The program includes:
- Initial presentation in the clinic
- clinical history taking
- review of medical records
- physical examination
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- inflammation indicators (CRP, ESR)
- indicators blood coagulation
- CT/MRI scan
- neuropsychological tests (on indications):
- ENMG (electroneuromyography)
- EEG (electroencephalography)
- SEPs (somatosensory evoked potentials)
- VEPs (visually evoked potentials)
- BAEP tests (brainstem auditory evoked potential)
- motor symptoms
- reflexes
- muscle strength
- Muscle tone
- coordination
- balance
- sensory symptoms
- sense of touch
- vision and eye movement
- hearing
- psychiatric symptoms
- mental status
- mood
- neuropsychological testing
- memory
- reasoning
- mental agility
- language function
- spatial reasoning
- psychiatric evaluation
- emotional state
- patterns of behaviors
- quality of judgment
- coping skills
- signs of disordered thinking
- vidence of substance abuse
- consultation of related specialists
- symptomatic specific treatment
- the cost of essential medicines and materials
- nursing services
- control examinations
- full hospital accommodation
- developing of further guidance
Required documents
- Medical records
- Genetic tests (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
The Department of Neurology and Epileptology at the University Hospital Ulm offers comprehensive diagnostics and effective treatment of diseases of the central and peripheral nervous systems. The department's team of doctors has long experience in the medical care of patients with Parkinson's disease, multiple sclerosis, amyotrophic lateral sclerosis, epilepsy, dementia, neuromuscular diseases, brain and spinal cord tumors, stroke, and other pathologies. The department has state-of-the-art diagnostic equipment for comprehensive diagnostics of the nervous system and assessment of the patient's neurological status. During the therapeutic process, doctors use individually developed treatment regimens, including drug therapy, physiotherapy, therapeutic exercises, occupational therapy, and other methods. The department also houses an outpatient clinic specializing in botulinum toxin injection therapy for dystonia, spastic paralysis, sialorrhea (excessive salivation), and hyperhidrosis (excessive sweating). Medical care includes not only primary care, and the department has a specially trained team for follow-up rehabilitation, including measures for occupational and home reintegration. High-precision medical equipment for diagnostics and therapy, combined with the rich clinical experience of the department’s doctors, is the key to high treatment success rates and the excellent reputation of the medical institution at the national and international levels. The Head Physician of the department is Prof. Dr. med. Georg Bernhard Landwehrmeyer.
The department is one of the few medical facilities in Germany that has gained vast experience in the medical care of patients with amyotrophic lateral sclerosis (ALS). This neurological disease occurs due to lesions of the motor neurons in the brain and spinal cord. Patients with ALS suffer from severe motor function disorders: they cannot walk, move their hands and fingers, or perform other similar actions. ALS is characterized by constant progression. Over time, movement restrictions are complemented by paresis of the respiratory muscles. The exact causes of the development of this neuropathology are still unknown. In many cases, specific genetic mutations trigger the condition. Diagnostics for suspected amyotrophic lateral sclerosis include a variety of laboratory tests, neurophysiological studies, brain and spinal cord MRI scans, and a lumbar puncture. Unfortunately, there are no effective methods for a complete cure of ALS, but the department's neurologists have at their disposal effective methods to control the pathology, prolong the patient's life, and ensure a high quality of life. The first-line treatment is drug therapy to relieve symptoms and slow disease progression. Medication intake may be complemented by therapeutic massage, physiotherapeutic procedures, thermal procedures, hydrotherapy, and other treatment methods.
An important focus of the department's clinical activities is the treatment of Parkinson's disease and other movement disorders. Parkinson's disease is one of the most common neurological disorders that affect elderly people. The main manifestations of the disease include limb tremors, stiffness, eyelid, tongue, and lower jaw twitching, balance and coordination impairments, memory, attention, and concentration disorders, depression, anxiety, sleep problems, and excessive salivation. If Parkinson's disease is suspected, the department's specialists study the patient's medical history, listen to their complaints, carry out a physical examination, neurophysiological studies, and imaging examinations of the brain (CT and MRI scans). Dopamine level testing is mandatory because movement disorders in Parkinson's disease are largely due to a deficiency of this neurotransmitter. After a comprehensive examination and making an accurate diagnosis, the department's neurologists proceed with treatment, the main goal of which is to alleviate symptoms and improve the quality of life of the patient. The therapy is based on the prescription of drugs that increase dopamine levels in the brain, thereby eliminating tremors and improving motor functions. Drug therapy is supplemented by physiotherapeutic procedures, occupational therapy, and speech therapy (if the patient has some speech disorders). An important role is given to a healthy diet, normal sleep, and regular, moderate physical activity. If the implementation of the above-mentioned therapeutic measures does not yield the desired result, the possibility of deep brain stimulation may be considered. The procedure is performed in collaboration with neurosurgeons. Its essence lies in stimulating certain areas of the brain with electrical impulses, which can significantly alleviate symptoms of Parkinson's disease such as tremors, stiffness, and slowness of movement.
The medical facility also admits patients with epilepsy. This is a chronic brain condition characterized by seizures resulting from increased electrical activity of the brain neurons. During the diagnostics of a patient with suspected epilepsy, it is important for the department's specialists to obtain information about the frequency, intensity, and duration of epileptic seizures. An integral part of the diagnostic process is electroencephalography (EEG), during which the electrical activity of the brain is recorded. In most cases, a brain MRI scan is also performed. A treatment regimen for confirmed epilepsy is developed individually. The specialists mostly use only drug therapy with anticonvulsants. If such treatment fails, vagus nerve stimulation may be carried out. This method significantly reduces the frequency and intensity of epileptic seizures, and in some cases, it can even ensure their complete disappearance. The last-line treatment is a surgical intervention, which is the responsibility of neurosurgeons.
The department's clinical focuses include the following:
- Diagnostics and treatment of amyotrophic lateral sclerosis
- Diagnostics and treatment of Parkinson's disease
- Diagnostics and treatment of epilepsy
- Diagnostics and treatment of restless legs syndrome
- Diagnostics and treatment of tremor
- Diagnostics and treatment of dementia
- Diagnostics and treatment of Huntington's disease
- Diagnostics and treatment of multiple sclerosis
- Diagnostics and treatment of neuromuscular diseases
- Diagnostics and treatment of brain and spinal cord tumors
- Diagnostics and treatment of neurofibromatosis
- Diagnostics and treatment of stroke
- Diagnostics and treatment of neuro-urological disorders (in collaboration with urologists): urinary incontinence, overactive bladder, and neurogenic bladder
- Diagnostics and treatment of dizziness
- Diagnostics and treatment of chronic headaches
- Diagnostics and treatment of swallowing disorders due to neurological diseases
- Diagnostics and treatment of Gilles de la Tourette syndrome
- Diagnostics and treatment of Phelan-McDermid syndrome
- Diagnostics and treatment of dystonia
- Diagnostics and treatment of spastic paralysis
- Diagnostics and treatment of other neurological diseases
Curriculum vitae
Prof. Dr. med. Georg Bernhard Landwehrmeyer is a highly qualified neurologist and one of the most experienced specialists in Germany in the treatment of Huntington's disease. He co-founded the European Huntington's Disease Network (EHDN) in 2004 and served as a Chairman of its Executive Committee until 2014. Dr. Landwehrmeyer is the Head Physician of the Department of Neurology and Epileptology at the University Hospital Ulm.
Prof. Landwehrmeyer graduated from the University of Freiburg, where he completed a residency in neurology, a research fellowship in neuropathology and molecular pharmacology, and a residency in psychiatry. The specialist trained in prestigious foreign hospitals, including the Royal Victoria Hospital in Belfast and the Canton Hospital St. Gallen in Basel. From 1993 to 1995, Dr. Landwehrmeyer served as a Postdoctoral Fellow at Massachusetts General Hospital, Harvard Medical School. From 1995 to 1999 he worked as a Member of the Department of Neurology and Psychiatry at the Albert Ludwig University of Freiburg. In 2000, he became a professor.
Prizes, Awards, and Honors
- 1980 - 1988 Scholarship by the German Academic Exchange Service.
- 1990 - 1991 Training Award by the German Research Foundation (DFG).
- 1993 - 1994 Research Prize by the German Research Foundation (DFG).
- 1994 - 1997 Research Award by the European Commission, Network of Excellence in Neural Networks.
- 2001 - 2004 Research Award by the European Commission, Neuroprotection & Natural History in Parkinson Plus Syndromes (NNIPPS).
- 2010 - 2013 Research Award by the European Commission, Pharmacodynamic Approaches to Demonstration of Disease-Modification in Huntington's Disease by SEN0014196.
Photo of the doctor: (c) Universitätsklinikum Ulm
About hospital
The University Hospital Ulm is an advanced medical complex that provides patients with high-class medical care using the very latest scientific achievements. The medical facility has been performing successful clinical activities for more than 40 years and has long earned an excellent reputation throughout Europe. The hospital regularly demonstrates high treatment success rates, takes an active part in the training of medical students, and works tirelessly on promising research projects.
The university hospital consists of 29 specialized departments and 16 scientific institutes, where more than 7,000 highly qualified employees work for the benefit of their patients. More than 55,000 inpatients and about 300,000 outpatients are treated here every year. The hospital has 1,274 beds. The medical team of the hospital is focused on providing personalized medical services using the most modern and sparing diagnostic and treatment methods.
The University Hospital Ulm is the largest medical complex in the region, and practically all areas of modern medicine are represented here. Transplantology and oncology are among the priority areas of clinical activity in the medical facility. The hospital holds leading positions in the world in bone marrow transplantation. In addition, the hospital has advanced experience in cancer treatment. The Comprehensive Cancer Center is recognized as the leading facility of this kind in the country, and it is certified by the German Cancer Society (DKG). It provides effective treatment for various types of cancer. The center also offers innovative CAR T-cell therapy. In addition, the Cancer Center is actively engaged in research activities to improve available treatment methods and develop innovative therapeutic techniques to fight cancer.
Along with the use of advanced technologies, doctors show respect, understanding, and a humane attitude toward the patient. The medical team includes competent psychologists, who are always ready to provide assistance and support to the patients and their families during the therapeutic process.
Photo: (с) depositphotos
Accommodation in hospital
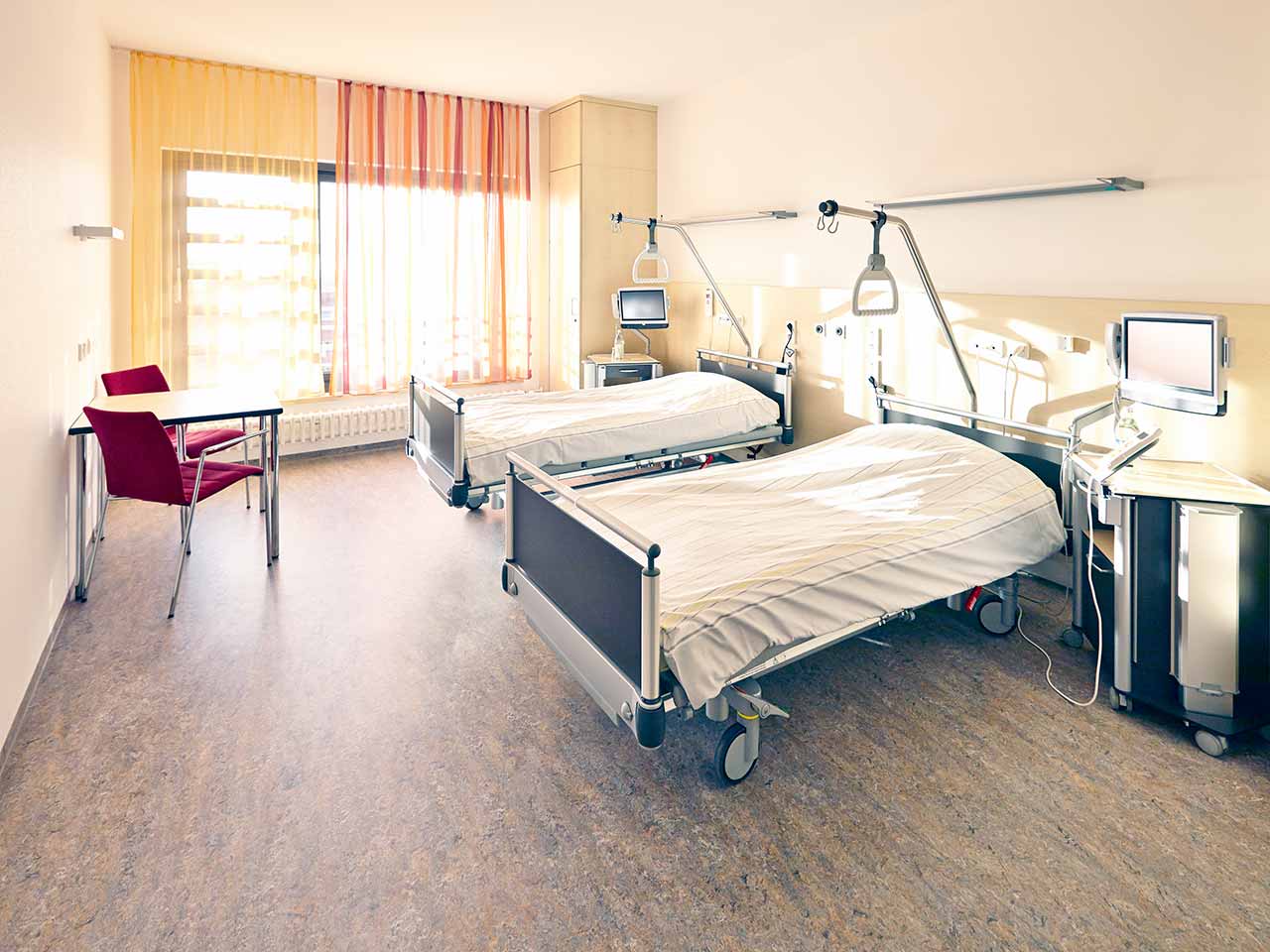
Patients rooms
The patients of the University Hospital Ulm live in comfortable single and double rooms with a modern design and light colors. All patient rooms have an ensuite bathroom with a toilet and a shower. The patient room furnishings include a comfortable automatically adjustable bed, a bedside table, a wardrobe, a table and chairs, a telephone, a radio, and a TV. Wi-Fi access is also available in patient rooms.
The hospital also offers enhanced-comfort rooms, which additionally have a safe, a refrigerator, and upholstered furniture. The bathroom in the enhanced-comfort room has changeable towels, a cosmetic mirror, a hairdryer, and toiletries.
Meals and Menus
Patients and their accompanying person are offered three meals a day: breakfast, lunch, and dinner. The patient and accompanying person have a choice of three menus every day, including a vegetarian menu. Patients staying in the enhanced-comfort rooms are also offered light snacks, fruits, desserts, and hot and cold drinks in the comfortable lounge area.
If, for some reason, you do not eat all the foods, you will be offered an individual menu. Please inform the medical staff about your dietary preferences prior to treatment.
Further details
Standard rooms include:
![]() Shower
Shower
![]() Toilet
Toilet
![]() Wi-Fi
Wi-Fi
![]() TV
TV
Religion
The hospital has a chapel where Catholic and Protestant services are held weekly. The services are also broadcast on the internal television channel of the hospital. The chapel is open 24 hours a day for visits and prayers.
The services of other religious representatives are available upon request.
Accompanying person
Your accompanying person may stay with you in your patient room or at the hotel of your choice during the inpatient program.
Hotel
You may stay at the hotel of your choice during the outpatient program. Our managers will support you for selecting the best option.