According to MDPI clinical data, melanoma accounts for 1.7% of global cancer diagnoses and is the fifth most common cancer in the US. Melanoma incidence is rising in developed, predominantly fair-skinned countries, growing over 320% in the US since 1975 [1]. That is why it is very important to look for new effective treatments, one of which is immunotherapy.
Melanoma immunotherapy is an innovative method of systemic therapy that complements the conventional protocol at all stages of the disease and can significantly increase treatment success rates, survival rates, and life expectancy. In German hospitals, doctors actively use this type of melanoma treatment in the early stages of the disease. Immunotherapy for metastatic melanoma makes it possible to restrain the progression of the disease and prolong the life of patients. In Germany, more than five groups of immunotherapy treatments are used, each of which is prescribed strictly individually, taking into account the genetic characteristics of the cancer cells, location of the melanoma tumor, and the patient's condition. Among these approaches, dendritic cell vaccines stand out as particularly promising, a groundbreaking discovery that earned scientist Ralph Steinman the 2011 Nobel Prize in Medicine for revolutionizing our understanding of the immune system and how it helps to fight cancer.
Role of Immunotherapy in the Complex Treatment of Melanoma
Immunotherapy treatment for melanoma is part of the complex therapy of this type of oncology. At stages I and II, the melanoma tumor is removed surgically with the capture of 0.5 to 2.0 cm of healthy tissue. If the fingers or auricle are affected, then German surgeons perform modified operations in order to preserve the function of the hand or organ of hearing. After complete healing of the postoperative wound, a course of immunotherapy treatments is prescribed. It is crucial to start treating advanced melanoma or early stages no later than nine weeks after surgery. The goal of melanoma treatment in this clinical situation is to minimize the risk of recurrence caused by residual cancer cells.
When given in the early stages of melanoma, immunotherapy (most often, this is a dendritic cell vaccine) forms a long-term anti-cancer memory. The human immune system stores information about the melanoma cells; if a similar malignant neoplasm reappears in the body, it is quickly destroyed due to the activation of specific T-cells and other immune cells, which generate a strong immune response.
In stage III melanoma, with the involvement of the lymph nodes, doctors additionally remove the lymph nodes, and immunotherapy begins no later than three months after that. The goal of treatment is to destroy the remaining microscopic metastases and ensure complete recovery. Many patients with advanced melanoma at this stage achieve sustained remission when combination therapy with immunotherapy and standard protocols is applied. If the tumor cells are unresectable (this may be in stage III or IV), then melanoma immunotherapy can slow down the further progression of the disease, i.e., the spread of metastases and the destruction of the primary melanoma. In this case, the patient receives immunotherapeutic drugs continuously, and this is the primary type of therapy. In advanced cases, dendritic cell vaccines have proven to be a valuable therapeutic option, offering melanoma patients new hope for treatment. Previously, doctors could offer such patients only chemotherapy, which had severe side effects.
Types of Immunotherapy for Melanoma
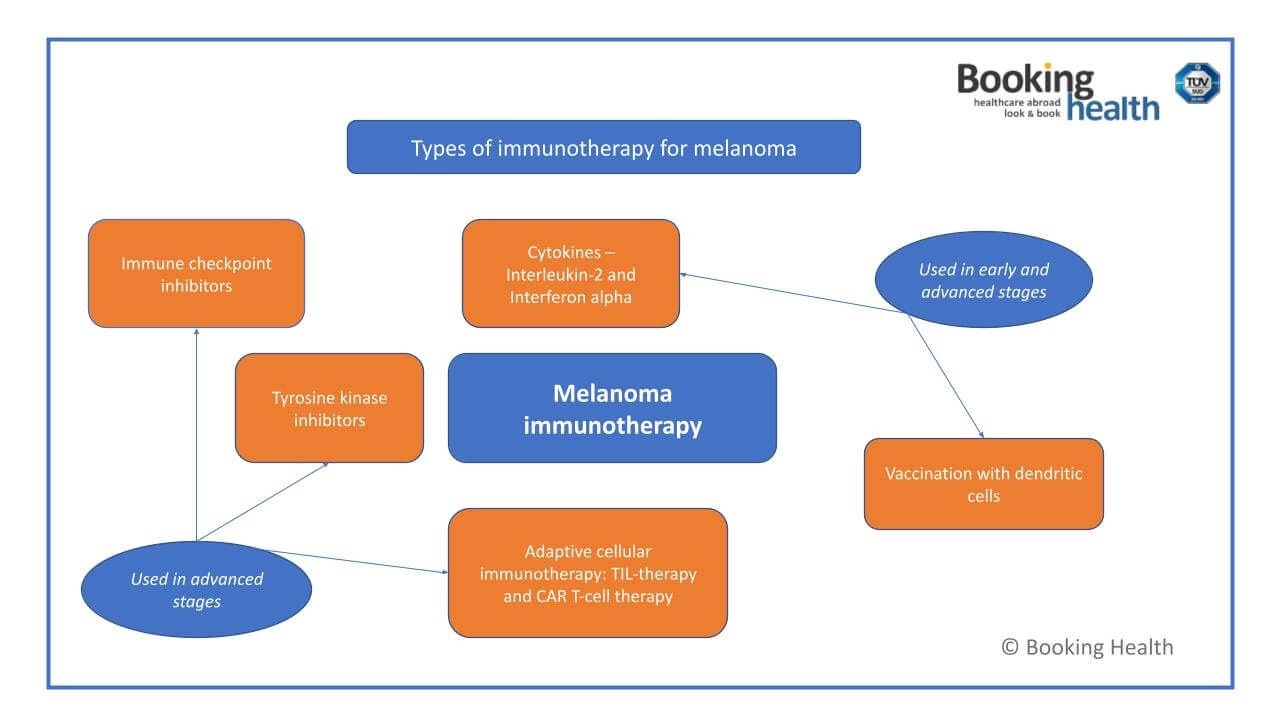
The overall goal of immunotherapy for melanoma is to make the human immune system learn to recognize and destroy cancer cells. In general, melanoma is a highly immunogenic tumor. This means that it has several unique surface antigens that can be a target for T-cells and other immune cells during the immune response. In medical practice, there are cases when small neoplasms disappear on their own, without surgery or other types of melanoma treatment, only due to the work of natural antitumor immunity. If this does not happen, then doctors use drugs of such groups:
- Dendritic cell vaccines, which harness the body's immune system to fight cancer and attack melanoma cells at any stage. These personalized vaccines are developed from the patient's own immune cells and can be effectively used both in early stages to prevent recurrence and in advanced melanoma to combat existing tumors.
- Cytokines, such as interleukin-2 and interferon alpha. In melanoma, interleukin-2 preparations are mainly used since interferon alpha is deactivated too quickly. By stimulating T-cells, cytokines help treat melanoma more effectively.
- Tyrosine kinase inhibitors. Such drugs are used in the detection of one of the mutations in the BRAF gene, namely the V600E mutation. Overall, mutations in the BRAF gene cause more than 80% of melanoma cases. Tyrosine kinase inhibitors suppress the activity of this gene and can support combination therapy approaches. BRIM-3 is the first phase III randomized trial that demonstrated an improvement in overall survival in patients with cutaneous malignant melanoma with BRAF V600E mutation [2].
- Monoclonal antibodies, such as immune checkpoint inhibitors. These are the most common drugs that are highly effective in patients with advanced melanoma. Immune checkpoint inhibitors block the CTLA-4 and PD-1 receptors on the surface of T-cells and thereby remove the ability of the melanoma cells and tumor cells to hide from anti-cancer immunity.
- Adaptive cellular immunotherapy: TIL-therapy and CAR T-cell therapy. In the first case, lymphocytes are isolated from the tissues affected by melanoma. Such T-cells have high anticancer activity. They are cultivated in the laboratory and reinfused in the patient to treat melanoma more aggressively. In the second case, doctors insert artificially synthesized receptors into the patient's lymphocytes, which will allow the immune system to see the tumor better. The method is extremely effective, but its application is limited by the high average cost of treatment.
Modern medicines of all groups are available in German clinics, and doctors have vast experience in their administration. It is better to choose the most effective immunotherapy treatments with minimal side effects, especially when treating advanced melanoma or designing combination immunotherapy regimens for advanced melanoma patients.
How Immunotherapy for Melanoma is Carried Out
The main type of melanoma treatment with immunotherapy is vaccination with dendritic cells. The treatment program consists of two main steps:
- During the first visit, melanoma patients undergo a comprehensive evaluation, including clinical examination and necessary laboratory tests. At this stage, blood samples are collected for manufacturing the individual vaccine. This initial step is completed in one day on an outpatient basis.
- The second step takes place after a 7-day period required for manufacturing the personalized DC vaccine. During this visit, the patient receives dendritic cell immunotherapy along with any necessary symptomatic treatment and specialist consultations. This vaccination is also administered on an outpatient basis and takes one day. A single injection is enough to boost anticancer immunity and stimulate T-cells to attack melanoma cells.
The choice of other immunotherapy treatments and schemes begins with an examination for mutations. In this case, the accuracy of the diagnostic stage significantly affects the treatment outcome since melanoma cells with different mutations are sensitive to different drugs. The most clinically significant mutations are:
- V600E mutation in the BRAF gene
- Mutation in the KIT gene
Depending on the results of the genetic examination, German oncologists recommend using a drug from the group of tyrosine kinase inhibitors, checkpoint inhibitors, or a combination therapy of both to treat melanoma effectively. Therapy can be continued for up to 2 years. It is canceled in case of the complete regression of the primary melanoma and all metastases according to the results of MRI, MSCT, or PET/CT with 18F-FDG. During immunotherapy, the patient undergoes regular examinations in order to assess the general condition, the immune response, and the progression of the disease.
| Treatment | Response Rate* | Duration of treatment | Cost of treatment,€** |
|---|---|---|---|
| Dendritic cell therapy | up to 90% | 1 week | 20,000 - 38,000 |
| Checkpoint inhibitors | up to 45% | about 1 year | 375,000 - 420,000 for the full course |
| CAR T-cell therapy | up to 40% | about 5 weeks | 450,000 - 550,000 |
*Booking Health data. Response rate is the number of patients who show improvement after treatment.
**The cost of treatment depends on the type of tumor, stage of cancer, and other factors.
Benefits of immunotherapy for melanoma
Melanoma is a highly immunogenic tumor. Therefore, treating advanced melanoma with immunotherapy is more effective than in most other types of cancer.
At a very early stage, the advantage of localized immunotherapy with creams is that it enables a complete cure of the cancer without surgery. This is especially important when the melanoma tumor is located in aesthetically and functionally significant areas. At later stages, the advantages of the technique are in the effective and non-invasive suppression of intradermal metastases.
The benefits of systemic immunotherapy for melanoma are as follows:
- A variety of available techniques, with dendritic cell vaccines leading the way due to their unique ability to activate the body's immune system at any stage of the disease. Other options include cytokines, TIL therapy, oncolytic viruses, immune checkpoint inhibitors, and CAR T-cell immunotherapy.
- High efficacy at all stages.
- Personalized approach, particularly with dendritic cell vaccines that are created individually for each patient using their own immune cells.
- Response to immunotherapy is observed in the majority of melanoma patients.
- The technique is more effective than targeted therapy and chemotherapy, helping patients treated with advanced tumors.
- Most immunotherapy drugs have low toxicity and are well-tolerated.
Recent studies show that innovative immunotherapy options allow patients with advanced melanoma to expect not only long-term survival with complete remission but also a complete cure. Cases have been described where, after all tumors have disappeared as a result of immunotherapy, melanoma cells have not returned for many years of follow-up.
Latest Research and Breakthroughs in Melanoma Immunotherapy
Leading immunotherapy expert Prof. Frank Gansauge brings over two decades of groundbreaking experience in dendritic cell therapy, a revolutionary approach that has transformed melanoma treatment outcomes. As one of the pioneers of dendritic cell immunotherapy treatments since 2001, Prof. Gansauge has demonstrated remarkable success rates with this innovative method. His research has been particularly significant in establishing treating advanced melanoma as a cornerstone of modern therapy, showing how it can extend life expectancy.
With documented cases of patients treated achieving full remission and remaining cancer-cell free for over 5 years, Prof. Gansauge's work represents a crucial advancement in melanoma treatment protocols. His contributions also emphasize the importance of activating the body's immune system to attack melanoma cells, highlighting the potential of dendritic cell therapy in combination with immunotherapy approaches of other types.
Leading Immunotherapy Expert Prof. Frank Gansauge: "Revolutionizing Cancer Treatment with Dendritic Cell Therapy"
Effective Treatment for Advanced Melanoma Cases
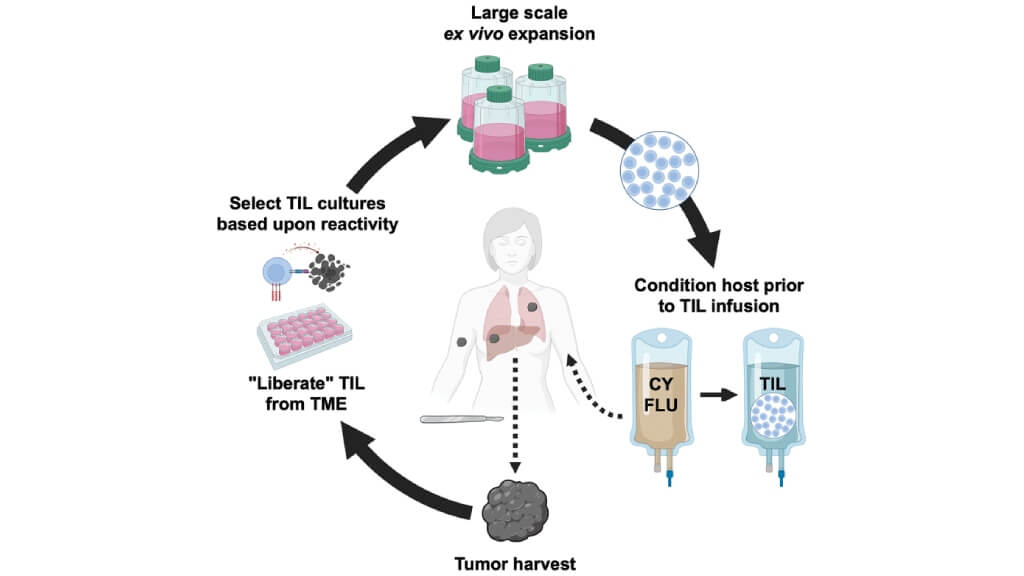
TIL therapy is based on the separation and cultivation of tumor cell-specific lymphocytes. These are white blood cells, T-cells, which are responsible for cellular immunity [3].
During the treatment, the patient’s own lymphocytes are obtained from the melanoma tumor tissue. They are located inside the melanoma, as they migrate to the tumor to fight cancer.
The next step is the activation of these T-cells and their cultivation in laboratory conditions. Then, the cells are injected back into the patient's body to enhance the immune response against the melanoma cells.
This method is combined with chemotherapy. The use of chemotherapy avoids the suppressive effect of immunity on the injected white blood cells. The drugs that do not suppress bone marrow are used.
Nowadays, TIL is used in the treatment of several types of cancer. The greatest success was achieved in the treatment of advanced melanoma. In some patients with metastatic melanoma, it is possible to achieve complete regression of the neoplasm and all metastases, even in metastatic melanoma treated with this method.
Is This a New Treatment Method?
TIL is not a new treatment method. Therefore, TIL refers to well-studied techniques in advanced melanoma therapy. Oncologists have studied not only the immediate, but also the long-term results of this immunotherapy treatment technique.
The first TIL trials on mice were carried out in 1986. In 1988, clinical trials on humans began. In 1992, the results from research illustrating the use of TIL in combination with immunotherapy with a high dose of interleukin-2 were published. About 34% of patients with advanced melanoma responded to the treatment, and 6% of these patients treated showed a complete response.
Since then, the technique has been improved, and today's results are much better than those that were reached 30 years ago, demonstrating the ability of the body's immune system to attack melanoma cells effectively.
Why Does it Work?
Our immune system can destroy cancer cells and does so all the time. It has long been known that people with acute immunity suppression (for example, HIV patients) suffer not only from infections, but also from malignant tumors.
Melanoma cells can defend themselves against immunity. Therefore, despite the migration of lymphocytes into the tumor, they cannot destroy it. There are several reasons for this:
- Insufficient number of T-cells
- Their low tumor cell reactivity
- Excretion of substances by melanoma cells, which reduces the activity of the immune cells
These problems are solved during the treatment, according to the TIL protocol. The immune cells are extracted from the melanoma tumor and cultivated in a laboratory in order to increase their number. At the same time, their reactivity increases. The T-cells develop without inhibiting tumor action, so when they are injected into the body, the doctors usually obtain a good immune response to treat melanoma. In the most favorable cases, the tumor cells and their metastatic foci are completely destroyed by the T-cells [5].
How is the Treatment Carried Out?
First, a doctor must obtain a melanoma tumor fragment with a diameter of at least 2 cm. An excision biopsy is used for this purpose. In fact, minor surgery is performed, during which the doctors receive the required amount of tissue.
The tumor is dissected into fragments of 1 to 3 cubic millimeters. They are cultivated for several weeks, and then interleukin-2 is added. Although many cancer cells are present in the material at the time of its harvesting, all of them gradually die "by their own death" or are destroyed by lymphocytes.
The cultivation period lasts 2-4 weeks. Then, TIL is tested for reactivity to tumor cells. Namely, the doctors verify whether these lymphocytes can destroy the melanoma cells in a particular patient. All of the tissues are cultivated in different tubes. The doctors check which populations of immune cells are more successful in fighting cancer. The specialists continue to multiply the most aggressive samples in order to obtain as many T-cells as possible. They cultivate them for another 2 weeks.
In total, the cultivation phase lasts 5-6 weeks. At the first stage, the doctors obtain 30-50 million T-cells. Then, during the final 2 weeks, their number is brought up to 1 billion. This is the minimum required for a successful melanoma treatment. Subsequently, these billion T-cells, or a little more, are injected into the patient's body.
Is it Always Possible to Obtain Cells for the Treatment of Melanoma?
The doctors do not always manage to obtain a generation of T-cells that are aggressive enough against the melanoma tumor. On average, they obtain them with a probability of 60 to 90%.
The researchers have demonstrated that the chance of success mostly depends on the age of the patients with advanced melanoma. In people under 30 years old, the chance of successfully receiving TIL is 94%, while for advanced melanoma patients older than 60 years old, it is only 46%. Cells can be obtained more often in women than in men. People who underwent the chemotherapy course more than 3 months ago have a better chance of receiving a good population of immune cells to treat melanoma.
The Results of Melanoma Treatment
Good melanoma treatment results can be achieved in 50% of patients with advanced melanoma. Their symptoms are less severe, most tumor cells regress, the growth rate of the melanoma tumor slows down, and the duration and quality of life increase. In 20% of advanced melanoma cases, the tumor and its metastases regress completely [6].
Although TIL therapy does not guarantee a cure, even the above-mentioned results should be considered impressive. After all, do not forget which patients treated can benefit from immunotherapy treatments. These are mainly people with an advanced stage of the disease, who no longer receive any results from other melanoma treatment methods. That is, doctors manage to achieve excellent results, even in the most severe cases.
It is worth mentioning the disadvantages of the TIL protocol, which at the moment do not allow doctors to make the technique a standard method for treating advanced melanoma at its advanced stages. It has two main disadvantages:
- High price
- Significant duration – up to 6 weeks
Not all melanoma patients can pay for TIL. This type of therapy is not available in all countries. It is carried out only in highly specialized cancer centers. Patients with the most aggressive types of advanced melanoma are not always able to wait 5-6 weeks until the population of immune cells is ready. Therefore, not every patient is a candidate for this treatment technique.
Enhanced protocols
Doctors constantly develop new, improved TIL protocols. They strive to make the treatment more effective, safer, and accessible, so that patients with metastatic melanoma can get it faster.
The main immunotherapy treatments for metastatic melanoma using TIL, which are already used in clinical practice or at the research phase, are the following:
- Low doses of interleukin-2 – some trials demonstrate that such treatment can reduce side effects with comparable results
- Young-TIL – treatment protocol, which has a shorter duration (allows patients with metastatic melanoma to undergo the treatment and treat melanoma more effectively)
- Immunosuppressive medications and total body irradiation increase the effectiveness of TIL
- Increasing doses of drugs, which suppress immunity, in some trials, a frequency of complete responses to immunotherapy treatments up to 40% was demonstrated (but such treatment regimens have more side effects)
- The possibility of using interleukin-15 and interleukin-21 instead of, or in addition to, the traditionally used interleukin-2 is studied
Is the Treatment Safe?
Most side effects are caused by chemotherapy, which is used during TIL. The main ones are:
- Gastrointestinal discomfort
- Fatigue
- Low blood cell count
Blood transfusions are required in many patients with metastatic melanoma. A decrease in the number of immune cells increases the risk of infections. If they occur, antibiotics are used. During the treatment of infectious pathologies, TIL T-cells can be stored frozen.
Immediately after the intravenous administration of TIL, most patients treated experience chills and a fever. Many patients treated have an increased heart rate and high blood pressure, as the body's immune system reacts to the therapy.
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods and with leading specialists in this field.
Success Stories in Immunotherapy Cancer Treatment
FAQ: Immunotherapy for melanoma in Germany
Send request for treatmentTIL protocol is based on the separation and cultivation of tumor cell-specific lymphocytes. During the treatment, the patient’s own lymphocytes are obtained from the melanoma tumor tissue. After processing these cells, they are injected back into the patient's body to fight cancer cells.
Germany is known for its structured protocols and disciplined approach. High-quality standards and highly specialized doctors are responsible for the safety and continuity of the process. That is why immunotherapy for melanoma in Germany shows excellent results.
Most side effects are caused by chemotherapy, which is used during TIL for melanoma. The main ones are gastrointestinal discomfort, fatigue, and low blood cell count.
The cost of immunotherapy for melanoma in Germany depends on the type of immunotherapy, duration of treatment, stage, and severity of the disease.
Immunotherapy for melanoma can’t completely cure the disease. However, this type of treatment allows for a high level of control of disease progression and prolongation of life expectancy.
Booking Health support for immunotherapy for melanoma provides international patients with expert coordination for diagnostics, clinic selection, and timely access to advanced treatments. They ensure patients receive effective care, including innovative therapies.
The highest response rate is with dendritic cell vaccination – it is up to 90%. Checkpoint inhibitors are effective in up to 45% of cases, CAR T-cell therapy – at up to 40%. This makes dendritic cell vaccines valuable for melanoma patients.
Treatment duration varies. Checkpoint inhibitors are intended for continuous intake; CAR T-cell therapy takes about 5 weeks, and dendritic cell therapy can be completed in just 1 week – as a painless outpatient intervention.
Cost ranges from €20,000-€38,000 for dendritic cell therapy to over €450,000 for CAR T-cell therapy (the price is explained by genetic modifications of a patient immune cells). Dendritic cell therapy offers the most cost-effective solution.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Kalyan Saginala, Adam Barsouk, John Sukumar Aluru, Prashanth Rawla, Alexander Barsouk. Epidemiology of Melanoma. Med Sci (Basel). 2021 Oct 20;9(4):63. doi: 10.3390/medsci9040063. [DOI] [PMC free article]
[2] Andrei POPESCU, Rodica Maricela ANGHEL. Tyrosine-kinase Inhibitors Treatment in Advanced Malignant Melanoma. Maedica (Bucur). 2017 Dec;12(4):293-296. [PubMed]
[3] Allison Betof Warner, Pippa G Corrie, Omid Hamid. Tumor-Infiltrating Lymphocyte Therapy in Melanoma: Facts to the Future. Clin Cancer Res. 2022 Dec 9;29(10):1835–1854. doi: 10.1158/1078-0432.CCR-22-1922. [DOI] [PMC free article]
[4] Shravan Leonard-Murali, Udai S Kammula. Optimizing TIL therapy for uveal melanoma: lessons learned and unlearned from cutaneous melanoma. Immunotherapy. 2025 Mar 18;17(4):283–291. doi: 10.1080/1750743X.2025.2478808. [DOI] [PMC free article]
[5] Katy K Tsai, Krishna V Komanduri. Tumor-Infiltrating Lymphocyte Therapy for the Treatment of Metastatic Melanoma. Am J Clin Dermatol. 2025 Jun 23;26(5):733–745. doi: 10.1007/s40257-025-00957-5. [DOI] [PMC free article]
[6] S Martín-Lluesma, I M Svane, U Dafni et al. Efficacy of TIL therapy in advanced cutaneous melanoma in the current immuno-oncology era: updated systematic review and meta-analysis. Ann Oncol. 2024 Oct;35(10):860-872. doi: 10.1016/j.annonc.2024.07.723. Epub 2024 Jul 23. [DOI] [PMC free article]
Read:
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
Dendritic cell therapy in cancer treatment in Germany - Vaccination against cancer
Top 10 Leading Oncology Hospitals for Cancer Treatment in Germany
Article menu:
- Role of Immunotherapy in the Complex Treatment of Melanoma
- Types of Immunotherapy for Melanoma
- How Immunotherapy for Melanoma is Carried Out
- Benefits of immunotherapy for melanoma
- Latest Research and Breakthroughs in Melanoma Immunotherapy
- Effective Treatment for Advanced Melanoma Cases
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ: Immunotherapy for melanoma in Germany
Don't know where to start?
Contact Booking Health














