Ovarian cancer is the 8th most common type of cancer in women, with more than 320,000 new cases registered in 2022. Around a quarter (25%) of all new cases were diagnosed in women aged 75 and older. Taking into account that early symptoms are subtle and non-specific, especially among older women, ovarian cancer is often found at advanced stages. Although highly curable in the early stages, ovarian cancer stage 4 presents a challenge with survival rates generally not exceeding 30%.
Every woman's health is a complex mechanism that requires dedicated care and love. Women of reproductive age are faced with even more life-turning choices when diagnosed with ovarian cancer stage 4, as there are few treatment options that spare reproductive function. Of course, survival and optimal quality of life are the ultimate priorities in stage 4, yet choosing between life and the possibility of having your own kids in the future is definitely devastating. However, hope goes hand-by-hand with new solutions. And innovative methods of treatment are called to turn the tables and win more of your precious time while slowing the progression of the disease.
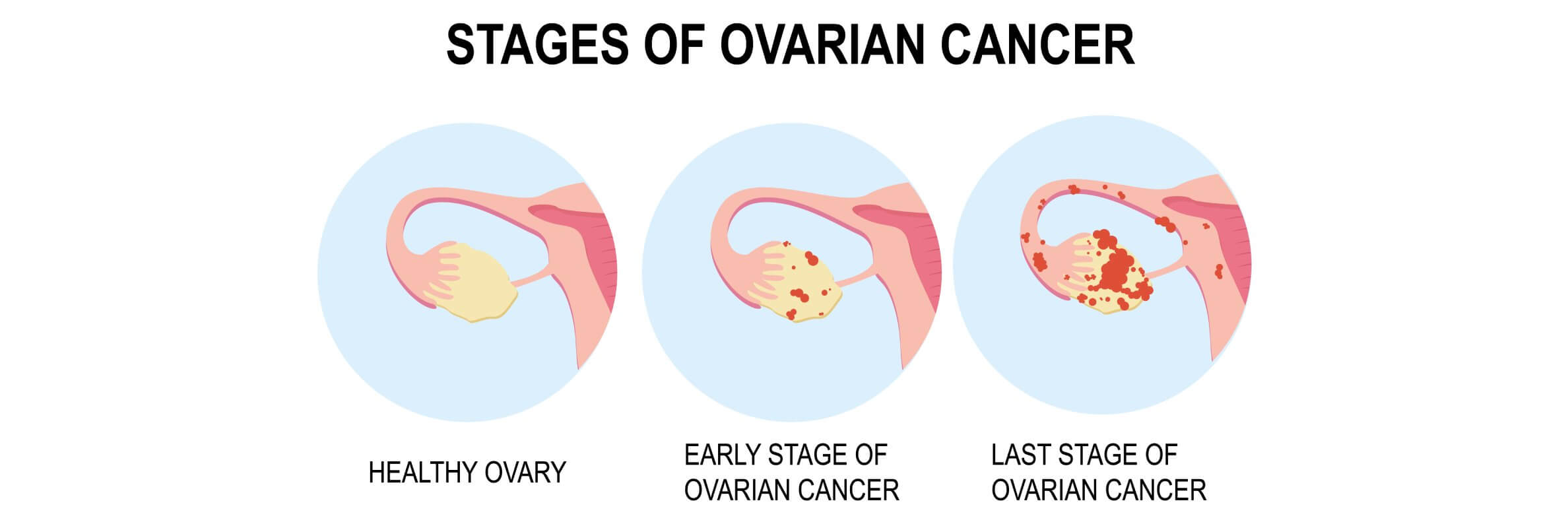
Understanding Stage 4 Ovarian Cancer
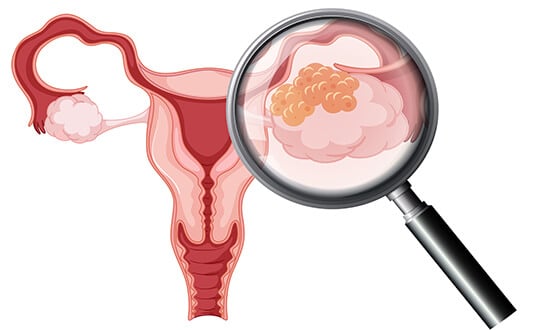
Stage 4 ovarian cancer is a metastatic stage of the disease. This means that the cancer has spread beyond the ovaries and the pelvic region to other distant organs and tissues, such as the lungs, liver, or bones. As the cancer spreads, women may experience additional symptoms such as heartburn, indigestion, back pain, or dull aches in the bones. This is exactly what makes ovarian cancer treatment at advanced stages such a complicated issue.
Standard Treatments for Stage 4 Ovarian Cancer
At stage 4, standard ovarian cancer treatment options typically include surgery, chemotherapy, and hormones for hormone-sensitive types of ovarian cancer. The combination of treatments suggested depends on the characteristics of the tumor, the previous treatment strategy and its success, and your health status.
Surgery for Stage 4 Ovarian Cancer
Surgery is a matter of choice even for advanced stages of ovarian cancer treatment. When cure rates are still high, fertility-sparing surgery is preferred whenever possible. In all other cases, primary cytoreductive surgery is performed to reduce the number of tumors in the abdomen that have disseminated from the pelvic region. When complete cytoreduction is impossible (either because of your health condition or for other reasons), a laparoscopic procedure is recommended to assess the extent of disease spread. Intraoperative biopsy (malignant tissue sampling) may also be performed during this laparoscopic evaluation.
Chemotherapy for Stage 4 Ovarian Cancer
Systemic chemotherapy is the cornerstone of ovarian cancer treatment at terminal stages. It often accompanies surgery in complex management of ovarian cancer in the advanced stages of the disease. Chemotherapy for ovarian cancer stage 4 typically requires a combination of several chemotherapeutic agents. Testing for BRCA1 and BRCA2 is crucial before starting therapy.
Advanced Stage 4 Ovarian Cancer Treatment Options
Innovative cancer treatments are gaining worldwide attention for their breakthrough effects, especially in the treatment of various types of gynecological cancer. Targeted therapy and immunotherapy, dendritic cell vaccines and chemoembolization, HIPEC and PIPAC are just a few of the treatments that have proven effective for 4 stages of ovarian cancer.
Targeted Therapy for Stage 4 Ovarian Cancer
Targeted therapy is a type of therapy that utilizes specific drugs that target genetic changes in malignant cells. These genetic mutations lead to the production of specific proteins or signaling molecules that help cancer cells grow and multiply. Targeted therapy for ovarian cancer is widely used for advanced stages of the disease with monoclonal antibodies and PARP inhibitors being included in the official guidelines.
Monoclonal antibodies are typically used in combination with chemotherapy after the completion of the therapy program. These drugs can significantly improve progression-free survival (up to 85%) and prolong overall survival. PARP inhibitors may also be administered post-chemotherapy. These drugs interfere with the process of DNA repair inside malignant cells, leading to their death.
Before starting treatment with PARP inhibitors, BRCA1 and BRCA2 testing is required to verify benefit from this treatment. PARP inhibitors are typically a therapy of choice when there is an inadequate response to chemotherapy. PARP inhibitors are also well-tolerated when used in combination with monoclonal antibodies due to the lack of overlapping toxicities. Either used as a monotherapy or in combination with other treatments, PARP inhibitors demonstrate clearly improved progression-free survival (up to 40%), which verifies the exceptional benefit of targeted therapy for ovarian cancer patients.
Immunotherapy for Stage 4 Ovarian Cancer
Immunotherapy utilizes your own immune system to recognize and eliminate malignant cells. Immunotherapy for ovarian cancer is still under investigation, but it has already shown first robust results in several clinical studies. One of the best-known and most studied classes of agents are immune checkpoint inhibitors. These drugs help stop cancer cells from evading the immune response by targeting specific signaling molecules that are crucial for the immune response. PD-1 and PD-L1 inhibitors are the drugs currently being studied in combination with other therapies such as targeted therapy and systemic chemotherapy to reduce disease recurrence and improve tumor control.
Dendritic Cell Therapy for Stage 4 Ovarian Cancer
Dendritic cell therapy is a form of personalized immunotherapy that uses a patient's own immune cells to eliminate malignant cells. Dendritic cells play a key role in the immune response by helping specific immune killers track down and destroy cancer cells. Dendritic cell vaccines are a novel form of immunotherapy where the therapy focuses on creating specific anti-tumor immunity based on your own cancer type. The process of dendritic cell therapy consists of the following steps:
- Drawing blood and harvesting dendritic cells from it.
- Obtaining the tumor specimen (either from surgery or from a liquid biopsy). The whole process is an outpatient procedure that does not require a hospital stay.
- Cell cultivation. Dendritic cells are cultured and multiplied in a special incubator influenced by numerous nutritional factors. At the initial stages of this process, tumor antigens are added to these cells.
- Antigen exposure. Dendritic cells make their "first contact" with tumor antigens and train to recognize them.
- Vaccine administration. The vaccine containing specific tumor-oriented dendritic cells is injected subcutaneously in the groin area.
Dendritic cell vaccination is a simple and time-sparing procedure. As opposed to other systemic treatments such as chemotherapy or radiation therapy, it does not cause any significant side effects. Several studies have focused on dendritic cell therapy in the treatment of ovarian cancer, including recurrent and chemotherapy-resistant types. These studies revealed that chemotherapy-sensitive patients with recurrent ovarian cancer who were administered a dendritic cell vaccine reported considerably longer progression-free survival rates (36 and 44 months). Apart from reducing recurrence, dendritic cell therapy improves overall survival when combined with other systemic treatment approaches. Even though studies are still ongoing, dendritic cell vaccines represent a valuable novel alternative to standard systemic treatments.
HIPEC for Stage 4 Ovarian Cancer
HIPEC (hyperthermic intraperitoneal chemotherapy) is a type of regional chemotherapy in which heated chemotherapy is delivered into the abdominal cavity. Since cancer cells disseminate to other organs and regions of the body at advanced stages, the abdomen is one of the most common sites for metastatic tumors. The abdomen covers a large area, and small metastatic lesions are extremely difficult to reach. HIPEC solves this problem by delivering chemotherapy directly to the tumor site. On the other hand, hyperthermia increases the absorption of chemotherapeutic agents as well as the sensitivity of the tumor to therapy by interfering with DNA repair. In addition, hyperthermia itself is also capable of inducing programmed cell death.
HIPEC can be administered during or immediately after cytoreductive surgery. Several studies have demonstrated its indisputable benefit for ovarian cancer treatment, including recurrent ovarian cancer. In a large multicenter randomized trial, patients who received HIPEC after cytoreductive surgery for recurrent ovarian cancer showed significantly improved survival: 54.3 vs 45.8 months in the surgery without HIPEC group. Another large multicenter study proved that adding HIPEC to surgery can improve disease recurrence rates and reduce the risk of death.
The HIPEC procedure is definitely beneficial for the patients in terms of clinical efficacy, although it is associated with a number of side effects. The most common adverse reactions were abdominal pain, discomfort, hepatotoxicity, and blood disorders (anemia). This may be one of the reasons why HIPEC is not yet a standard practice for ovarian cancer.
PIPAC for Stage 4 Ovarian Cancer
PIPAC (pressurized intraperitoneal chemotherapy) is a minimally invasive surgical procedure that administers chemotherapy into the abdominal cavity by means of pressurized aerosol. This aerosol is delivered under pressure, which enables deeper tissue penetration and a more widespread distribution of the drug.
While still under research, PIPAC for ovarian cancer recommended itself as a beneficial palliative treatment when other systemic therapies are not effective. One of the largest studies for the usage of PIPAC in recurrent ovarian cancer demonstrated that over 80% of patients had a valuable clinical benefit. Studies in other cancers (gastric peritoneal metastases) also found PIPAC to be extremely beneficial in terms of overall survival compared to systemic therapy alone (19.1 vs 10.7 months).
PIPAC may also be more patient-friendly than other treatment options, including HIPEC, as reported by some studies. Due to the fact that chemotherapy is administered regionally, there are no systemic side effects from chemotherapy. The procedure itself is done by means of laparoscopy (a minimally invasive surgical technique), which significantly reduces the risk of major intra- and postoperative complications such as infection. The overall better tolerability of PIPAC turns out to be an advantageous innovative approach for recurrent ovarian cancer without having serious adverse effects on the patient's health.
Interventional Radiology for Stage 4 Ovarian Cancer: Percutaneous Ablation and Transarterial Embolization
Minimally invasive, image-guided techniques are becoming increasingly integrated into treatment protocols for advanced ovarian cancer. These methods present a valuable alternative for patients who are not candidates for surgery, enabling precise destruction of tumor sites under the guidance of imaging technologies such as computed tomography (CT) and ultrasound.
Thermal ablation, including radiofrequency ablation (RFA) and microwave ablation (MWA), has been used as a complementary modality for metastatic and recurrent ovarian carcinoma. These approaches are especially effective for disease recurrence affecting the peritoneal surface or the liver. Thermal ablation, which uses elevated temperatures to irreversibly destroy malignant cells, is increasingly being used in multimodal cancer treatment plans, although it is not yet part of a standard protocol. Clinical studies have demonstrated local tumor responses of more than 90% at one-year intervals. Above that, thermal ablation is commonly accompanied by notable symptom relief, specifically in reducing pain levels. MWA, which is known for its ability to produce extensive eradication zones, is particularly beneficial for deep pelvic or retroperitoneal secondary ovarian malignancies.
Cryoablation employs sub-zero temperatures to cause tumor necrosis. It has emerged as a promising approach for recurrent ovarian tumors, including lesions located near critical anatomic structures such as the bowel or ureter. Scientists suggest that cryoablation can lead to disease control of around 70% in patients with recurrent pelvic tumors, which is of absolute advantage to enhance quality of life by successfully managing intestinal obstruction. It is especially beneficial in cases where repeated surgical debulking is not indicated or has already failed.
Electrochemotherapy for stage 4 ovarian cancer is a novel technique that uses electrical impulses to eliminate malignant foci while administering chemotherapeutic drugs via injection. Electro-chemotherapy (ECT) is being explored for challenging cases of ovarian cancer tumor recurrence. Doctors reported tumor response rates of around 70% for cases when standard treatment options, including surgery and chemoradiation, have failed. ECT is also capable of activating specific immune responses aimed at eliminating the residual malignant cells. It is especially crucial for complex management of terminal cases of advanced ovarian cancer. You can find the cost of electrochemotherapy on the Booking Health website; electrochemotherapy cost may be somewhat different depending on the healthcare facility.
Prof. Kovács on Electrochemotherapy – How Electric Pulses Help Chemo Actually Work
Regional chemotherapy for ovarian cancer stage 4 breaks through widespread drug resistance. The problem with systemic chemotherapy is that drugs dilute in 5-7 liters of blood, reaching tumor diluted, that is – a significant portion of the medication is wasted.
For stage 4 ovarian cancer regional chemotherapy solution includes isolation of abdominal circulation, delivering drugs directly to tumor site at maximum concentrations, and removing drugs through chemofiltration before they enter systemic circulation. These protect patients while exposing tumor to lethal chemo levels. Hypoxic conditions enhance effect: drugs produce augmented cytotoxicity, multiple times over normal effect.
You can find more practical information about ECT and regional chemo in the interview with Prof. Aigner, who has been practising these methods for almost 45 years.
Chemoembolization is a form of regional chemotherapy, which involves administering chemotherapeutic drugs directly into the blood vessels feeding a tumor. This comes alongside emboli (small blocking substances) that simultaneously block the blood supply. As a result, due to such technical characteristics it is possible to deliver high-dose chemotherapy while minimizing systemic exposure.
In ovarian cancer, chemoembolization is considered for patients with isolated metastatic lesions, for example, in the liver, or those who did not respond to systemic treatments. Chemoembolization was found to be particularly effective in previously treated patients with platinum resistance, as it improved overall disease control. The technique also demonstrated high response rates (70-90%), statistically reducing the risk of disease recurrence.
Although not yet a standard of care, chemoembolization for ovarian cancer is well tolerated by patients compared to systemic therapy. The regional effect of chemotherapy prevents systemic exposure and maximizes the regional effect on metastatic lesions, which result in a particularly good therapeutic effect. Less adverse effects combined with maximum efficacy make chemoembolization an advantageous choice for stage 4 ovarian cancer.
| Procedure/Characteristics | Surgery | Systemic Chemotherapy | Targeted Therapy | Dendritic Cells | HIPEC | PIPEC | Chemoembolization |
|---|---|---|---|---|---|---|---|
| Response rate | 15-30% | Less than 10% | 35-45% | 60-80% | 40-55% | 35-45% | 35-45% |
| Recurrence rate | No significant impact on recurrence | Reduces recurrence for 13 of the patients | Reduces recurrence for up to 40% | Reduced recurrence rates | Reduced recurrence for several months | Extended progression-free time for several months | Extends progression-free time up to 1 year when combined with other treatments |
| Overall survival | ~20-30% | ~20% for advanced cancer | ~50% for advanced cancer (with biomarkers) | ~80% for advanced cancer | 30-50% | 30-50% | ~60% for advanced cancer |
| Adverse effects | Pain, infection, indigestion | Hair loss, nausea, vomiting, blood disorder | Mild to moderate (rash, fatigue) | Minimal (flu-like symptoms) | Pain, indigestion | Mild (abdominal pain, nausea, temporary inflammation) | Mild (localized discomfort) |
Stage 4 Ovarian Cancer Treatment Stories: Regain Hope with Innovative Treatment Options
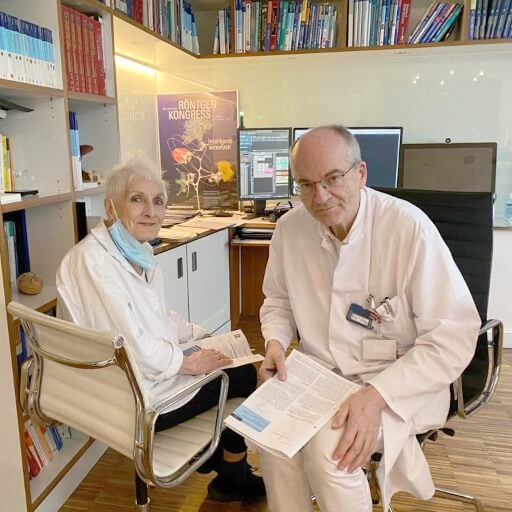
The management of gynecological cancer presents a complicated task indeed, both for you as a patient and for your oncologist. At times, you may feel that there is no visible progress or that nothing more can be done in your case. However, you are not alone in this battle. Hope will always come for those who seek it, and this is exactly what happened to Sonja Maria from Sweden. Maria was diagnosed with high-grade serous tubular ovarian cancer stage 4A, with peritoneal involvement. Looking for another opinion, she went to a German oncology hospital renowned for gynecological cancer treatment at advanced stages. Ms. Holst underwent surgery, but it was more than just a mere surgical procedure. She gained a supportive environment and overwhelming care that is essential for patients on their journey of dealing with cancer.
Ms. Gasparian was also looking for hope and alternative treatment options, so she accompanied her beloved mother to Germany for immunotherapy. Ms. Gasparian's mother was diagnosed with stage 4 ovarian cancer, and they were in desperate need of action. After learning about dendritic cell therapy, they grabbed an opportunity to organize the treatment abroad at Prof. Gansauge's clinic. Immunotherapy for ovarian cancer is a novel yet promising approach that not only improves the patient's quality of life, but also provides valuable clinical benefits in terms of disease control and tolerability of the procedure itself. In addition to the exceptionally comfortable atmosphere at the clinic, Ms. Gasparian also highly appreciated the quality of service and organization of her treatment. There was no need to worry about visas, translations or coordinating other processes, which is invaluable for patients with various cancer types undergoing treatment abroad.

Explore Your STage 4 Ovarian Cancer Treatment Options with Expert Support
Finding the most effective method as well as the best hospitals for ovarian cancer treatment is not only time-consuming, but also quite stressful. Already being tired from a long search for advanced ovarian treatment options, you may be wondering if there is a way to delegate such a delicate yet crucial matter. And the answer is yes, Booking Health can do it for you.
Doubts such as "What if this is a scam?" or "What if this is another unreliable source of information that suggests air instead of real solutions?" may cross your mind. However, Booking Health is a reputable company with over 10 years of experience in the medical tourism market. We have advised more than 100,000 patients around the world and organized ovarian cancer treatment abroad for thousands of international patients.
Booking Health assists in finding the best hospitals for ovarian cancer therapy without compromising on quality, yet saving money. The company offers all-inclusive services, including:
- Development of personalized treatment strategies
- Selection of the most suitable clinic in your case
- Preliminary consultations with doctors to develop a complex management plan
- Follow-up care, even when you return home after completing your treatment
- Coordination of your stay in a foreign country
- Visa and airline ticket assistance
- No additional costs and transparent prices excluding fees for international patients
Remember that timely intervention can save your precious time and halt disease progression. Top gynecological clinics offer multiple innovative treatment methods to not only improve your quality of life, but also to prevent disease recurrence and bring back the hope of living life as it is.
Modern Cancer Treatment: Patient Journeys with Booking Health
Frequently Asked Questions of Our Patients About Stage 4 Ovarian Cancer
Send request for treatmentStage 4 ovarian cancer is the most advanced form of the disease, where cancer has spread to distant organs such as the liver, lungs or lymph nodes outside the abdominal area.
While stage 4 ovarian cancer is generally not considered completely curable, it is treatable. Many patients can achieve remission and live for a long time with appropriate care.
Treatment typically includes a combination of surgery (to remove as much of the tumor as possible) and systemic therapies (chemotherapy). Targeted therapies and, in some cases, immunotherapy may also be considered.
Chemotherapy remains a foundation of treatment and can be highly effective in reducing tumor burden, relieving symptoms, and prolonging overall survival, especially when combined with other therapies.
Immunotherapy shows promise in advanced ovarian cancer, though it is not a part of standard treatment protocol yet. Select patients may benefit from specific immunotherapy combinations depending on the molecular profile of their cancer.
The best hospitals for ovarian cancer with expertise in gynecologic oncology offer the most comprehensive care, including access to advanced treatment options and clinical trials. Many of these international clinics are located in Germany.
Survival varies based on many factors, including the patient's overall health, response to treatment, and cancer subtype. With modern therapies, patients can live for several years after diagnosis.
In Germany, stage 4 ovarian cancer treatment costs between €25,000 and €280,000, depending on the method. For example, dendritic cell therapy costs €20,000 - €38,000. HIPEC therapy costs €55,000-€75,000 and PIPAC一€18,000-€20,000.
Surgical treatment of stage 4 ovarian cancer provides a response rate of 15–30%. Its main goal is to reduce the tumor mass and create conditions for more effective subsequent therapy.
Systemic chemotherapy has the lowest response rate of less than 10%. It is used in combination with targeted or regional methods to control the progression of the disease.
Targeted therapy in stage 4 ovarian cancer shows a 35–45% response rate, especially in the presence of BRCA mutations. The use of PARP inhibitors significantly prolongs the progression-free period.
Dendritic cell therapy provides 60–80% responses in patients with chemotherapy-sensitive relapses. In addition it prolongs the progression-free period to several months.
HIPEC shows a 40–55% response rate and can extend overall survival to several months. The method increases the sensitivity of the tumor to chemotherapy and reduces the risk of relapse.
PIPAC shows a 35–45% response rate for recurrent stage 4 ovarian cancer. More than 80% of patients experience clinical improvement, including symptom reduction and progression.
Chemoembolization (TACE) achieves 35–45% responses and extends the progression-free period to 1 year when combined with other treatments. The method is particularly effective for isolated metastases, such as in the liver, with minimal side effects.
Dendritic cell therapy has a survival rate of 80%, targeted therapy has a survival rate of about 50%, HIPEC and PIPAC provide 30–50% and chemoembolization has a survival rate of up to 60%. This is significantly higher than the results of standard chemotherapy (~20%).
Standard chemotherapy causes nausea, hair loss, anemia and other severe side efftcts. Innovative methods usually have mild side effects such as short-term pain or discomfort and flu-like symptoms. Immunotherapy is best tolerated.
For stage 4 ovarian cancer treatment is personalized. Doctors focus on reducing tumor spread, controlling symptoms and improving quality of life. Approaches may combine surgery, targeted therapies or immune support. Every method is chosen according to tumor location and patient condition.
The best hospitals treat many advanced ovarian cancer cases yearly. They coordinate care across specialists adjusting procedures as the disease changes.
Germany is the perfect example of highly organized cancer care with centers experienced in complex ovarian cancer; multidisciplinary teams provide rapid evaluation and adapt treatment as needed – combining innovative therapies and supportive care.
Choose treatment abroad and you will for sure get the best results!
Authors:
The article was edited by medical experts, board certified doctors Dr. Nadezhda Ivanisova and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
National Ovarian Cancer Coalition
Read:
Treatment of stage 4 ovarian cancer in Germany
Ovarian cancer – modern treatments
Leading 10 Gynecologic Oncologists in Germany: Who Are They?
Article menu:
- Understanding Stage 4 Ovarian Cancer
- Standard Treatments for Stage 4 Ovarian Cancer
- Advanced Stage 4 Ovarian Cancer Treatment Options
- Stage 4 Ovarian Cancer Treatment Stories: Regain Hope with Innovative Treatment Options
- Explore Your STage 4 Ovarian Cancer Treatment Options with Expert Support
- Frequently Asked Questions of Our Patients About Stage 4 Ovarian Cancer
Don't know where to start?
Contact Booking Health