The program includes:
- Initial presentation in the clinic
- clinical history taking
- review of medical records
- physical examination
- laboratory tests:
- complete blood count
- general urine analysis
- biochemical analysis of blood
- TSH-basal, fT3, fT4
- tumor markers
- inflammation indicators (CRP, ESR)
- indicators of blood coagulation
- abdominal ultrasound scan
- CT scan/MRI or PET-CT of abdomen
- preoperative care
- cytoreductive surgery to remove visible tumors
inside the abdomen and HIPEC - histological and immunohistochemical
examination of removed tissues - symptomatic treatment
- cost of essential medicines
- nursing services
- stay in the hospital with a full board
- accommodation in a 2-bed room
- elaboration of further recommendations
How program is carried out
During the first visit, the physician will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examination, such as the assessment of liver and kidney function, ultrasound scan and tomography of the abdominal organs. Based on the results of the examination, the physician will choose the surgical technique and the type of anesthesia. After that, preparation according to the preoperative standard will start.
Cytoreductive surgery begins with general anesthesia. The intervention is performed as open surgery, i.e. through the incision in the anterior abdominal wall, so that the surgeon can carefully examine the peritoneum and the surface of the abdominal organs. The surgeon removes affected by the malignant process areas of the peritoneum and metastases in other internal organs. This stage of the operation can take several hours, since the overall effectiveness of the treatment depends on the completeness of the malignant tissues removal.
At the next stage of the operation, the surgeon inserts several catheters into the abdominal cavity. Through the catheters, a heated solution of a chemotherapy drug is pumped inside. The special system maintains the required temperature (42-43 degrees Celsius), pressure and circulation rate of the medicinal solution. The solution mechanically flushes out blood clots and remnants of malignant tissues, and a heated chemotherapy drug destroys micrometastases in internal organs and lymph nodes (micrometastases can’t be detected by the naked eye).
After 1-1.5 hours, the chemotherapy drug is removed from the abdominal cavity and the abdominal cavity is washed with saline. After that, the surgeon removes the catheters and sutures the incision of the anterior abdominal wall.
After the completion of the operation, you will be transferred to the ward of the intensive care unit, under the round-the-clock supervision of doctors and nurses. In 1-3 days after the operation, your drains will be removed and you will be transferred to a regular ward for further recovery. The whole treatment takes 10-12 days on average.
Finally, the attending physician will evaluate the results of control examinations, schedule the date of discharge from the hospital and give you detailed recommendations for further follow-up and treatment.
Required documents
- Medical records
- MRI/CT scan of the abdomen (if available)
- Biopsy results (if available)
Service
You may also book:
 BookingHealth Price from:
BookingHealth Price from:
About the department
According to the Focus magazine, the Department of General, Abdominal, Adult and Pediatric Transplant Surgery ranks among the top German departments specializing in the treatment of bowel cancer!
The department specializes in the treatment of tumors of the gastrointestinal tract, pancreas, liver, and retroperitoneal space (peritoneal carcinomatosis), liver, kidney, pancreas, bowel transplantations in children and adults, as well as the surgical treatment of obesity and general surgical interventions. The Chief Physician of the department is Prof. Dr. med. Alfred Königsrainer.
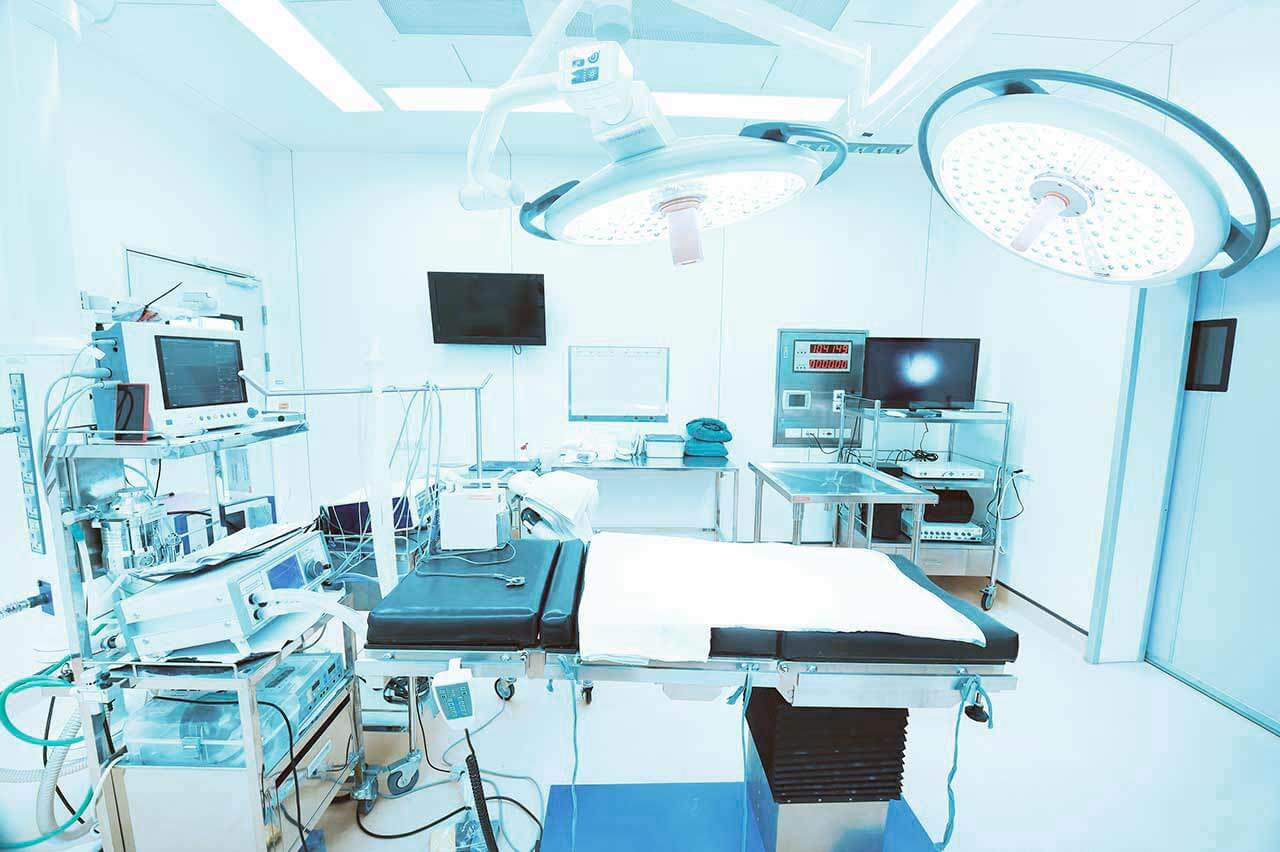
All surgical interventions are carried out in ultramodern operating rooms, equipped with the accurate equipment, computer systems, which allow to control the course of intervention. With appropriate clinical indications, the preference is given to minimally invasive interventions, which reduce blood loss, minimize the risk of the development of postoperative infections, as well as allow the patient to return to everyday life as soon as possible. Also, robotic surgery (daVinci surgical system) is widely used in the department.
The therapeutic service range of the department includes:
- General surgical interventions
- Surgical hernia treatment
- Functional surgery of the upper gastrointestinal tract (for example, treatment of gastroesophageal reflux disease)
- Gallbladder removal
- Appendix removal
- Sigmoid colon removal (in diverticulosis and diverticulitis)
- Surgical interventions in intestinal obstruction
- Sigmoid colon removal (in diverticulosis and diverticulitis)
- Emergency surgery (for example, in injuries of the abdominal organs)
- Bowel and pelvic surgery
- Constipation
- Pelvic organ prolapse (for example, rectocele, intestinal invagination)
- Fecal incontinence
- Anal fistulas and their recurrence
- Hemorrhoids
- Anal fissures
- Pilonidal sinus, coccygeal fistula, coccygeal cyst
- Benign and malignant tumors and polyps
- Chronic inflammatory bowel disease (ulcerative colitis, Crohn's disease)
- Liver and pancreatic surgery
- Removal of malignant liver tumors
- Extensive and combined resections
- Removal of liver segment
- Removal of malignant and benign neoplasms of the biliary tract
- Surgical treatment of chronic and acute pancreatic inflammatory processes
- Transplant surgery in adults and children
- Kidney transplantation
- Liver transplantation
- Pancreas transplantation
- Bowel transplantation
- Multivisceral transplantation
- Oncosurgery
- Removal of tumors of the upper gastrointestinal tract (esophagus, stomach), liver, bile ducts
- Removal of retroperitoneal tumors
- Removal of small and large bowel tumors
- Removal of thyroid and adrenal tumors
- Removal of soft tissue tumors
- Bariatric surgery (surgical treatment of obesity)
- Endoscopic sleeve gastroplasty
- Sleeve gastroplasty (classical method)
- Omega Loop Bypass technique
- SADI-S surgical technique
- Gastric bypass surgery
- Biliopancreatic diversion
- Gastric banding
- Intragastric balloon installation
- Tummy tuck after quick weight loss
- Endocrine surgery
- Thyroid and parathyroid surgery
- Adrenal surgery
- Surgical treatment of neuroendocrine tumors
- Other medical services
Curriculum vitae
Professional Experience
- 01.12.1979 - 30.11.1980 Intern, Meran Regional Hospital, South Tyrol (Gynecology, General Surgery, Internal Medicine).
- 01.01.1981 - 30.06.1987 Training for the title of a Medical Specialist, Department of General, Vascular, Pediatric, Transplant Surgery, Surgical Endoscopy, University Hospital Innsbruck (Head: Prof. Dr. F. Gschnitzer).
- June 1987 Medical Specialist in Surgery.
- 01.10.1987 Senior Physician, Department of General, Vascular, Pediatric, Transplant Surgery, Surgical Endoscopy, University Hospital Innsbruck (Head: Prof. Dr. F. Gschnitzer).
- 09.12.1991 12/09/1991 Habilitation, General Surgery, Department of General, Vascular, Pediatric, Transplant Surgery, Surgical Endoscopy, University Hospital Innsbruck. Subject: "Experimental and clinical trials on immunological monitoring of pancreatic allografts".
- 31.03.04 Deputy Head of the Department of General and Transplant Surgery (Chief Physician: Prof. Dr. R. Margreiter), University Hospital Innsbruck.
- Head of the Department of General, Abdominal, Adult and Pediatric Transplant Surgery at the University Hospital Tuebingen.
University Positions
- 09.12.1991 University Lecturer.
- May 1992 Assistant Professor.
- 01.10.1997 University Professor.
Internships Abroad
- April 1994 Istituto Scientifico "San Raffaele", Milan, Italy, Clinical and Experimental Islet Cell Transplantation (Director: Prof. G. Pozza).
- 01.07. - 31.12.1995 Bolzano, South Tyrol, Bolzano Regional Hospital, Head of the Department of General Surgery.
- January and February 1996 University Hospital Eppendorf, Department of General Surgery (Head: Prof. Dr. CE Brölsch), Hepatobiliary Surgery and Liver Transplantation.
- March 1996 Saint-Luc University Hospital, Brussels, Department of Pediatric Surgery and Transplantology (Head: Prof. Dr. JB Otte), Hepatobiliary Surgery and Liver Transplantation.
- April - June 1996 Hospital at the University College London (UK), Section of Liver Transplantation (Head: Prof. Dr. R. Williams Cons).
Special Positions
- Until 2004 Member of the Eurotransplant Pancreas Advisory Committee.
- Board Member of the European Liver Transplant Association (ELTA).
- Until 2004 Board Member of the Austrian Society for Transplantation.
- Member of the Advisory Council on Transplantation of the Austrian Federal institute for Health Care.
- Until 2004 Representative of the Tyrol Working Group on Oncology (cancer of the esophagus and cardiac stomach; tumors of the liver and biliary tract).
- Until 2005 Board Member of the AIDPIT.
Photo of the doctor: (c) Universitätsklinikum Tübingen
About hospital
According to the prestigious medical publication Focus, the University Hospital Tuebingen ranks among the top five German hospitals!
The hospital was founded in 1805, therefore it is proud of its long history, unique experience, and outstanding achievements in the field of medical care, as well as research and teaching activities. Nowadays, it is one of the most advanced medical institutions, which provides a wide range of general and highly specialized medical services. The hospital combines the state-of-art medical technologies in the field of diagnostics and the very latest treatment methods of a wide range of diseases.
The hospital has 17 specialized departments, which cover almost all fields of modern medicine and contribute to the top-class medical service in Germany. It treats about 367,000 outpatients and 74,000 inpatients annually. This testifies to the high authority of the hospital at the national and international medical arena. This is the first German hospital, which confirmed the high quality of healthcare and the effectiveness of service with a KTQ certification (in 2009).
Photo: (с) depositphotos
Accommodation in hospital
Patients rooms
The patients of the University Hospital Tuebingen live in comfortable single and double rooms with an ensuite bathroom equipped with a shower and toilet. The beds in the patient rooms are equipped with orthopedic mattresses that promote good and full sleep. There is a TV in the room, and it is also possible to connect a smartphone or laptop to the Internet. In addition, there is enough space in the patient room to receive 2-3 guests without inconvenience for the second patient.
The enhanced-comfort rooms include a hairdryer, heated towel rail, a large mirror, a direct dial telephone, a flat-screen satellite TV, a writing desk, free Internet access, a mini-bar and a refrigerator.
Meals and Menus
The patients of the hospital are offered tasty and healthy three meals a day: breakfast, lunch and dinner. Breakfast is served as a buffet, while for lunch and dinner there is a choice of several menus. Also, if desired, the patient will be provided with an individual menu. There are several cafes and cafeterias on the territory of the hospital, where one can have a tasty meal or enjoy a cup of coffee, tea and dessert.
Further details
Standard rooms include:
Religion
Religious services are available upon request.
Accompanying person
During the inpatient program, an accompanying person can stay with you in a patient room or in a hotel of your choice.
Hotel
During the outpatient program, you can stay in a hotel of your choice. Our managers will help you choose the most suitable option for you.