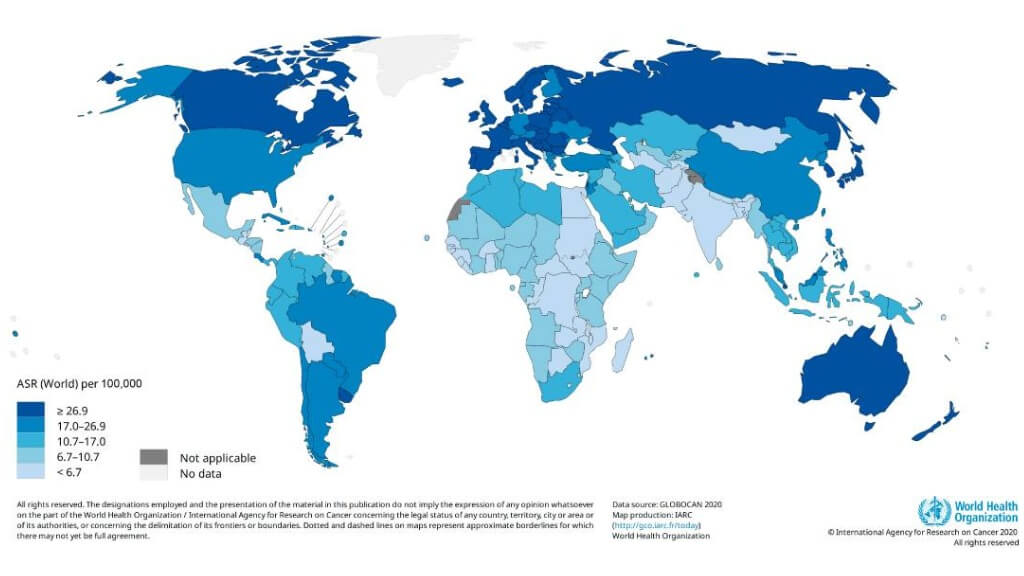
Colorectal cancer (CRC) is a major public health concern in Germany and is among the most frequently diagnosed cancers. In 2022, approximately 24,650 women and 29,960 men were newly diagnosed with CRC. Most cases arise in the colon, with relatively few in the rectum, and incidence rates increase sharply after the age of 55 years [1]. Despite significant advances in diagnostics and standard therapies, CRC remains a leading cause of cancer-related mortality.
The 5-year survival rates of colorectal cancer patients vary greatly depending on the stage of the disease一approximately 90% for early growth and only 12% for advanced colorectal cancer. These statistical data underline the need for more effective and more individualized cancer therapies, particularly in advanced cancer patients.
Germany has become a world leader in oncology, especially in the field of immunotherapy for colorectal cancer. German clinics successfully combine immunotherapy, targeted therapy, and other measures in a modern way to increase the immune response against the tumor cells. So much more interesting and more important, however, is the fact that good percentage remission rates of over 90% for early colon and rectal cancer and about 80% for advanced colorectal cancer have been achieved with dendritic cell vaccines in a multimodal treatment. These results suggest the great potential of modern immunotherapeutic methods for improving the course of the tumor in patients and for better tumor control.
Understanding Colon and Rectal Cancer: Pathogenesis, Risk Factors, and Clinical Features
Colorectal cancer includes malignancies arising in the colon and rectum—two distinct yet closely related segments of the large intestine. Although they share similar biological mechanisms and treatment strategies, colon and rectal cancers differ in their pathogenesis, symptom profile, and treatment approach. A deeper understanding of these cancers helps clinicians personalize oncology protocols, select the most effective immunotherapy, and improve the prognosis for colorectal cancer patients.
Colon Cancer (Cancer of the Large Intestine)
Colorectal cancer refers to malignancies arising in the colon and rectum, two distinct but closely related segments of the large intestine. Although the biological mechanisms and treatment approaches in the therapy of colon and rectal cancer are similar, the pathogenesis, symptom complex, and treatment modalities differ. A better knowledge of these tumors will allow the oncologist to individualize protocols for colorectal cancer management.
The majority of cases of colorectal cancer arise in the colon, where the cancer develops from premalignant lesions known as adenomatous polyps. The genetic changes that lead to polyp formation and its subsequent progression to cancer result from an accumulation of mutational events, some of which affect immune checkpoint mechanisms and may alter DNA repair pathways.
The most common symptoms include changes in bowel habits, blood in the stool, unexplained weight loss, and dull abdominal pain, but early lesions may produce little or no symptoms, and therefore, screening for these tumors is important to prevent or treat them at an early stage.
Major risk factors for colon cancer include:
- Age over 50 years
- Family history of colon cancer or genetic syndromes involving colorectal cancer
- A diet high in red or processed meats
- Obesity and a sedentary lifestyle
- Chronic inflammatory bowel diseases (ulcerative colitis, Crohn’s disease)
The knowledge of the molecular mechanisms and the immune environment of the colon will help in optimizing strategies for immunotherapy for colorectal cancer that will be most effective in restoring immune system regulation of malignant immune cells.
Rectal Cancer
Rectal cancer has its origin in the distal part of the large bowel, known as the rectum, where it exhibits more aggressive local behavior than colonic cancer because of the constricting effect of the pelvis anatomy. The pathogenesis involves similar genetic and molecular alterations, but rectal cancer is more invasive to local structures and requires combined surgical treatment, radiotherapy, and immunotherapy.
Typical symptoms include rectal bleeding, tenesmus, painful defecation, and changes in the caliber of the stool. Because these symptoms can be interpreted as benign pathologies, many patients being treated for rectal cancer are diagnosed at later stages of the disease.
The important risk factors overlap with those found in colon cancer, but also include chronic inflammatory conditions in the rectal area and a greater exposure to carcinogenic metabolites since stool contact is prolonged. In recent years, the incorporation of targeted therapy and checkpoint inhibitors into treatments for advanced colorectal cancer has resulted in significant improvement in both local control and overall survival of patients.
| Feature | Colon Cancer | Rectal Cancer |
|---|---|---|
| Primary Site | Large intestine (colon) | Lower part of the large intestine (rectum) |
| Typical Symptoms | Abdominal pain, altered bowel habits, fatigue | Rectal bleeding, tenesmus, pain during defecation |
| Tumor Behavior | More likely to spread to distant organs | Often locally invasive due to pelvic anatomy |
| Treatment Approach | Surgery, immunotherapy, targeted therapy | Surgery, radiation therapy and immunotherapy |
| Prognosis | Better in early stages | Slightly lower due to late detection |
| Molecular Profile | More MSI-high tumors responsive to checkpoint inhibitors | Higher rate of local recurrence |
Role of Immunotherapy for Colorectal Cancer
The best time for immunotherapy treatment in colorectal cancer is after surgical removal of the primary colorectal tumor and, if possible, the largest metastatic foci. However, immunotherapy is also effective in advanced colorectal cancer, when surgery cannot be performed, thus offering a valuable option for patients with advanced disease or relapsing tumors.
The group of patients eligible for immunotherapy in colorectal cancer consists of those with high microsatellite instability in their tumors (MSI-H). This molecular feature is determined through genetic analysis of surgical specimens removed from the digestive tract. In the human genome, four genes are responsible for DNA replication error repair, a critical function for normal cell division. When one or more of these genes are defective, DNA damage accumulates, leading to microsatellite instability (MSI) and the formation of malignant tumor cells. A high degree of MSI occurs in about 15% of patients with colorectal cancer and in approximately 3–4% of patients with advanced disease. This group is particularly sensitive to treatment with immune checkpoint inhibitors, especially PD-1 receptor blockers. These drugs increase the activity of T-lymphocytes and other immune cells, enhancing the ability of the immune system to recognize and eliminate cancer cells.
Patients with MSI-H colon cancer should also be screened for Lynch syndrome, which is a hereditary disease, determining the high risk of tumors of various organs such as the stomach, ovaries, brain, and urinary tract. In this case, a multi-modal oncology approach appears to be justified, where the treatment of colon cancer will be connected with immunotherapy protocols of other malignancies, e.g., gastric or esophageal cancers.
Recent studies have shown that the application of immunotherapy changes the clinical criteria, especially when it is applied at earlier stages. It has been proven that the application of such treatments significantly increases effectiveness, as reflected in remission and survival rates. In leading German oncology centers, targeted therapy, immune checkpoint inhibitors, and cancer vaccines are being applied, thus stimulating a powerful immune response. The goal of the individually selected protocols is the improvement of T-lymphocyte activation, restraining of cancer growth, and preservation of healthy tissue.
Types of Immunotherapy for Colorectal Cancer
Colorectal tumor cells have also acquired numerous mechanisms for evading the body's own anti-cancer defenses. They secrete immunosuppressive substances, change the structure of the tumor microenvironment, and induce chronic inflammation, all of which weaken the immune response. The basic task of immunotherapy for colorectal cancer is therefore to counteract these mechanisms, to restore the body to its natural defense, and to induce an immune response against cancer cells.
In German oncological institutions, various classes of new drugs are used, which stimulate T and other immune cells to destroy tumor cells while protecting the healthy tissues. These new therapies are particularly effective in advanced colorectal cancer and are often combined with advanced targeted therapy or standard therapy protocols to achieve the best results.
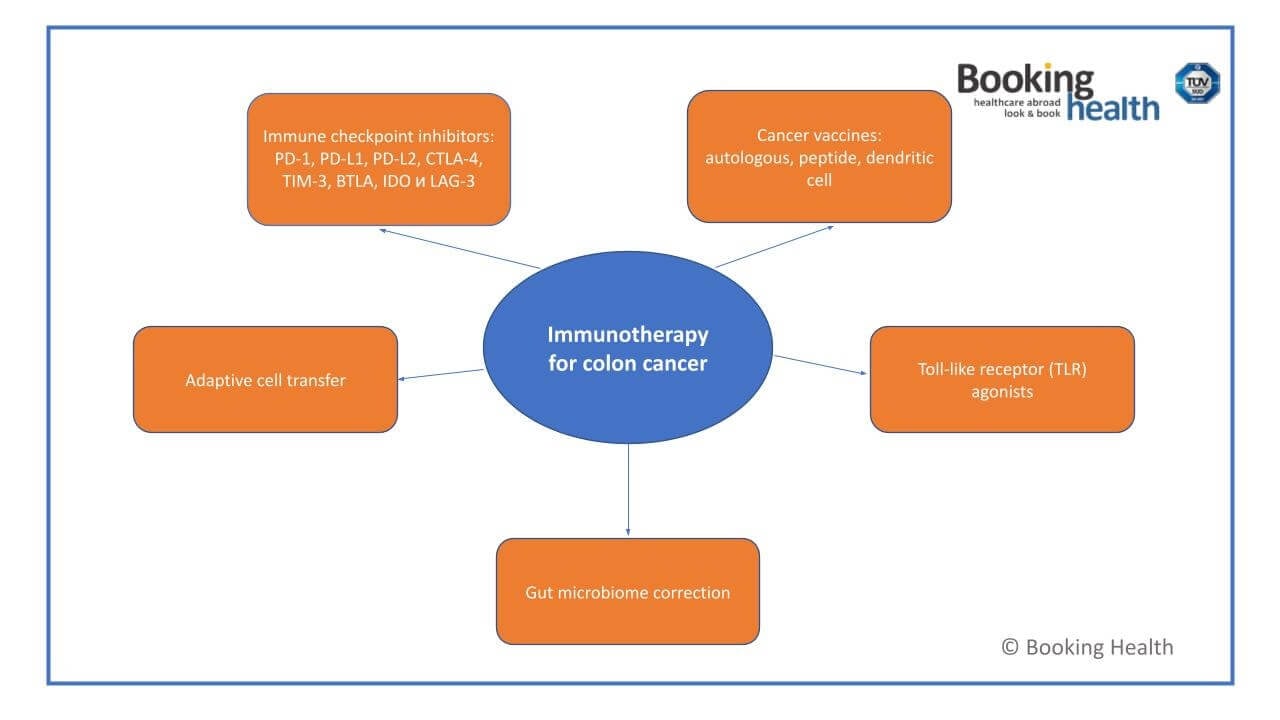
Immune Checkpoint Inhibitors
One of the greatest successes in cancer immunotherapy has been the introduction of the immune checkpoint inhibitors. Under physiological conditions, there are checkpoint proteins, e.g., PD-1, PD-L1, or CTLA-4, which the immune system uses to keep the functions of the T-cells in check, and thus to prevent damage to the healthy cells. However, the colorectal and rectal cancer cells can use these pathways and send "false" messages, thus inhibiting the immune defense.
The checkpoint inhibitors block these inhibiting messages, which means that the T-cells and other immune cells remain active and can continue to attack the cancer cells. This reactivation of the immune defense then leads to tumor shrinkage and to improved survival rates of the patients treated for advanced colorectal cancer [3].
If immune checkpoint inhibitors are combined with chemotherapy or targeted therapy, then the immune checkpoint blockade can lead to stable remission, even in advanced stages of the disease. Thus, checkpoint inhibition is one of the most effective strategies in contemporary oncology, providing a new level of precision and efficacy in cancer therapy.
Cancer Vaccines
Unlike traditional vaccines, which are used to prevent infectious diseases, cancer vaccines are designed to induce an immune response, enabling the immune system to recognize and eliminate neoplastic cells. In the context of immunotherapy for colorectal cancer, peptide and autologous vaccines have been applied to T-cells, which are exposed to known tumor antigens to sensitize them to specifically recognize and destroy neoplastic cells [4].
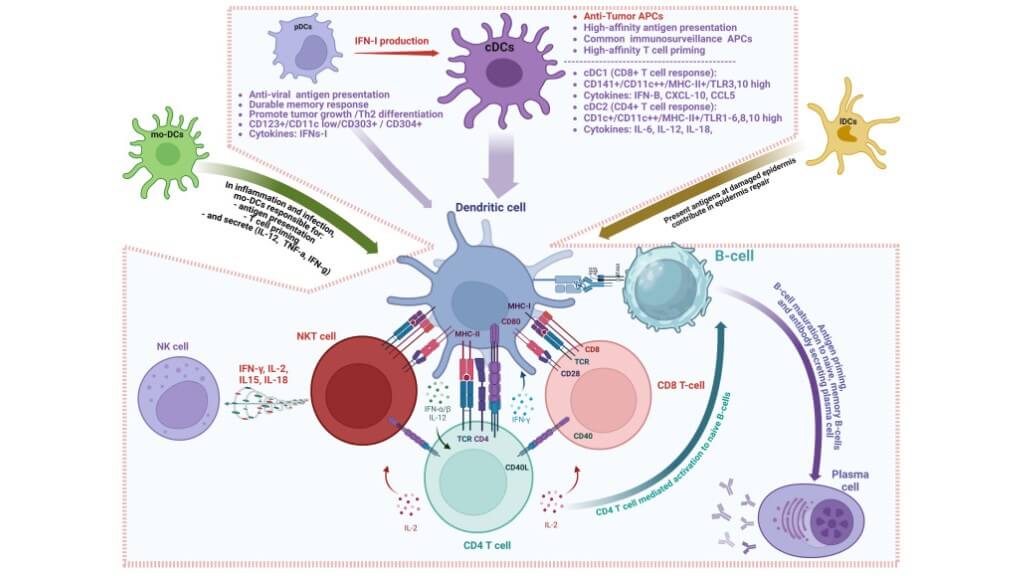
Of all vaccines, the most valuable in the therapeutic sense are the dendritic cell vaccines. These vaccines act as "teachers" of the immune system because they instruct the T-cells what targets to attack. The role that they play in the "teaching" of the immune system to initiate an anti-tumor immune response has been the subject of Nobel Prize-winning research, which emphasizes their importance.
The use of dendritic vaccines in the clinical setting has been studied in early and advanced colorectal cancer in order to improve the control over the neoplasm. These therapies increase the activity of the immune cells and raise the ability of the body to suppress neoplastic growth, while at the same time allowing the normal cells to be undisturbed.
The vaccines for colon cancer are:
- Autologous: These vaccines, prepared using tumor material from the patient, enable the individual’s immune system to recognize the tumor’s unique antigenic profile and to mount an appropriate immune response.
- Peptide vaccines: Through reacting to defined molecular targets like carcinoembryonic antigen (CEA) and beta-hCG, these vaccines activate the T-cells and, therefore, make the therapy more selective and reduce the side effects.
Prof. Frank Gansauge: How Dendritic Cell Therapy is Transforming Modern Cancer Treatment
Adoptive Cell Therapy
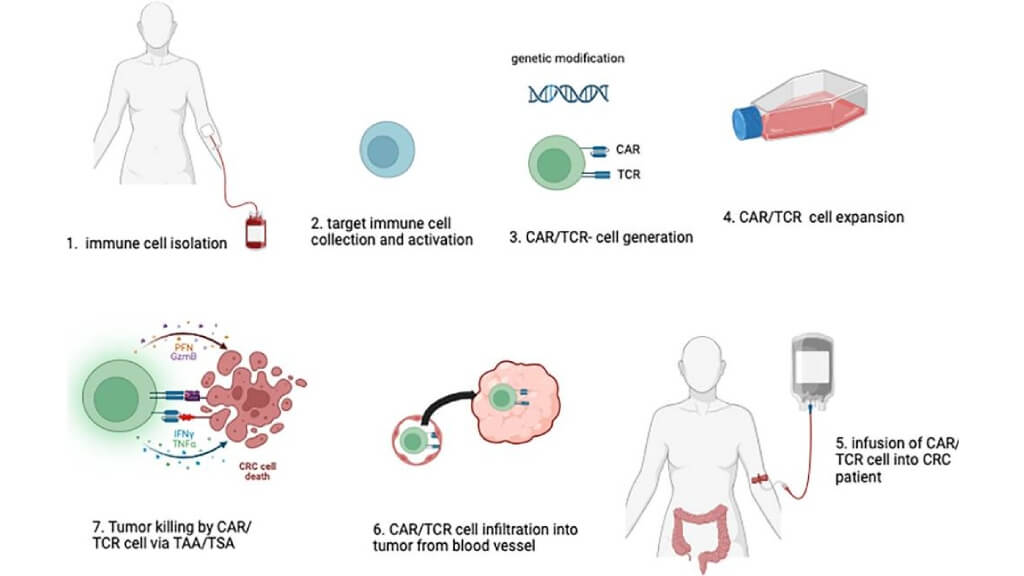
Adoptive cell therapy (ACT) is one of the most individualized forms of immunotherapy in modern oncology. During the procedure, the patient’s T-cells or other immune cells are extracted from the patient's blood, genetically modified, expanded in culture, and reinfused into the body. These augmented cells act as an elite army trained to seek and destroy cancer cells that have escaped the control of the natural immune checkpoints of the body [5].
For patients with colorectal cancer with advanced disease who are no longer sensitive to standard treatments, ACT can offer a breakthrough. It increases the precision of the immune response of the organism, encourages the immune response, and gives a new hope of long-term remission.
Toll-like Receptor (TLR) Agonists
Toll-like receptors (TLRs) constitute a vital mechanism of the innate immune system, which is responsible for the detection of invading harmful agents. Unfortunately, many tumor cells have found methods of escaping the detection of these receptors. TLR agonists are drugs that "wake up" the immune defense by activation of these receptors, and thereafter set into play a cascade of immune modulatory processes.
Upon stimulation, immune cells secrete cytokines that recruit T-cells and enhance the immune response, leading to subsequent tumor destruction. TLR agonists are frequently used in conjunction with other methods of immunotherapy, based on increased immune effectiveness, especially in patients with advanced colorectal cancer.
Gut Microbiome Correction
It has recently become known that the intestinal microbiome – trillions of beneficial bacteria that reside in the intestine – plays a decisive role in the success of immunotherapy. An unbalanced microbiome impairs immune cell activation, diminishes the specific T-cell response, and reduces the effectiveness of anti-cancer treatments. Restoring gut health with diet, probiotics, and fecal microbiota transplant can facilitate the results of colorectal cancer immunotherapy. A balanced microbiome allows for a vigorous immune response, permits efficient targeting of tumor cells, while, at the same time, preserving the surrounding healthy tissue.
| Aspect | Colon Cancer Immunotherapy | Rectal Cancer Immunotherapy |
|---|---|---|
| Integration with Radiation | Radiation therapy rarely needed; systemic immunotherapy is often sufficient | Frequently combined with radiation therapy due to pelvic anatomy and higher local recurrence risk |
| Immune Targeting | Systemic activation of T-cells and immune cells targeting colon tumor cells | Requires additional local immune activation strategies to overcome stronger local immunosuppressive microenvironment |
| Timing with Surgery | Usually administered after standard surgical resection | Timing carefully coordinated with surgery and radiation to avoid damage to surrounding pelvic tissues |
| Delivery Approach | Standard intravenous checkpoint inhibitors, vaccines, adoptive cell therapy | Same systemic therapies, but may require higher local doses or localized vaccine/injection strategies |
| Response Patterns | Tumors respond mainly via systemic T-cell activation; lower local recurrence | Tumors may require combined systemic and local immune activation; higher risk of residual disease in pelvic tissue |
How is Colorectal Cancer Immunotherapy Carried Out?
The immune checkpoint inhibitors, for example, PD-1/PD-L1 and CTLA-4, are administered intravenously under medical supervision in either an outpatient or day hospital setting. The time intervals between doses are usually in the range of every 3-6 weeks, depending upon the treatment regimen for the cancer. These agents are generally well-tolerated and effective in stimulating the immune system, including T-cell activity. Side effects are usually mild and may include abdominal pain, fatigue, anorexia, nausea, and diarrhea.
The vaccines for the colon cancers are usually administered subcutaneously in a day hospital setting. In the case of dendritic cell vaccines, which create a target-specific immune response, a single injection will accomplish long-term anticancer immunity. This procedure is designed to instruct the immune cells to recognize and attack cancer cells, but leave the healthy tissues, which are not affected, intact. If desired, more injections can be given, depending upon the clinical needs of the patient.
The adoptive cell therapy necessitates an inpatient procedure because, usually, pre-treatment with high-dose chemotherapy is employed before the infusion of the modified CAR T-therapy, which is used for patients with advanced disease. The laboratory phase in the generation of CAR T-cells may take up to three weeks. Typically, two visits to the clinic are required. The first one is for the preparatory procedures, and another is for the immunotherapy infusion. This individualized therapeutic approach directs the immune system against tumor proliferation, which often does not respond to conventional treatment modalities.
The toll-like receptor agonists and reformation of the gut microbiome are going to be used and analyzed in clinical trials. These create a rapid immune response, stimulate the immune cells, and are on the brink of becoming an important area of colorectal cancer treatment.
Benefits of Colorectal Immunotherapy Treatments
In countries with a well-developed health system, cancer immunotherapy is increasingly being instituted as a first line of treatment for colon cancer, while at first it was reserved for patients with advanced colorectal cancer, including those who have metastatic tumors or therapy-resistant tumors. The average survival rate of patients with metastatic colon cancer is about 6 months after failure of chemotherapy and targeted therapy, since uncontrolled tumor growth has taken place, standard treatment has little or no effect in prolonging life. In these areas of limited medical resources, tumor resistance usually results in symptomatic and palliative care being the only means of treatment left to the physician.
The advent of immunotherapy has greatly changed this picture. For instance, adoptive cell therapy may now increase the average survival of patients with metastatic colon cancer from 14 to 28 months, since genetically modified T-cells and other immune cells can launch a potent immune attack on the cancer cells found in the host.
Following these successful efforts, immune checkpoint inhibitors and cancer vaccines have been introduced earlier in the course of the disease, usually after surgical excision of the primary tumor when it is possible. The earlier immunotherapy can be used, the more effective the treatment is, since the immune system is trained to attack remaining cancer cells before widespread metastases occur.
Clinical experience and clinical trials have shown that in patients who have received immunotherapy for advanced colorectal cancer, the cytotoxic T-cells found in the blood begin to increase rapidly. This is an indication that these immune cells attack both the primary tumor and metastatic sites, resulting in slowing down the disease progression, even in some cases resulting in remission. This demonstrates the remarkable capabilities of modern oncology, harnessing the body’s defenses to control tumor growth and improve survival in patients with colorectal cancer.
| Cancer stage | Response to standard treatment protocol | Response to standard treatment protocol + Immunotherapy |
|---|---|---|
| Stage 3 | 50% | 20% |
| Stage 4 | 70% | 50% |
*According to Booking Health data
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans for colorectal cancer with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for colorectal cancer with leading specialists in this field.
Immunotherapy Journey: Dendritic Cell Treatment with Booking Health
Frequently Asked Questions of Our Patients About Immunotherapy for Colon Cancer in Germany
Get a ConsultationImmunotherapy for colon cancer involves using medications to stimulate the patient's immune system to recognize and attack cancer cells. It targets specific proteins or receptors on the cancer cells, enhancing the body's natural defenses.
Benefits include a targeted treatment approach, fewer side effects compared to traditional therapies, and the potential for long-term remission by stimulating the immune system. It offers new hope for patients with advanced or resistant colon cancer.
Modern immunotherapy for colon cancer in Germany includes immune checkpoint inhibitors, dendritic cell vaccines, adoptive T-cell transfer, and experimental methods such as TLR agonists. These treatments help the immune system detect and attack tumor cells more effectively.
Dendritic cell therapy for colon cancer is showing promising results, especially in clinical trials. By stimulating the immune system to recognize tumor antigens, this therapy can slow disease progression, reduce relapse risk, and improve overall survival when combined with other treatments.
The cost of immunotherapy in Germany varies depending on the chosen method, the hospital, and the patient’s condition. On average, prices start from €20,000–30,000 per course. Booking Health helps patients save up to 70% by arranging treatment directly with leading German clinics.
Yes, Booking Health colon cancer support includes selecting the best clinic, negotiating costs, translating medical reports, and organizing the entire trip. Patients benefit from transparent pricing, professional guidance, and coordination throughout the whole treatment journey.
Stage 4 colon cancer immunotherapy can be effective in controlling tumor growth, especially when standard chemotherapy fails. It helps extend survival and improve quality of life by activating the immune system to attack cancer cells, even in advanced metastatic cases.
The side effects of immunotherapy for colon cancer are usually milder than those of chemotherapy. Patients may experience fatigue, appetite loss, diarrhea, or mild skin reactions. Most symptoms are temporary and manageable under medical supervision in German clinics.
You can begin by booking colon cancer treatment in Germany through Booking Health’s platform. Simply send your medical records, and their team will suggest the best options, provide cost estimates, and guide you through every step of the process.
Adding immunotherapy significantly increases the effectiveness of colon cancer treatment. At stage 3, the response rate to standard regimens increases from 50% to 80% and at stage 4 from 30% to 50%. This approach improves survival and helps to achieve stable remission even with advanced disease.
At stage 4 colon cancer, standard treatment gives a positive response in 30–40% of cases while adding immunotherapy increases the effectiveness to 50%. This means that even patients with metastases have a chance for stable improvement and prolongation of life.
Combining immunotherapy with standard colon cancer treatment activates the patient's natural immunity, enhances the effect of drugs and reduces the risk of relapse. This approach increases the sensitivity of the tumor to therapy and promotes long-term remission without significant deterioration in well-being.
The cost of immunotherapy in the treatment of colon cancer depends on the type of drug, the stage of the disease and the duration of the course. On average the price is formed individually after diagnosis, but patients note that the results exceed the costs due to the long-term effect.
Yes. Immunotherapy for rectal vs colon cancer activates T-cells and other immune cells. Methods like vaccines and adoptive cell therapy for CRC target tumor cells, while protecting healthy tissue, improve outcomes even in advanced cases. Booking Health support of CRC immunotherapy in Germany ensures access to leading clinics, personalized protocols, and coordination for advanced treatment options.
Immunotherapy shows different patterns of effectiveness in rectal vs colon cancer, largely due to differences in tumor location and the local immune microenvironment. Rectal tumors often require both local and systemic immune activation, whereas colon tumors generally respond primarily to systemic therapy.
Yes. Immunotherapy combination for CRC with chemotherapy or radiation enhances immune response and tumor control, providing a synergistic effect that improves outcomes for both colon and rectal cancer patients.
Administration of immunotherapy for colorectal cancer is tailored to the tumor site. Studies evaluating the effectiveness of immunotherapy for rectal vs colon cancer show that colon tumors generally respond better to systemic therapy, whereas rectal tumors may require additional local immune activation for optimal results.
In Germany colon cancer patients can access full spectrum of immunotherapy options. Treatments are individualized and administered in specialized centers. Also they are combined with standard oncology care to enhance immune response.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Zentrum für Krebsregisterdaten. Colorectal Cancer. https://www.krebsdaten.de/Krebs/EN/Content/Cancer_sites/Colorectal_cancer/colorectal_cancer_node.html
[2] Gholamreza Roshandel, Fatemeh Ghasemi-Kebria, Reza Malekzadeh. Colorectal Cancer: Epidemiology, Risk Factors, and Prevention. Cancers (Basel). 2024 Apr 17;16(8):1530. doi: 10.3390/cancers16081530. [DOI] [PMC free article]
[3] Frontiers in Immunology. Immune checkpoint inhibitors in colorectal cancer: limitation and challenges. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1403533/full
[4] Mahmoud Singer, Jennifer Valerin, Zhuoli Zhang et al. Promising Cellular Immunotherapy for Colorectal Cancer Using Classical Dendritic Cells and Natural Killer T Cells. Cells. 2025 Jan 22;14(3):166. doi: 10.3390/cells14030166. [DOI] [PMC free article]
[5] Frontiers in Immunology. Adoptive immune cell therapy for colorectal cancer. https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1557906/full
Read:
Cancer immunotherapy in Germany
Article menu:
- Understanding Colon and Rectal Cancer: Pathogenesis, Risk Factors, and Clinical Features
- Role of Immunotherapy for Colorectal Cancer
- Types of Immunotherapy for Colorectal Cancer
- How is Colorectal Cancer Immunotherapy Carried Out?
- Benefits of Colorectal Immunotherapy Treatments
- A Medical Journey: Every Step of the Way With Booking Health
- Frequently Asked Questions of Our Patients About Immunotherapy for Colon Cancer in Germany
Don't know where to start?
Contact Booking Health
















