarthritis
- Arthroplasty, partial arthrodesis, arthrodesis, joint replacement surgery in arthrosis or posttraumatic complications
- Emergency and secondary brachial plexus reconstruction
- Denervation and reconstruction of the nerve endings
- Operations in rheumatic hand lesions
- Treatment of nerve compression syndromes in the forearm and hand
- Operations to restore hand mobility in nerve lesion
- Treatment of spastic contractures
- Secondary reconstructive procedures after finger amputation (stump extension, callus distraction, finger transposition, etc.)
- Hand surgery in children, including severe hand injuries and deformities
- Emergency surgery
- Knee, hip, shoulder, elbow, wrist and finger joint endoprosthetics
- Foot surgery
- Arthroscopic surgery
- Treatment of diabetic foot syndrome
- Treatment of osteochondral lesions
- Correction of deformity of the hindfoot and foot arch
- Treatment of clubfoot, claw foot, cavus foot
- Forefoot deformity correction
- Correction of the foot with a flat transverse arch, hallux valgus, little toe defects
- Transplantation and regeneration of cartilage tissue
- Intraoperative use of navigation and 3D imaging techniques
- Surgical interventions in rheumatic foot lesions
- Treatment of foot injuries
- Soft tissue surgery
- Ganglion treatment
- Compression syndromes (tarsal tunnel syndrome)
- Achilles tendon reconstruction
- Ligament reconstruction
- Reconstructive surgery and hindfoot replacement
- Surgical treatment of benign and malignant bone and soft tissue tumors (special focus on the treatment of sarcomas), secondary bone tumors (bone metastases)
- Other medical services
Curriculum vitae
Prof. Hofmann attended Medical School, passed a state examination and obtained a doctorate from the Ludwig Maximilian University of Munich. Thereafter, he moved to the Technical University Munich, wherefrom he graduated in 1984 with a Dr. rer. nat. (Doctor rerum naturalium) in Physics.
In 1987, Dr. Hofmann commenced work as a Research Fellow at the University Hospital of the Ludwig Maximilians University of Munich until he started his habilitation in 1992. During his habilitation, Prof. Hofmann did research at the Massachusetts General Hospital in Boston, Massachusetts, and started to work at the University Hospital of the Ludwig Maximilians University of Munich in the same year. In 1995, he moved to the BG Trauma Hospital in Murnau. Since 2004, Prof. Hofmann has been the Medical Director of the Bergmannstrost Hospital Halle, Saxony-Anhalt and the Head of the Department of Adult and Pediatric Trauma, Hand, Reconstructive Surgery at the University Hospital Jena, Thuringia.
Research Focuses
- Development of implants for osteosynthesis and joint replacement surgery.
- Bone and joint grafting.
- Biomaterials.
- Biomechanics.
- Computer-assisted surgery.
- Bone infections.
Awards
- 1986 Otto Goetze Award of the Association of Bavarian Surgeons.
- 1997 Herbert Stiller Award of the Physicians Against Animal Experiments.
- 2008 Science4Life Venture Cup for the development of an optical system for the detection of osteoarthritis (Team: arthrospec AG).
Photo of the doctor: (c) Universitätsklinikum Jena
About hospital
According to the prestigious Focus magazine, the University Hospital Jena regularly ranks among the top German medical facilities!
The hospital has positioned itself as a multidisciplinary medical facility with a long history of more than 200 years. Since its foundation, the hospital has been constantly developing and modernizing, thanks to which nowadays it offers patients the highest level of treatment in Germany based on the use of innovative technologies and the very latest therapeutic techniques. The hospital consists of 26 specialized departments and 25 research institutes. It treats more than 53,600 inpatients and about 274,000 outpatients every year. The staff of the hospital includes more than 5,600 competent doctors.
The extensive resources of the university hospital, high treatment standards, and the introduction of new research developments provide first-class treatment in Germany meeting the stringent international standards. The hospital has an excellent reputation not only in Germany, but also far beyond its borders, due to which it accepts a large number of foreign patients for the diagnostics and treatment.
Despite the technical progress and the availability of accurate computerized systems, the patient’s physical health and emotional state is the main value of each employee of the hospital, since some diagnoses cause emotional distress in patients. The doctors of the hospital believe that the key to a successful result is a comprehensive and individual approach, so they spend a lot of time talking with patients, listen carefully to all their wishes and support at all stages of the therapeutic process. All this in combination with high-precision diagnostic techniques and the very latest types of therapy forms a solid basis for the achievement of an optimal treatment result.
Photo: (c) depositphotos
Accommodation in hospital
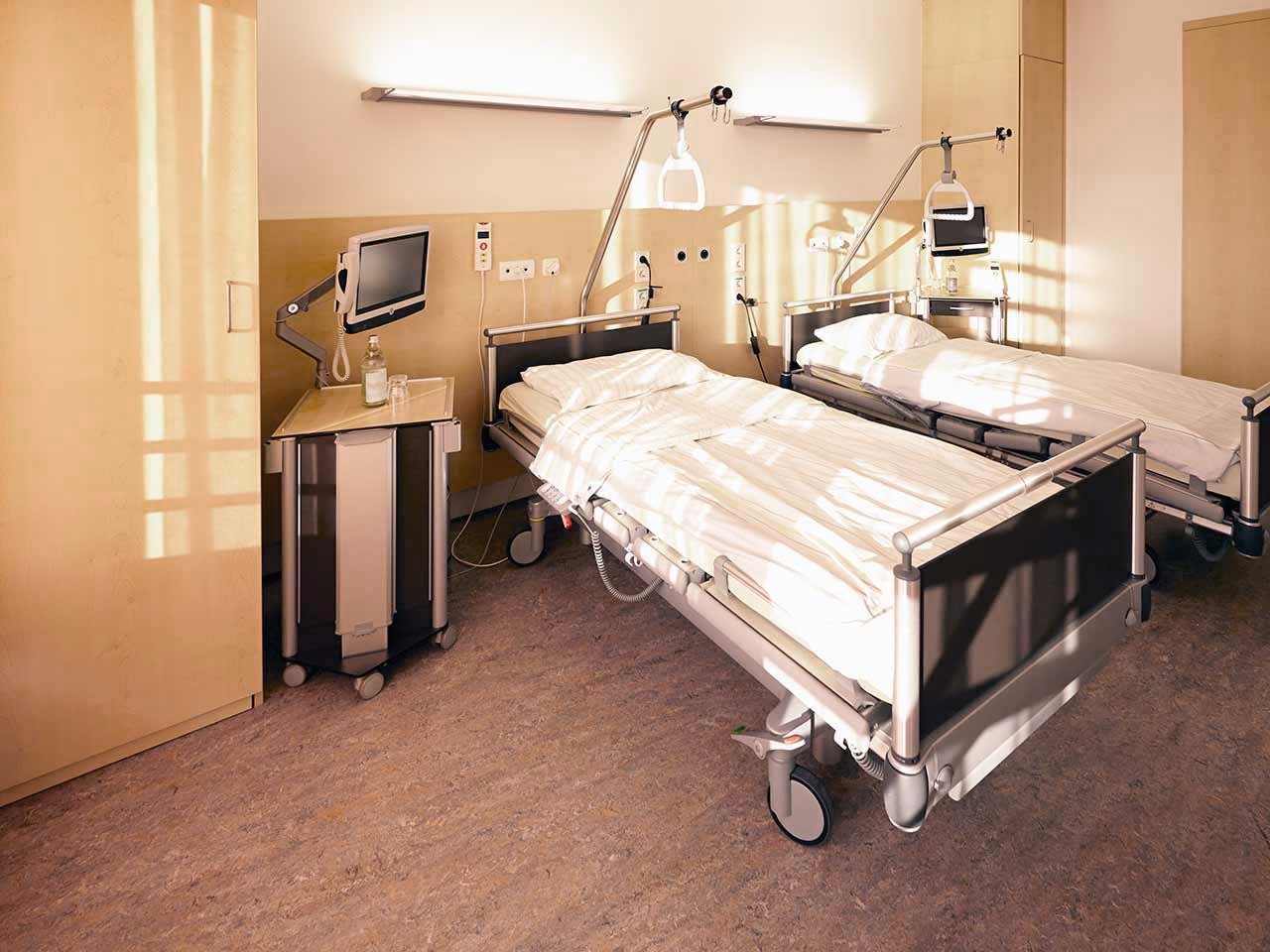
Patients rooms
The patients of the University Hospital Jena live in comfortable single and double rooms made in a modern design. Each patient room is equipped with an ensuite bathroom with shower and toilet. The room has enough space to store personal belongings, as well as a table and chairs for receiving visitors. A bedside table can be converted into a table so that patients can eat right in their bed. Each room has a TV, and there is also access to the Internet. In addition, the hospital offers enhanced-comfort rooms.
Meals and Menus
The patient and his accompanying person have a daily choice of three menus. If for some reason the patient does not eat all the foods, he will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to the treatment.
Further details
Standard rooms include:
Religion
Religious services are available upon request.
Accompanying person
During the inpatient program, an accompanying person may stay with you in a room or at the hotel of your choice.
Hotel
During the outpatient program, you can live at a hotel of your choice. Managers will help you to choose the most suitable options.