Dr. med. Michael Lipp is one of the most experienced colorectal surgeons in Germany, specializing in HIPEC treatment. During the doctor's 18 years of active clinical practice, he has learned much about the healthcare systems of several countries (Switzerland and Germany) and has published more than 60 scientific papers on various topics. His research interests include the development of new techniques in abdominal surgery and the study of potential biomarkers for colorectal cancer.
Dr. Lipp now practices at the Asklepios Hospital Barmbek Hamburg, Germany, in the Department of General and Abdominal Surgery, Hepatopancreatobiliary Surgery and Hernia Surgery. He is the department's leading specialist in HIPEC and colorectal surgery. In this exclusive interview, Prof. Lipp shares his in-depth knowledge of the HIPEC technique, covering important aspects such as indications, features, efficacy, and perspectives.
ABOUT DR. LIPP
My name is Michael Lipp. I work in the Department of General and Abdominal Surgery, Hepatopancreatobiliary Surgery and Hernia Surgery at the Asklepios Hospital Barmbek Hamburg. We have been performing cytoreductive surgery and HIPEC in patients with peritoneal carcinomatosis for many years. I have been working at the Asklepios Hospital Barmbek Hamburg since 2011 and have been performing HIPEC since 2015.
WHAT IS HIPEC AND HOW IS IT DIFFERENT FROM OTHER SURGICAL PROCEDURES?
The concept of treating peritoneal carcinomatosis with HIPEC was developed at the end of the last century.
HIPEC is a procedure in which the abdominal cavity is rinsed with a solution containing a high concentration of chemotherapy drugs after cytoreductive surgery. Abdominal tumors can metastasize throughout the peritoneum, that is, the primary cancer site grows and invades surrounding tissues (per continuitatem). Surgical resection of metastases in the abdominal cavity and rinsing it with a solution of chemotherapy agents immediately after surgery allows for the destruction of micrometastases, i.e. small clusters of cancer cells that cannot be seen with the naked eye during surgery.
Therefore, the concept of treating peritoneal carcinomatosis with HIPEC always involves HIPEC in combination with surgery. Surgery is the first stage of treatment to remove visible tumor foci, and HIPEC is the "icing on the cake" to ensure maximum success of the operation.
WHAT TYPES OF CANCER CAN BE TREATED WITH HIPEC?
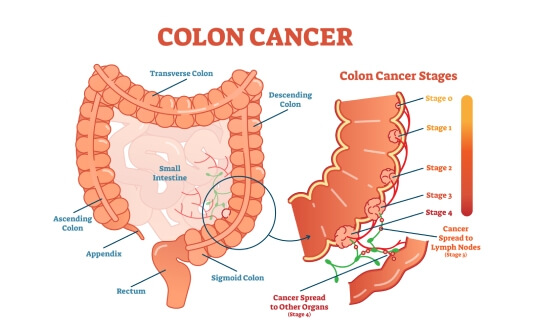
We do not currently use HIPEC to treat all cancers with peritoneal metastases. There is a reason for this: the prognosis for each of these cancers is different. Up to 90% of the patients we treat with HIPEC are diagnosed with colorectal cancer.
We offer HIPEC to some patients with stomach cancer. We also have rare tumors in our practice, such as mesothelioma. There is pleural mesothelioma, which is caused by exposure to asbestos fibers. This tumor, however, can also affect the peritoneum. The treatment of peritoneal mesothelioma is one of our specialties. We also treat pseudomyxoma peritonei. Patients with these tumors have a good prognosis a priori, and cytoreductive surgery combined with HIPEC can improve it even further.
Based on our observations, the HIPEC procedure is also a very promising method for treating women with abdominal metastases from ovarian cancer. Currently, abdominal surgeons, and I in particular, mainly face the treatment of cancer recurrence after surgery. It is likely that the tumor foci on the peritoneum were removed during the primary surgery, but cancer recurrence is an indication for repeated surgery in combination with HIPEC.
WHO IS AN IDEAL CANDIDATE FOR HIPEC?
The success of the treatment largely depends on the correct determination of the indications for HIPEC. Therefore, we have to strictly follow the candidate selection criteria. First of all, HIPEC treatment is suitable for patients whose condition allows them to undergo a complex operation lasting several hours. At the same time, the patient's psycho-emotional state plays an important role because he or she needs to be ready to deal with all the difficulties associated with the treatment, including the peculiarities of the course of oncopathology and the possible risks of developing complications after surgery. It is important that the patient can confidently say, "Yes, I want this very treatment." Even if some difficulties arise during the therapeutic process, the patient must be committed to going all the way. This point is of crucial importance.
Next, there are the medical aspects to consider. As I have already said, there must be an absolute indication for treating a particular tumor with HIPEC, as it is not suitable for all types of cancer. The success of the treatment depends largely on the peritoneal cancer index.
The basic problem is that peritoneal carcinomatosis is the common name for cancers of all types and extent of spread. Whether it is just 2 tumor foci in the abdominal cavity or as many as 500, this is peritoneal carcinomatosis and there are no distinctions. Nevertheless, this point is of utmost importance for the upcoming surgery.
To summarize, HIPEC is suitable for patients with a satisfactory general health condition and an appropriate psychological attitude. The next prerequisite is the selection of patients with tumors for which HIPEC is advisable and a minimal peritoneal cancer index.
HOW IS HIPEC PERFORMED? WHAT STAGES DOES IT CONSIST OF?
The first stage of HIPEC is surgery, multivisceral resection. This is not a minimally invasive or robot-assisted surgery but an open abdominal surgery. The operation involves a long incision in the anterior abdominal wall because the surgeon must be able to perform a complete visual inspection and make the necessary manipulations if cancer foci are detected in any part of the abdominal cavity.
The first step in surgery is to remove all visible tumors. This can sometimes be difficult because even modern imaging methods such as CT or MRI have a certain resolution limit and do not always guarantee that all tumor foci will be identified before surgery. The surgeon can only see all the tumors to be removed during surgery.
Such surgical procedures can be quite extensive. They may include additional stages. For example, if appendicitis is found, an appendectomy will be performed simultaneously with cytoreductive surgery. We usually perform gallbladder removal surgery during multivisceral resections. Undoubtedly, it would be unwise to put the patient at risk of repeat surgery, for example, for cholelithiasis.
Our goal is to defeat cancer, but we are well aware that a treatment like HIPEC does not go unnoticed. We don't want the patient to have to prepare for another surgery, for example, for cholelithiasis, 5 years after HIPEC. So, as I said, we do a standard surgery first, like an appendectomy or a cholecystectomy, and then we resect the cancer foci.
When performing surgery, we often have to excise the rectum. This is due to the fact that the rectum is the distal part of the colon and is located in the lower pelvis, where tumor foci often accumulate due to gravity.
After the surgical removal of all visible tumors from the abdomen, silicone drains are placed in the abdomen to perform HIPEC. The surgeon sutures the anterior abdominal wall and then connects the drains to a perfusion device. This is a special pump that heats a solution of chemotherapy drugs. The abdominal cavity is rinsed with a heated solution of chemotherapy agents for 90 minutes, i.e., HIPEC, hyperthermic intraperitoneal chemotherapy, is performed. HIPEC is the final stage of the operation.
WHAT SPECIALIZED TRAINING AND EXPERIENCE SHOULD A SURGEON HAVE TO PERFORM HIPEC?
Generally, abdominal surgeons perform HIPEC.
General surgeons do not perform this type of surgery. It is the responsibility of highly specialized surgeons. Today, there are many subspecialty training programs available to physicians to learn surgical techniques for treating peritoneal carcinomatosis. Physicians with specialized training in colorectal surgery mostly perform HIPEC because cytoreduction almost always involves bowel resection. HIPEC is, therefore, the specialty of colorectal and abdominal surgeons.
HOW DO THE PATIENT AND MEDICAL TEAM PREPARE FOR HIPEC?
The complexity of this operation for the surgeon lies in performing a wide range of manipulations in a relatively limited time. The specialist must perform all stages of surgical resection efficiently and quickly. There is no opportunity to linger on a single pathological focus because the longer the operation lasts, the higher the risks for the patient. The surgeon is faced with the task of performing all manipulations without any delay.
As for the preparation on the part of the patient, it is absolutely necessary to empty the bowels the day before the operation, just as before the colonoscopy. Of course, it is desirable for the patient to be in the best possible physical condition immediately before the operation and to have no deficiencies. If there is time left before the operation, it is necessary to take care of a balanced diet and physical activity to prepare the body for the upcoming treatment. This is really important, including physical training, if the patient's condition allows it. Based on our observations, such preparation for surgery is beneficial for the patient.
If the patient is taking the chemotherapy drug Cisplatin, which is known to adversely affect kidney function, an additional intravenous infusion of medications for kidney support is given prior to cytoreductive surgery with HIPEC.
These are the most important points to consider when preparing for HIPEC.
WHAT ARE THE POTENTIAL RISKS OF HIPEC? WHAT COMPLICATIONS MAY THIS TREATMENT CAUSE?
As I have already mentioned, the main problem is that before the operation, we do not know exactly what surgical manipulations may be required.
For example, if cancer foci are found in the spleen, the organ is removed, which increases the risk of bleeding. Large blood vessels run through the spleen, so the surgeon must ligate them. Of course, this may provoke certain risks.
It may also be necessary to remove liver metastases that grow from the outer surface of the organ into its parenchyma during surgery. In this case, there is a risk of bile entering the abdominal cavity after surgery. Bile is a product of liver secretion. Bile spreading beyond the liver parenchyma causes the development of a biloma.
Another example is when the surgeon has to perform a bowel resection during cytoreductive surgery. Of course, in such situations, we restore the integrity of the intestines by means of an anastomosis. However, there is a risk of intestinal anastomosis failure.
Extensive bowel resection requires the formation of a new rectal outlet (colostomy). Here, at the Asklepios Hospital Barmbek Hamburg, we have a clear idea of what we are doing. We operate on cancer patients who have no time for postoperative complications. Therefore, if we find that an anastomosis is not advisable or the patient's condition worsens during surgery, we prefer a colostomy in rare cases.
Of course, it should be taken into account that a colostomy affects the patient's quality of life, but we believe that it is justified in the presence of life-threatening cancer. In addition, it should be understood that cytoreductive surgery with HIPEC is rarely the final stage of the therapeutic process because many patients receive classical chemotherapy after surgery.
These are the major complications of HIPEC. Of course, there are other complications that may potentially occur after major surgery, such as pneumonia or pulmonary embolism.
HOW LONG DOES A HIPEC PROCEDURE TAKE ON AVERAGE?
Under certain circumstances, the operation may take a very long time. The more cancer foci there are in the abdomen, the longer it will take.
In the early stages of peritoneal carcinomatosis, cytoreductive surgery may take only 2-3 hours. Then HIPEC begins, the second stage of surgery. It takes 90 minutes.
However, experience shows that, together with drain placement, perfusion device setup, and heating of the chemotherapy drug solution to the required temperature, HIPEC takes 2.5 hours. Thus, even if there is a minimal number of tumor foci in the abdominal cavity, the duration of the operation is 5-6 hours. It all depends on the number of cancer foci. We had to operate on patients for 10, 11, and 12 hours. Sometimes this happens. Other HIPEC surgeons will confirm this.
Due to the fact that the duration of the surgery can be 5-10 hours, it is very important that the patient is able to tolerate such a major surgical procedure.
HOW OFTEN DOES DR. LIPP PERFORM HIPEC?
I am currently performing HIPEC once a week. This is due to the fact that the entire medical team is present in the operating room during the surgery. We also have patients who need other operations, so we are physically unable to perform HIPEC every day. Of course, there are weeks when we do 2 HIPEC procedures.
HOW LONG DOES IT TAKE FOR A PATIENT TO RECOVER FROM HIPEC?
From my experience, the shortest hospital stay after HIPEC was 9 days. It was a very fast period of postoperative recovery. As a rule, the duration of a hospital stay after such a treatment is 10-14 days. If there are complications, there is no clear time limit for hospitalization, so the patient stays in the hospital as long as necessary.
WHAT FOLLOW-UP CARE DO PATIENTS NEED AFTER HIPEC?
As I have already mentioned, our hospital performs most HIPEC procedures for colorectal cancer. In Germany, there is a clear five-year follow-up care protocol for patients with colorectal cancer.
After the completion of treatment at the hospital, the patient visits his or her oncologist for regular follow-up examinations. If necessary, chemotherapy may be prescribed. Basically, medical supervision after HIPEC includes blood tests, monitoring tumor marker levels to prevent cancer progression, and imaging tests, the main of which is a CT scan.
As I said before, the problem is that it is almost impossible to see small foci of tumor growth on CT scans because they only become visible when they reach a certain size. This is the generally accepted algorithm for follow-up care of patients after HIPEC.
There are special clinical cases where a personalized follow-up regimen is developed for the patient. For example, CT scans are performed every 3 or 6 months in order to assess the condition of the abdominal organs as accurately as possible. The question of performing a diagnostic laparoscopy may also arise.
WHAT CAN AFFECT THE SUCCESS OF HIPEC?
The patient's role in the outcome of HIPEC is minimal.
The surgeon is fully responsible for the success of the procedure. Every step of the surgery is important, including the quality of surgical manipulations, drainage placement, and monitoring the work of the perfusion device. As I already said, it is important to monitor kidney function and eliminate the risk of dehydration prior to surgery. Communication with the anesthesiologists plays an important role as well. They should be as united as possible with the team of surgeons who will perform HIPEC. This will allow the anesthesiologists to take into account all the nuances associated with complications, including the risks of kidney damage.
It is up to the surgeons to make sure that HIPEC is as successful as possible, so absolutely nothing depends on the patient here.
WHAT IS THE PROCESS OF SELECTING PATIENTS FOR WHOM HIPEC IS THE OPTIMAL TREATMENT OPTION?
We pay special attention to the detailed study of each case in order to understand whether HIPEC treatment is suitable for the patient.
For example, if a person cannot climb a flight of stairs, he or she will not tolerate such a complex surgery. There is no point in doing it. It is very important for us that the patient and his or her family initially understand the treatment they are going to receive and the risks associated with it.
As I mentioned at the beginning of our conversation, the patient's diagnosis must correspond to the indications for HIPEC. We review his or her clinical case at an interdisciplinary tumor board with the participation of radiologists, oncologists, gastroenterologists, and gynecologists. This is now a common practice in oncology. I don't personally decide whether to operate on a patient or not, but it is a joint decision of a medical board.
When working with a candidate for HIPEC, we need recent CT or MRI scans of the chest and abdomen, which should be done no more than 4 weeks prior to the patient's visit to the hospital. It is advisable for the patient to provide us with all necessary medical documents, such as information about the previous cancer surgery, medical reports, previous medications, allergies, etc. Taking this information into account, we can comprehensively assess the patient's condition. If HIPEC is advisable for the patient, we will tell him or her about the specific surgical procedures to be performed during the operation.
As I said, there are certain difficulties at this stage. We cannot provide the patient with accurate information about the extent of the upcoming surgery because we may find new cancer foci after opening the abdominal cavity that CT and MRI scans have not shown. Of course, many people are frankly confused at this point. If necessary, we may perform a diagnostic laparoscopy, based on the results of which we can more accurately predict the potential outcome of the surgery.
WHAT ADVANCES HAVE BEEN MADE IN THE USE OF HIPEC IN RECENT YEARS? HOW HAVE THEY AFFECTED TREATMENT OUTCOMES?
When HIPEC was first introduced into clinical practice, it was used for patients in the palliative stage of their disease. By the time HIPEC was prescribed, the patient had already undergone all possible treatments. Most of these patients were in poor general health and were often diagnosed with a large number of tumor foci in the abdominal cavity.
In the process of using HIPEC, it has become evident that, with the proper selection of patients, it is possible to significantly improve the prognosis and quality of life in many cases. There are cases where patients can be completely cured. This is what cytoreductive surgery with HIPEC is all about. In fact, it is the only curative procedure for peritoneal carcinomatosis, while all other techniques are palliative.
Obviously, the fewer cancer foci in the abdominal cavity, the better the results of HIPEC. Today, HIPEC is actively combined with other therapeutic procedures, in particular systemic chemotherapy. For example, systemic chemotherapy used to be administered after surgery to remove a colorectal tumor, if lymph nodes were found to be affected. Today, every patient receives adjuvant systemic chemotherapy after HIPEC, and it is part of the standard clinical protocol.
We also know that in the advanced stages of colorectal cancer (a malignant tumor that extends beyond the colon), it is highly likely that some tumor cells will detach and spread throughout the abdominal cavity. At some point, this may lead to peritoneal carcinomatosis, in which there is a high risk of stomach involvement in the malignant process.
Healthcare professionals are now working to make HIPEC an adjuvant treatment option in the future. We would not have to wait for the tumor to grow again, and the patient would be referred for another surgery. After intestinal surgery, we would determine that it was an advanced tumor and that it would require not only systemic therapy but also HIPEC to treat it.
We also learned some new facts about HIPEC. For example, physicians in North America and Europe used different chemotherapy drugs for it. This allowed us to conclude that Oxaliplatin, which was widely used in Europe to treat peritoneal carcinomatosis, is not very effective for colorectal cancer. The duration of HIPEC has also changed. For example, a few years ago, HIPEC for colorectal cancer was only 30 minutes, and at some point it was necessary to admit that the treatment had failed.
The duration of HIPEC is now 90 minutes. A different cytostatic drug, Mitomycin C, is used. So there are a lot of changes in the use of HIPEC, and this is not the end yet. We are working hard to improve the process.
In my opinion, it is advisable to perform HIPEC as early as possible in a patient with indications for this procedure, as this treatment method is effective and can be really helpful. Timely performance of the procedure will facilitate the treatment process for both the patient and the surgeons, because in this case the recovery is much faster and the oncopathology can be better controlled.
ARE THERE ANY ALTERNATIVES TO HIPEC? IN WHAT CASES CAN ALTERNATIVE METHODS BE PREFERRED?
There are currently three main methods of cancer treatment in conventional medicine: surgery, systemic chemotherapy (intravenous administration of chemotherapy drugs), and radiation therapy.
Both surgery and radiation therapy are local methods of affecting the tumor. It is not possible to completely irradiate the abdomen, so it doesn't work that way. If surgery is contraindicated, chemotherapy is ultimately the only alternative treatment option. When conducting chemotherapy, the question of its effectiveness always arises. Chemotherapy for peritoneal carcinomatosis is definitely effective, but the question is how effective?
Now there is another therapeutic procedure that is gaining popularity. This is called pressurized intraperitoneal aerosol chemotherapy (PIPAC). PIPAC is a minimally invasive procedure. Catheters and laparoscopic trocars are inserted into the abdominal cavity through the abdominal wall, after which the chemotherapy drug (the same as in HIPEC) is sprayed under pressure into the abdominal cavity in the form of an aerosol. The main difference is that PIPAC does not involve surgical tumor removal.
I am sure that the future has many discoveries in store for us.
Read:
PIPAC treatment for peritoneal cancer
Don't know where to start?
Contact Booking Health