The program includes:
- Initial presentation in the hospital
- Clinical history taking
- Review of available medical records
- Physical examination
- Laboratory tests:
- Complete blood count
- General urine analysis
- Biochemical analysis of blood
- Tumor markers
- Inflammation indicators (CRP, ESR)
- Coagulogram
- Ultrasound scan
- CT scan / MRI
- Preoperative care
- Embolization or chemoembolization, 2 procedures
- Symptomatic treatment
- Cost of essential medicines
- Nursing services
- Elaboration of further recommendations
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examination, such as the assessment of liver and kidney function, ultrasound scan, CT scan and MRI. This will allow the doctor to determine which vessels are feeding the tumor and its metastases, as well as determine how well you will tolerate the procedure.
Chemoembolization begins with local anesthesia and catheterization of the femoral artery. The thin catheter is inserted through a few centimeters long incision of the blood vessel. The doctor gradually moves the catheter to the vessel feeding the primary tumor or its metastases. The procedure is carried out under visual control, an angiographic device is used for this. The vascular bed and the position of the catheter in it are displayed on the screen of the angiograph.
When the catheter reaches a suspected artery, a contrast agent is injected through it. Due to the introduction of the contrast agent, the doctor clearly sees the smallest vessels of the tumor and the surrounding healthy tissues on the screen of the angiograph. After that, he injects emboli into the tumor vessels through the same catheter.
Emboli are the spirals or the liquid microspheres. The type of embolus is selected individually, taking into account the diameter of the target vessel. When carrying out chemoembolization, a solution of a chemotherapy drug is additionally injected into the tumor vessel. Due to the subsequent closure of the vessel lumen with an embolus, the chemotherapy drug influences the tumor for a long time. In addition, the drug does not enter the systemic circulation, which allows doctors to use high doses of chemotherapeutic agents without the development of serious side effects. Chemoembolization leads to the destruction of the tumor or slowing down its progression.
After that, the catheter is removed from the artery. The doctor puts a vascular suture on the femoral artery and closes it with a sterile dressing. During chemoembolization, you will be awake. General anesthesia is not used, which significantly reduces the risks of the procedure and allows performing it on an outpatient basis, avoiding long hospital stay.
After the first procedure, you will stay under the supervision of an interventional oncologist and general practitioner. If necessary, you will receive symptomatic treatment. As a rule, a second chemoembolization procedure is performed in 3-5 days after the first one in order to consolidate the therapeutic effect. After that, you will receive recommendations for further follow-up and treatment.
Required documents
- Medical records
- MRI/CT scan (not older than 3 months)
- Biopsy results (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
The Department of Interventional Radiology at the Helios Hospital Hildesheim provides the full range of medical services in the area of its specialization. The team of the department's doctors specializes in diagnostic and therapeutic image-guided interventional procedures. The doctors have at their disposal the most advanced imaging devices, including X-ray systems, ultrasound devices, equipment for computed tomography and magnetic resonance imaging. In most cases, the department's specialists perform interventions on the vessels, and therefore doctors from the Department of Vascular Surgery are often involved in the therapeutic process. The use of state-of-the-art equipment allows the patients to get rid of pathological changes in the vessels of any part of the body, excluding open invasive surgery with its high risks. The department's medical staff has excellent qualifications and vast clinical experience, so patients confidently trust their health to real professionals. The Chief Physician of the department is Dr. med. Jörg Werhand.
Every day, the department's doctors carry out image-guided catheter procedures to eliminate stenosis and vascular obstruction, which, if not treated promptly, can even lead to death. The most effective therapeutic interventions in this area are balloon dilation and stent implantation. The treatment is quite often carried out on an outpatient basis. In some cases, for example, when carrying out interventions on the carotid arteries, the patient still needs a short hospitalization.
The department's therapeutic offer is complemented by other image-guided procedures. These are tissue sampling (biopsy), punctures, placement of drains, pain therapy for chronic back pain (periradicular therapy, facet joint block).
Another important focus of the department's specialists is the interventional treatment of tumors. The department's specialists perform embolization for the treatment of benign and malignant tumors. This is a minimally invasive catheter procedure, during which the doctor occludes (closes) the blood vessels supplying the tumor. The procedure helps to reduce the size of the tumor or slow down its growth, thereby increasing the effectiveness of further therapeutic measures (chemotherapy, surgery, etc.). In addition, the operation is accompanied by significantly less blood loss after embolization.
The department's range of medical services includes:
- Interventions to eliminate vascular stenosis and obstruction
- Percutaneous transluminal angioplasty
- Stent implantation
- Thrombolysis
- Thrombectomy
- Embolization of blood vessels to arrest haemorrhage, treat uterine fibroids, etc.
- Chemoembolization
- Radiofrequency ablation
- Implantation of port systems
- Aortic replacement surgery for aneurysms
- Biliary drainage
- Percutaneous transhepatic cholangiodrainage
- Stent implantation
- Pain therapy for chronic back pain
- Periradicular therapy
- Facet joint block
- Puncture treatment of false aneurysms of the femoral arteries using thrombin injections
- Other image-guided interventional procedures
Curriculum vitae
Higher Education and Professional Career
- Study of Human Medicine at the Universities of Mainz and Tuebingen.
- 1992 Admission to medical practice.
- 1993 Doctoral Degree in Medicine.
- Since 1993 Residency in the Department of Diagnostic and Interventional Radiology at the hospitals in Schaffhausen, Marburg, Duisburg and Paderborn.
- Attending Physician at the hospitals in Hildesheim and Hanover.
- 1996 Board certification in Diagnostic and Interventional Radiology.
- Since October 2005 Chief Physician of the Department of Interventional Radiology at the Helios Hospital Hildesheim.
Clinical Interests
- Therapeutic interventions on the vessels.
- Interventional diagnostics of the breast.
- Diagnostic imaging: computed tomography and magnetic resonance imaging.
Memberships in Professional Societies
- German Radiological Society.
- European Society of Radiology.
- Cardiovascular and Interventional Radiological Society of Europe.
- European Board of Interventional Radiology.
Photo of the doctor: (c) Helios Kliniken GmbH
About hospital
The Helios Hospital Hildesheim positions itself as an advanced provider of high-quality medical services at the European level. The medical facility is an Academic Hospital of the Hannover Medical School, thanks to which it can successfully introduce the very latest medical achievements into clinical practice. The hospital is distinguished by the excellent quality of diagnostics, highly effective treatment of pathologies of any severity and the best patient care based on understanding and humane attitude. The history of the medical complex dates back to 1838, so it carefully honors traditions, but at the same time the hospital actively uses innovative diagnostic and treatment methods. The medical team of the hospital consists of more than 1,450 people. The hospital employs highly qualified doctors who are rightfully proud of their treatment outcomes.
The medical facility has 579 beds. The team of doctors working at the hospital treats more than 28,000 inpatients and about 80,000 outpatients every year. The patients from foreign countries often undergo diagnostics and treatment in the hospital, which confirms the excellent reputation of the medical center in the international arena.
The hospital offers highly specialized departments with different medical focuses, including oncology, cardiology, gastroenterology, gynecology, dermatology, otolaryngology, general and abdominal surgery, plastic and aesthetic surgery, traumatology, etc. Many medical fields are awarded with prestigious certificates, including German Cancer Society (DKG) certification, IQM certification, and others.
Photo: (с) depositphotos
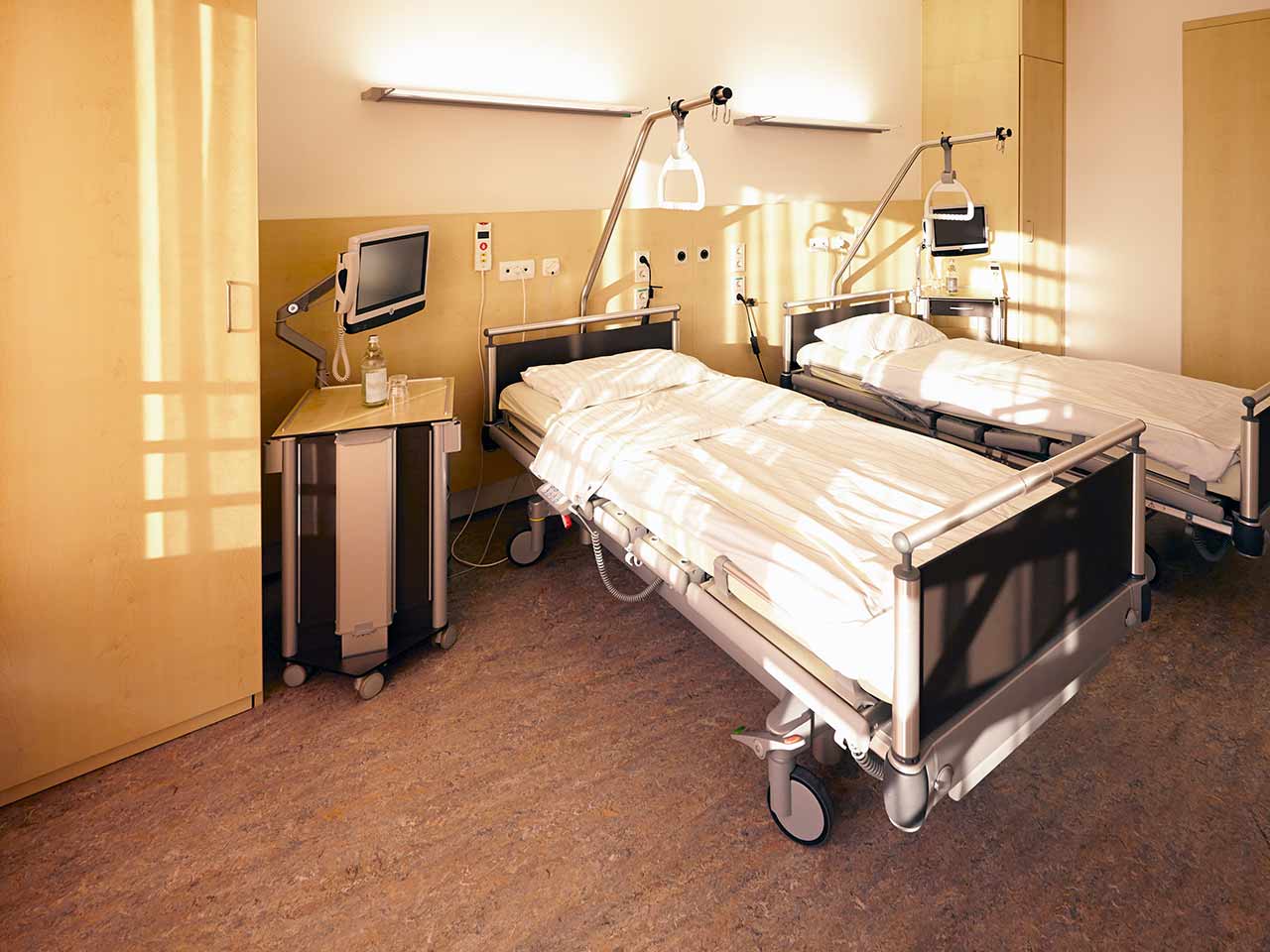
Accommodation in hospital
Patients rooms
The patients of the Helios Hospital Hildesheim live in spacious and light rooms. The furnishings of a standard patient room includes an automatically adjustable bed with an orthopedic mattress, a bedside table, and a wardrobe for storing things. All patient rooms have telephone, radio and TV, as well as free Wi-Fi. For maximum convenience of patients, each room has an ensuite bathroom with shower and toilet.
If desired, the patient can stay in an enhanced-comfort room. Such rooms are distinguished by a more sophisticated design, and are additionally equipped with a safe, a minifridge and upholstered furniture.
Meals and Menus
The patients of the hospital are offered tasty and varied meals. Diet and vegetarian menus are also available. If the patient follows a special diet recommended by the attending physician, he will be provided with food cooked from approved products.
Breakfast is served buffet style: eggs, various types of cheese, sausage, buns, jam, vegetables. There are three set menus to choose from for lunch. Dinner is also served buffet style.
In addition, the hospital has a cozy cafe called Leckeria where one can have a delicious snack. The range of dishes includes light salads, hearty set meals, snacks, sandwiches, cakes, as well as tea, coffee and soft drinks. The terrace is open in the summertime.
Further details
Standard rooms include:
Television
All patient rooms have a TV set. The TV can be used with headphones – the patients can use their own headphones or ask for the headphones from the staff.
Religion
The patient can talk with a Christian priest at any time. Divine services are held every Sunday at 10 am (on the ground floor).
Other religious services are available upon request.
Accompanying person
During the inpatient program, the accompanying person can stay with the patient in a patient room or at a hotel of his choice. Our managers will help you choose the most suitable option.
Hotel
During the outpatient program, the patient can stay at a hotel of his choice. Our managers will help you choose the most suitable option.