In the last ten years, there have been significant advancements in the area of immunotherapy that offer cancer patients alternatives to traditional cancer therapies (in many cases, сhemotherapy, radiation, etc.) with their side effects. There is now substantial evidence demonstrating strong clinical benefits from intratumoral immunotherapy in cancer patients who receive this type of therapy as a second-line treatment or in the adjuvant setting (after initial surgical removal or radiation) [1-3]. These findings have sparked growing interest in utilizing cancer immunotherapies as neoadjuvants before local treatments to stimulate a long-term anti-tumor immune response by activating T-cells, recruiting dendritic cells, and reprogramming the tumor microenvironment [4].
Currently, intratumoral immunotherapy is one of the most promising new developments in oncology. Recent clinical trials show that more than 350 ongoing trials are examining intratumoral approaches to treat different types of cancers (including melanoma, prostate cancer, lung cancer, etc.), and more than 60% of these trials have shown objective regression of the tumor and systemic immune activation beyond the injection site.
Understanding Intratumoral Immunotherapy
For the past ten years, there has been a tremendous amount of excitement about the use of intratumoral immunotherapies in cancer treatment. Unlike systemic immunotherapy, which sends an immune agent throughout your body, localizing the delivery of the treatment to the tumor itself (intratumoral) enables a highly active and targeted stimulation of an anti-tumor immune response at the tumor site. This process is able to alter the environment within the tumor and stimulate the activity of dendritic cells, thereby providing a robust anti-tumor response.
What Is Intratumoral Immunotherapy?
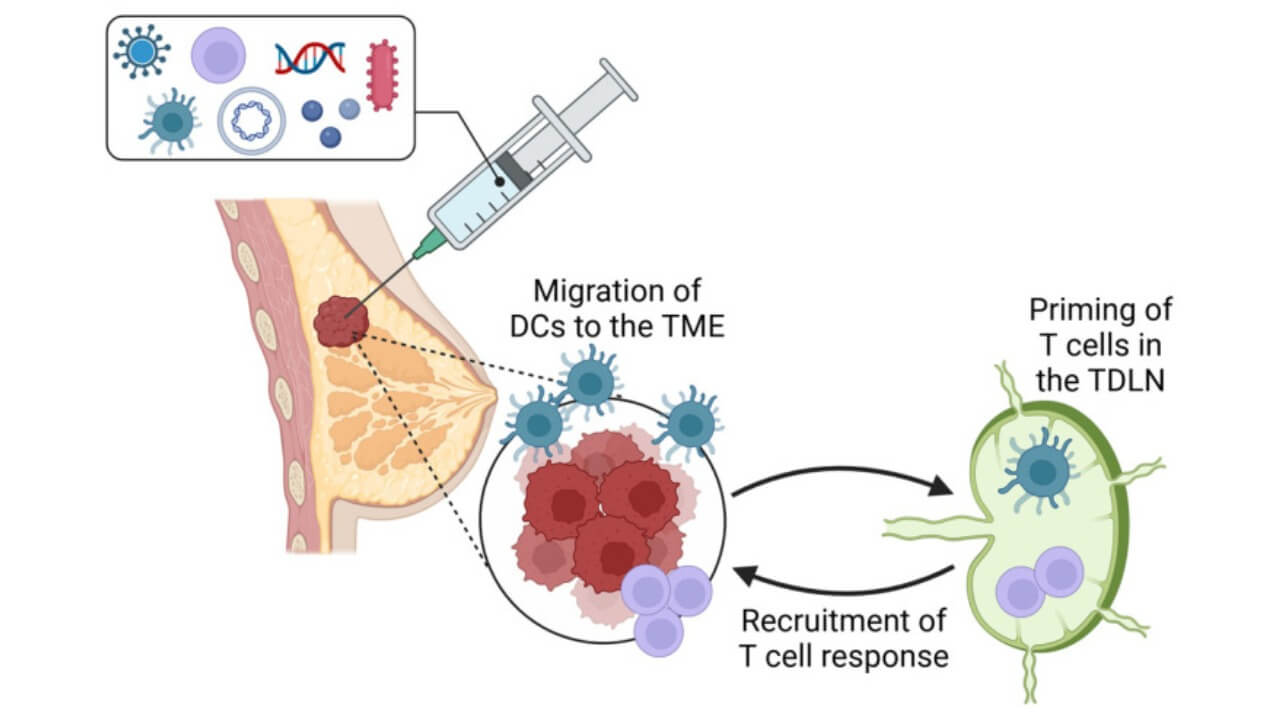
Intratumoral immunotherapy (ITI) is a form of treatment in which agents that augment and enhance the immune response are injected directly into cancer cells. Agents include cytokines, viral vectors, TLR (toll-like receptor) agonists, and newer gene-based substances such as interferon genes [5]. When administered into tumor tissue, these agents stimulate localized immune cells, particularly dendritic cells, to process tumor antigens and present them to T-lymphocytes. This leads to the activation of T-cell populations with resultant formation of an effective anti-tumor immune response, which has the capability of recognizing and destroying localized metastatic cancer cells in distant sites. Studies also show that intratumoral immunotherapy can convert the tumor itself into an effective "in situ vaccine". By stimulating the tumor microenvironment, the agents cause increased local inflammation, neutralization of immunosuppressive cells, and restoration of natural anti-cancer immunity. These considerations may account for the effectiveness of many intratumoral immunotherapy agents in patients diagnosed with advanced cancer who do not respond to standard manipulation.
Why Intratumoral Immunotherapy Is Gaining Global Relevance
Conventional chemotherapy and systemic immunotherapy are often ineffective due to toxicity, off-target effects, and inadequate concentration of the drug at the site of the tumor. In contrast, intratumor immunotherapy allows for the deposition of immune stimulatory agents directly at the locus of disease, which actually maximizes efficacy and minimizes systemic toxicity. Clinical trials in melanoma, prostate cancer, and lung cancer show not only tumor regression at the injected site but also regression of non-injected lesions. This is evidence of a clear systemic immune response. From present oncology databases, the number of immune trials for intratumoral immunotherapy has increased threefold since 2018. Initial results show tumor shrinkage in as much as 65% of those treated, with lasting effects for years in some instances. It is thus one of the most effective local cancer immunotherapy modalities in development today.
How Intratumoral and Systemic Immunotherapy Differ
Although systemic immunotherapy, such as checkpoint inhibitors (ICI) and CAR T-cell therapy, is delivered throughout the body, its efficacy is dependent on the presence of pre-existing immune infiltration within the tumor microenvironment. However, infiltration in many solid tumors is quite limited, leading to only moderate overall response rates. In contrast, intratumoral immunotherapy directly modifies the immune landscape of the tumor, transforming an otherwise "cold" tumor into a "hot" one that is recognized and attacked by immune cells. This synergy has driven the development of intratumoral immunotherapy in combination with systemic immunotherapies, checkpoint inhibitors, and CAR T-cell therapy. This approach results in pronounced local immune activation while simultaneously inducing a long-term systemic anti-tumor immune response. In this way, even patients with advanced disease have achieved measurable clinical improvement and prolonged survival.
Biological Rationale and Mechanisms
When the immune cells are present within a solid tumor but remain functionally suppressed, intratumoral therapy can help restore their normal immune activity. The delivery of immunomodulatory drugs directly into the tumor allows for the continuous interaction of these therapies between the cancer cells and their surrounding environment (tumor microenvironment). Unlike systemic immunotherapies, which may distribute throughout the body (with possible toxicities), intratumoral therapy has the advantage of providing very high concentrations of immune-modulating drugs inside the tumor. This targeted delivery of immunostimulatory drugs results in higher efficacy rates for local treatment, while simultaneously decreasing adverse effects commonly associated with systemic administration of immunotherapeutic agents.
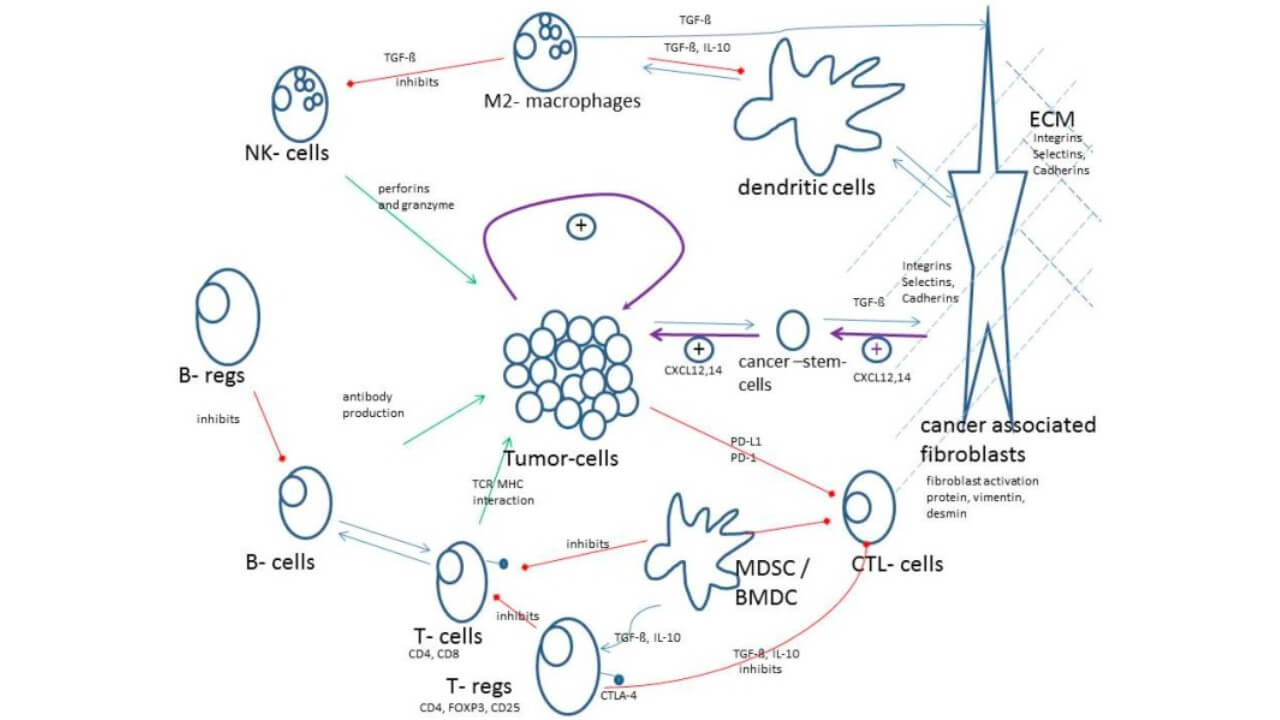
The tumor microenvironment (TME) consists of a variety of cell types, including immune cells, fibroblasts, vasculature, and various extracellular matrix (ECM) components. For many cancers, the primary role of the TME is to suppress the host's ability to recognize and destroy cancer cells through multiple mechanisms. When immunotherapeutic agents are delivered directly to the TME, they disrupt the immunosuppressive cells of this environment. As a result, dendritic cells are activated, inflammatory cytokines are produced, and the activity of the previously active inhibitors is eliminated.
Local Immune Activation and Reduced Toxicity
One of the main advantages of an intratumoral approach to immunotherapy is its potential to induce a localized immune response in proximity to the site of the disease (the tumor) as opposed to a systemic immune response, which may lead to destruction of normal tissue. This localized effect will increase the recruitment of cytotoxic T-lymphocytes and the T-cell activation within the tumor microenvironment. Activated T-cells can then disseminate systemically to other tumors and target all of them. A key clinical observation is that patients receiving intratumoral therapy experience less systemic toxicity than those treated with systemic therapy targeting the same pathway.
Remodeling the Tumor Microenvironment
In the context of solid tumor immunotherapy, modulation of the tumor microenvironment (TME) is of paramount importance. The substantial presence of immunoregulatory cells within solid tumors poses a major barrier to effective immunopotentiation [6]. One approach to overcoming this local immunoresistance is through local immunopotentiation: local macrophages from a tumor supporting phenotype transmute to a tumor-controlling one, then local dendritic cells achieve a more vigorous functional status, allowing enhanced vascular permeability for more extensive immune infiltration. This leads to a more effective anti-tumor action with improvement of response to adjunctive forms of therapy, such as CAR T-therapy or treatment via checkpoint inhibitors, etc.
In contrast to traditional systemic immunotherapy, in which immune modulators are distributed through the systemic circulation, local immunotherapy (LIT) allows precise immunogram control across all lesions. Such targeted biological modulation ensures minimal systemic exposure while maximizing the therapeutic potential within the local tumor microenvironment (TME). This approach not only achieves local tumor control but also promotes local immunopotentiation, transforming the tumor into a site of long-term immune stimulation and intervention.
Types of Intratumoral Immunotherapeutic Agents
Immunotherapies administered intratumorally are utilized in various forms to elicit an immune response at the level of the tumor by activating the immune system. Every therapeutic agent has different biological mechanisms, advantages, and disadvantages, enabling clinicians to develop tailored therapies based on the specific characteristics of the tumor, its size, as well as the local tumor microenvironment (TME).
Cytokines
Cytokines (small proteins) activate the immune system by sending signals to immune cells. Injected into cancer cells themselves, cytokines (like interleukins and interferons) can trigger T-cells and bring in dendritic cells to create a strong local and systemic immune reaction. Cytokines have advantages including an immediate induction of inflammation at the site and the capacity to modify the tumor microenvironment. Cytokine disadvantages include their very short half-lives and the possibility of causing irritation to local tissues.
Immune Adjuvants
Immune adjuvants help enhance the effects of many different types of intratumoral cancer immunotherapies. Adjuvants work either through their ability to stimulate pattern recognition receptors or as an activator of innate immunity. Therefore, they can enhance the function of dendritic cells and support the initial T-cell activation. The benefits of using adjuvants include the potential for synergistic effects when used in combination with other therapies and the capability to induce strong local immune responses against tumors. However, there is a possibility that the degree of immune response generated by the use of adjuvants could vary based on the pre-existing immune microenvironment of the tumor.
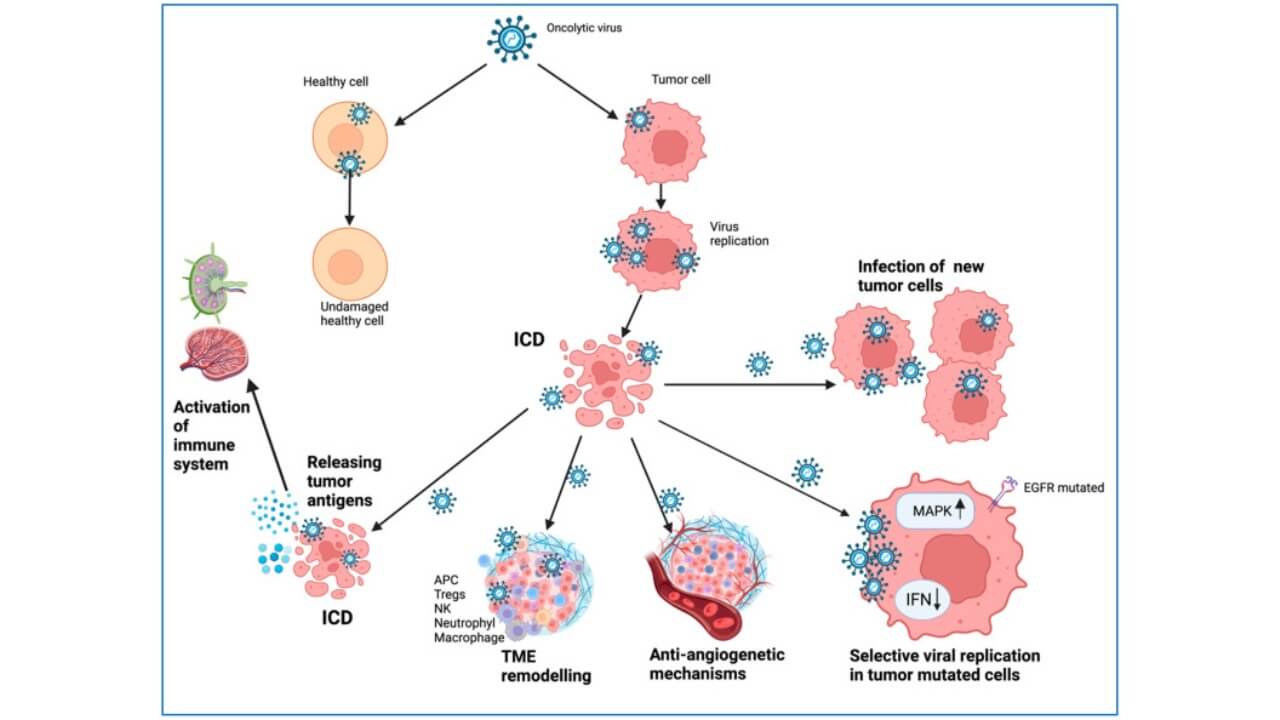
Oncolytic Viruses
Oncolytic viruses directly attack tumor cells, lysing them and liberating tumor antigens into the systemic circulation, thus producing an effective immune response to neoplasia. [7] The benefits of using oncolytic viruses include their activity in neoplastic lysis as well as their ability to provide immune priming and a potential for synergy with systemic immunotherapy. The drawbacks of therapy with oncolytic viruses include their neutralization effect by the host immune response, heterogeneous replication of the virus in the tumor microenvironment, and necessitating the administration of increasingly precise dosages in order to minimize secondary inflammation induced by the oncolytic virus.
Monoclonal Antibodies
Localized application of monoclonal antibodies can act on tumor-associated antigens, block immune checkpoints, or modulate the tumor microenvironment. Local delivery of monoclonal antibodies enables a selective therapeutic approach, resulting in higher local concentrations with reduced systemic exposure, thereby enhancing immune responses and minimizing toxicity. Advantages of local injection of monoclonal antibodies include specificity and concomitant use in the treatment regimen. Disadvantages would be poor penetration of monoclonal antibodies through dense tumors and potential adverse effects related to immunotherapy if they achieve systemic absorption.
Cell-Based Approaches
Intratumorally administered cellular therapies, including dendritic cells or engineered T-cells, can directly target cancer cells and induce strong activation of T-cells. Dendritic cells are recognized for their critical role in antigen presentation and initiation of an anti-tumor immune response, and were awarded the Nobel Prize in Physiology or Medicine for their important role in immune function. The local administration of these cells helps prime T-lymphocytes and induces systemic immune responses that are durable and capable of targeting both distant tumor burdens and the injected tumor lesions. The advantages include long-term memory against tumor cells, high specificity against tumor-derived antigens and the ability to remodel the tumor microenvironment (TME). The disadvantages or limitations include the difficulty of preparation, logistical issues that need to be overcome and variable infiltration according to the tumor type.
Delivery Methods and Technical Considerations
The success of intratumoral immunotherapy depends not only on the type of agent used but also on the accurate application of the agent. Accurate injection allows the therapeutic agent to have its maximum effect with minimum systemic exposure and toxicity. With the aid of current techniques, physicians can manipulate the deposition of the immunotherapeutic agent during its application into an appropriate area in the tumor microenvironment (TME)ーa great combination of efficiency, speed and safety.
Image-Guided Injection Techniques
A majority of tumors are treated intra-tumorally by means of local injections under image guidance with the aid of imaging modalities such as computer tomography (CT-Scan) or ultrasonography (US). These methods provide accurate localization of the needle into the tumor mass while at the same time avoiding important neighboring structures and ensuring even distribution of the drug. Imaging guidance is especially needed in the case of tumors that are deep-seated and of irregular contour, where blind injection may result in poor anti-tumor immune response and leakage into the neighboring tissues.
Distribution Within the Tumor
Once within the tumor, therapeutic agents must diffuse efficiently within the lesion to stimulate local dendritic cells, activate T-cells, and remodel the local tumor environment. The chemical and physical properties of the agent, injection volume, and needle design all contribute to intratumoral diffusion. Multi-needle systems or slow infusion techniques may improve coverage while reducing reflux along the needle track and leakage into surrounding healthy tissue.
Needle Design and Injection Volume
Choosing the right needle and the correct amount of liquid (volume) for injections is very important in order to achieve accurate and precise delivery. Using fine-gauge needles results in less tissue damage and less leakage. Using large amounts of liquid increases local pressure which could result in greater dispersion of the material into the surrounding tissues, but also raises the risk of extravasation. Clinical experience has shown that by altering the gauge of the needle, the bevel (the flat side of the needle), and the rate at which you inject, you can maximize your ability to deposit the material locally (thus maximizing your local immune response and subsequently your overall systemic effect).
Risk Management and Safety Considerations
Although thorough planning is in place, there will always be an element of potential leakage or non-uniform distribution that could impact the treatment's effectiveness. To minimize complications (such as those from the injection process), it is recommended to continuously image the delivery process of the drug during (using slow infusion rates) and closely monitor the patient's reaction to the procedure. Using technology (to ensure precise delivery of the drug), combined with the biologic reasoning behind using drugs delivered directly into tumors (intratumoral therapy), provides clinicians the opportunity to maximize the local immune response against tumors, while also providing safety for their patients suffering from metastasis or advanced cancer.
| Feature | Intratumoral Immunotherapy | Systemic Immunotherapy |
|---|---|---|
| Delivery site | Directly into tumor cells, often under imaging guidance | Systemic circulation (intravenous) |
| Immune effect | Local immune activation, stimulation of dendritic cells, generation of an anti-tumor immune response | Systemic activation, dependent on pre-existing T-cell infiltration in the tumor microenvironment |
| Systemic toxicity | Minimal (reduced systemic toxicity) | Higher, risk of immune-related adverse events |
| Effect on metastases | Can induce systemic immunity from local injection | Acts on distant lesions but may be less effective in "cold" tumors |
| Injection technique | Intratumoral injection technique (CT/US guidance, precise distribution) | Infusion or injection, no direct tumor targeting |
| Indications | Local tumors, patients with advanced or resistant disease | Widespread cancers, often combined with other treatments |
| Advantages | High local concentration, minimal side effects, durable anti-tumor immune response | Can target distant metastases, accessible to a broad range of patients |
| Limitations | Requires precise delivery, specialized equipment, trained personnel | Less effective in "cold" tumors, risk of systemic toxicity |
How Intratumoral Immunotherapy Gave Mark a Second Chance
Mark, a 58-year-old Ukrainian man, had been diagnosed with advanced prostate cancer that had metastasized to the regional lymph nodes. After a short period of some benefit from conventional treatment and systemic immunotherapy, his oncologist recommended intratumoral immunotherapy in Germany.
Mark used the services of Booking Health, which helps facilitate consultations, medical travel, and hospital admissions, and in his case, to arrange CT-guided intratumoral immunotherapy injected directly into the tumor cells. This treatment produced immediate results, including activation of local dendritic cells, alteration of the tumor microenvironment, and induction of a systemic anti-tumor immune response. Imaging showed regression in the size of the tumor lesions within a few weeks, and the lesions at distant sites also responded to the treatment, with evidence of T-cell activation. Because of the local mode of immunotherapy administration, Mark experienced fewer side effects than he had with previous systemic immunotherapy.
Over the following months, his general health improved, enabling him to maintain a highly active daily life. His case highlights the significant benefits of intratumoral immunotherapy in Germany, which can be effectively facilitated by the expert support of Booking Health and provides patients with clinical improvements, particularly in advanced or metastatic disease that is poorly responsive to conventional treatments.
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods and with leading specialists in this field.
Modern Cancer Treatment: Patient Journeys with Booking Health
FAQ: Intratumoral Immunotherapy
Send request for treatmentIntratumoral immunotherapy involves injecting immune-activating agents directly into the tumor. This stimulates a local immune response, helping the body recognize and attack cancer cells more effectively.
Intratumoral immunotherapy can be used to treat various cancers, including melanoma, breast cancer and head and neck cancers. It is particularly effective for tumors that are accessible for direct injection.
Benefits include a localized treatment approach, reduced systemic side effects and the potential for a strong and sustained immune response against the cancer. This therapy can improve overall outcomes and quality of life.
Effectiveness is monitored through regular imaging tests and clinical evaluations. These assessments help doctors determine the therapy's impact and make any necessary adjustments.
Most side effects are localized and mild, such as pain at the injection site and inflammation. Severe side effects are rare but can occur necessitating close monitoring during treatment to manage any adverse reactions promptly.
Immunotherapy can be used for early, advanced, or metastatic cancers depending on tumor type and patient condition. Its application often complements surgery, radiation, or chemotherapy to enhance systemic immunity from local injection.
Life expectancy varies by cancer type, stage and treatment response. Some patients achieve long-term remission, while others experience disease stabilization, highlighting the importance of personalized planning and monitoring through expert consultation.
Cancers with high immunogenicity, such as melanoma, lung, bladder and kidney cancers, often respond best to immunotherapy due to their ability to stimulate strong systemic immunity from local injection and durable anti-tumor effects.
Recent advances include engineered cellular therapies and novel immune modulators delivered via direct intratumoral injection technique offering localized activation of immune cells and systemic anti-cancer benefits.
Intratumoral immunotherapy definition: it delivers treatment directly into the tumor, providing higher local concentration and targeted immune activation, unlike systemic therapies that circulate through the whole body.
Various types of intratumoral agents are used, including cytokines, viral vectors, immune adjuvants, monoclonal antibodies, and cell-based therapies, each designed to stimulate the local immune response effectively.
Key benefits include precise tumor targeting, reduced systemic toxicity, and the ability to transform the tumor into an in situ vaccine, generating both local and systemic anti-tumor responses.
Patients can seek guidance through oncologists, specialized clinics, or an international coordinator Booking Health to receive expert consultation for personalized treatment plans and access to cutting-edge clinical trials.
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Alexander M M Eggermont, Christian U Blank, Mario Mandala et al. Adjuvant Pembrolizumab versus Placebo in Resected Stage III Melanoma. N Engl J Med. 2018 May 10;378(19):1789-1801. doi: 10.1056/NEJMoa1802357. Epub 2018 Apr 15. [DOI] [PubMed]
[2] Eliezer M Van Allen, Diana Miao, Bastian Schilling et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science. 2015 Oct 9;350(6257):207-211. doi: 10.1126/science.aad0095. Epub 2015 Sep 10. [DOI] [PubMed]
[3] Alexander M M Eggermont, Vanna Chiarion-Sileni, Jean-Jacques Grob et al. Prolonged Survival in Stage III Melanoma with Ipilimumab Adjuvant Therapy. N Engl J Med. 2016 Nov 10;375(19):1845-1855. doi: 10.1056/NEJMoa1611299. Epub 2016 Oct 7. [DOI] [PubMed]
[4] Jake S O'Donnell, Esmée P Hoefsmit, Mark J Smyth, Christian U Blank, Michele W L Teng. The Promise of Neoadjuvant Immunotherapy and Surgery for Cancer Treatment. Clin Cancer Res. 2019 Oct 1;25(19):5743-5751. doi: 10.1158/1078-0432.CCR-18-2641. Epub 2019 Apr 30. [DOI] [PubMed]
[5] Camille C Baumrucker, Nicole Harris, Susan Hoover, Brian J Czerniecki. Intratumoral Immunotherapy in Breast Cancer. Vaccines (Basel). 2025 Apr 19;13(4):429. doi: 10.3390/vaccines13040429. [DOI] [PMC free article]
[6] Borros Arneth. Tumor Microenvironment. Medicina (Kaunas). 2019 Dec 30;56(1):15. doi: 10.3390/medicina56010015. [DOI] [PMC free article]
[7] Simona Ruxandra Volovat, Dragos Viorel Scripcariu, Ingrid Andrada Vasilache et al. Oncolytic Virotherapy: A New Paradigm in Cancer Immunotherapy. Int J Mol Sci. 2024 Jan 18;25(2):1180. doi: 10.3390/ijms25021180. [DOI] [PMC free article]
Read:
New Effective Treatments for Stage 4 Cancer (oncology)
Article menu:
- Understanding Intratumoral Immunotherapy
- Biological Rationale and Mechanisms
- Types of Intratumoral Immunotherapeutic Agents
- Delivery Methods and Technical Considerations
- How Intratumoral Immunotherapy Gave Mark a Second Chance
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ: Intratumoral Immunotherapy
Don't know where to start?
Contact Booking Health















