Anal carcinoma is a rare but increasingly common, malignant neoplasm: the incidence has increased by approximately 2.7% per year over the past decade. Squamous cell carcinoma (SCC) accounts for approximately 85% of all cases. Although anal carcinoma is relatively rare compared with other malignancies, it has a notable prevalence, especially among individuals with certain risk factors. The HPV vaccine is one of the most effective means of preventing HPV-associated anal cancer and reduces the risk of infection with oncogenic types of the virus. The HPV vaccine is recommended for both adolescents and adults from high-risk groups, as the HPV vaccine helps reduce the incidence in the long term. Accurate diagnosis and effective treatment require a detailed understanding of the anatomy of the anal canal and lymphatic drainage. Early detection is key to improving prognosis, and although a comprehensive clinical examination and imaging techniques play an important role [1].
What is anal carcinoma?
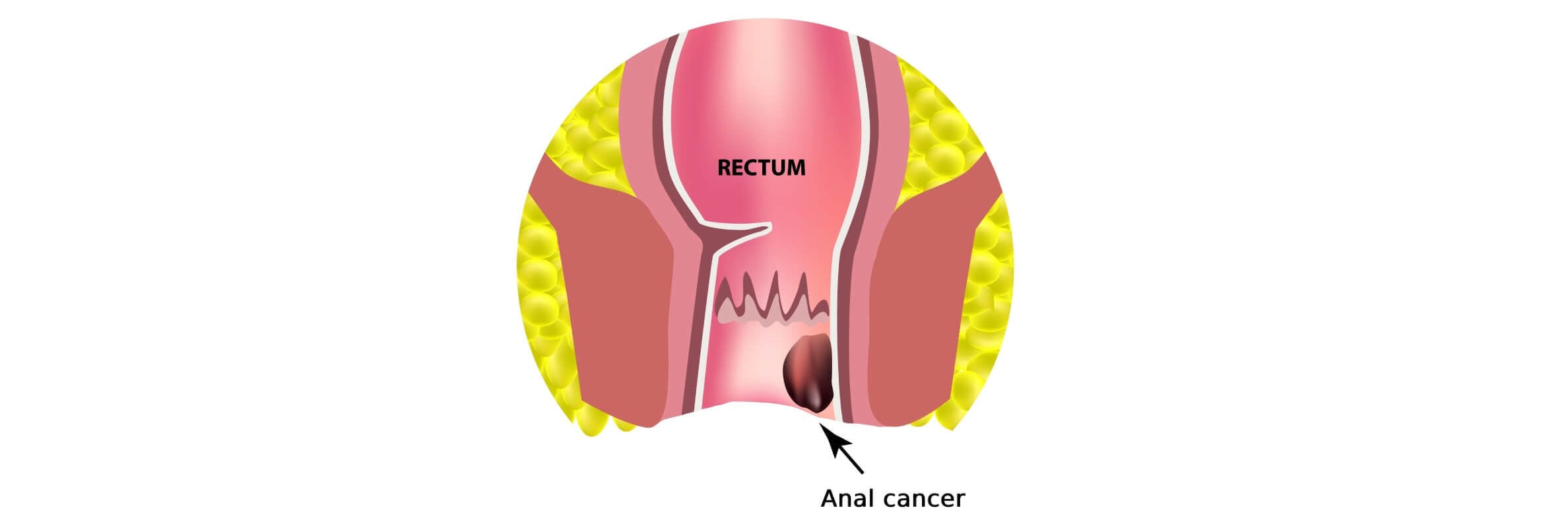
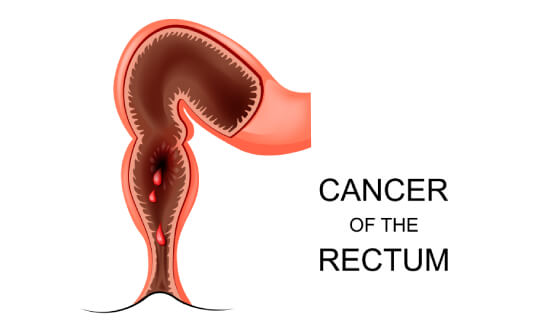
Anal cancer develops from the epithelium of the anal canal or perianal area, most often represented by squamous cell carcinoma, and is biologically and clinically different from colorectal cancer. The disease has its own risk factors. In most cases cancer cells are associated with high oncogenic risk human papillomavirus (HPV infection), and characterized by specific routes of lymphogenic spread and require a separate approach to diagnosis, staging and treatment, the basis of which, according to international treatment protocols, are chemotherapy and radiation therapy with organ-preserving goals.
According to the definition of the International Union for Cancer Control (UICC), the surgical anal canal is 3-4 cm long and extends from the upper edge of the internal anal sphincter (levator anorectalis) to the anal verge [2].
The incidence of anal intraepithelial neoplasia increases with age, with a median age of diagnosis of 62 years. Although the disease is rare in individuals younger than 35 years, the incidence rate among younger adults is increasing. The highest prevalence is observed in women aged 75-79 years and in men aged 80-84 years. Age is also a key factor in the progression to high-grade anal intraepithelial neoplasia, especially in HIV-positive and HIV-negative men. This trend is largely due to the long latency period of human papillomavirus-associated cancer cells carcinogenesis ( when normal cells are transformed into cancer cells) [3].
Types of malignancies associated with anal cancer include:
- Squamous cell carcinoma (SCC). The most common type of malignancy of the anal canal (about 85% of cases).
- Verrucous carcinoma. Known as Buschke–Löwenstein tumor, this is a locally aggressive lesion that morphologically resembles condyloma but has destructive potential and high risk factors.
- Adenocarcinoma. Originates from the mucosa or anal canal glands; may be associated with Paget's disease or Crohn's disease.
- Melanoma. Rare and highly aggressive tumor; anal melanomas are morphologically similar to cutaneous melanomas but have a poor prognosis.
- Neuroendocrine tumors. Represent about 1% of all anal canal malignancies.
Symptoms of anal carcinoma
Anal carcinoma most often presents with rectal or anal bleeding (anal squamous intraepithelial lesions) – in almost 50% of cases, followed by anal pain and the presence of a palpable mass. Additional symptoms include pruritus, anal pain, tenesmus, mucopurulent discharge, change in stool caliber, and incontinence. In some patients, clinical manifestations may mimic benign anorectal conditions such as anal fissures or fistulas, while others remain asymptomatic until the disease reaches a late stage [1].
Duration of symptoms generally does not correlate with prognosis, except for symptoms lasting less than 1 month, which is associated with better treatment outcomes. The type of initial symptoms is more closely related to the T stage of the tumor than to their duration.
The location of the lesion should be precisely defined, differentiating between the following:
- Cutaneous lesions – located more than 5 cm from the anal verge and visible without traction.
- Perianal lesions – located within 5 cm of the anus and fully visualized with gentle traction.
- Anal canal lesions – partially or completely invisible even with traction and requiring digital rectal exam for detection [4].
Diagnostic methods of anal cancer
The first diagnostic steps according to current European and American guidelines are digital rectal exam with anal canal examination and, if necessary, vaginal examination, rectoscopy, and palpation of the inguinal lymph nodes. Besides, anal cancer screening is performed in high-risk groups and is aimed at early detection of precancerous changes and tumors.
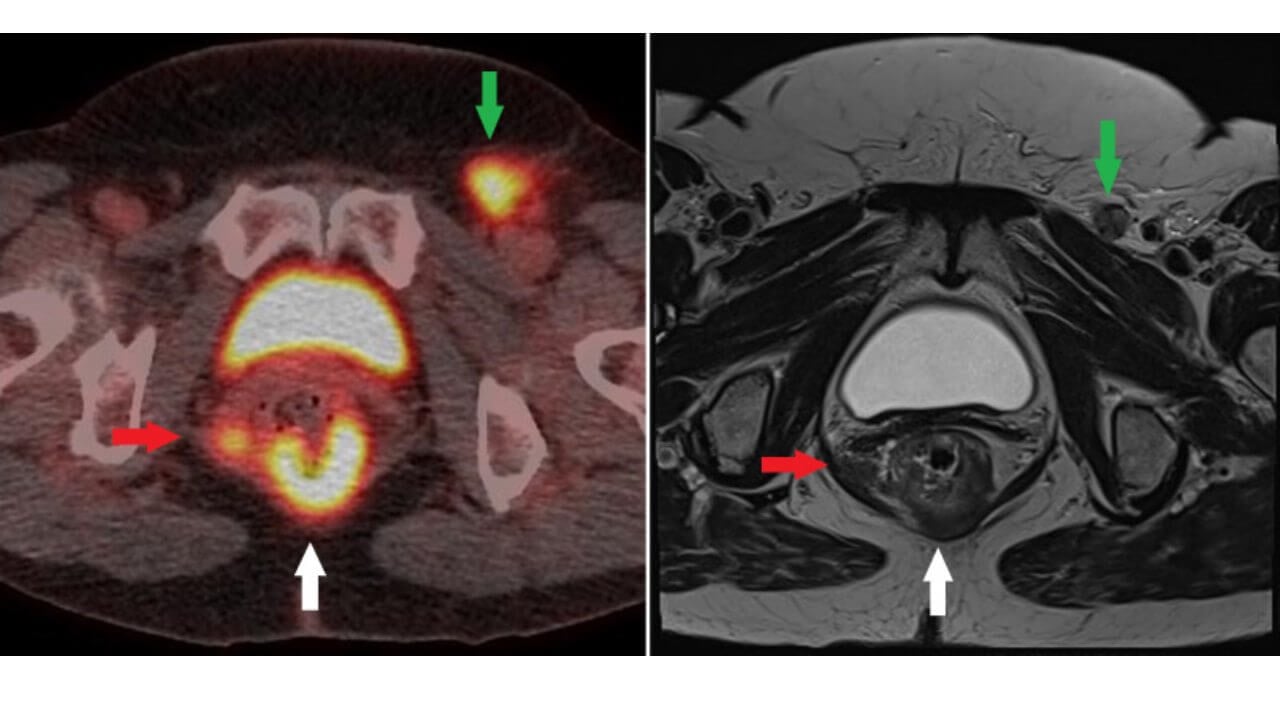
The NCCN [5] recommends palpation of the inguinal lymph nodes with fine-needle aspiration (FNA) and/or excisional biopsy of nodes that are suspicious on clinical or radiological grounds. Evaluation of the pelvic lymph nodes by CT or MRI of the pelvis is also recommended. Fluorodeoxyglucose positron emission tomography (FDG-PET/CT) is highly sensitive in detecting involved lymph nodes. However, PET/CT is not currently part of routine staging. According to current NCCN guidelines, PET/CT is indicated for confirmation of staging in T2–4, N0, and in any T, N+ anal carcinoma [1].
The following laboratory tests are recommended in the evaluation of patients with anal cancer:
- HIV testing, as anal cancer is closely associated with HPV infection and is more common in patients with HIV infection.
- Complete blood count (CBC) to assess for anemia or other hematologic abnormalities.
- Liver function tests to assess for liver metastases.
- High-risk HPV subtypes (HPV-16, HPV-18) are implicated in the majority of cases of anal squamous cell carcinoma. Measurement of the p16 protein (a surrogate marker for HPV infection-associated cancer) may provide prognostic information [1].
Stages of anal cancer
The TNM staging system for anal cancer, developed by the American Joint Committee on Cancer (AJCC), is described in detail in the relevant guidelines. The prognosis for anal carcinoma depends on the size of the primary tumor and the presence of lymph node metastases.
Staging of anal cancer is based on the TNM system (AJCC) and takes into account:
- Size and extent of the primary tumor (T).
- Involvement of regional lymph nodes (N).
- Presence of distant metastases (M).
Stage I – localized cancer (early stage)
T1N0M0
Tumor ≤2 cm, limited to the anal canal or perianal area. Lymph nodes are not involved, there are no distant metastases. Often has minimal symptoms or is discovered incidentally. It is possible to prevent anal cancer on this stage.
Stage II – localized but larger cancer
IIA: T2N0M0 (tumor >2 cm but ≤5 cm)
IIB: T3N0M0 (tumor >5 cm)
Lymph nodes are not involved. The disease remains localized, but the risk of recurrence is higher.
Stage III – locally advanced cancer
IIIA–IIIC
A tumor of any size with involvement of regional lymph nodes (inguinal, pelvic, mesorectal), or invasion of adjacent structures (sphincter, vagina, urethra, bladder). This is locally advanced disease. Lymph nodes are a key negative prognostic factor.
Stage IV – metastatic cancer
Any T, any N, M1. Distant metastases are present (most often liver, lungs, distant lymph nodes). The disease is systemic [5].
Thus, localized anal cancer is confined to the anal canal or perianal area without involvement of lymph nodes or distant organs and has the opportunity to prevent anal cancer in some cases. Locally advanced cancer is characterized by involvement of regional lymph nodes or invasion of adjacent structures, which reduces the prognosis but still allows for radical treatment. Metastatic anal cancer is accompanied by distant metastases and requires mainly systemic therapy with palliative or control goals.
Treatment options for anal cancer
Standard treatment for anal cancer
Historically, treatment of most anal cancers has involved surgical resection by abdominoperineal resection, which has a cure rate of approximately 50%, but is associated with significant morbidity and functional loss. Today, the standard of care for localized anal cancer is a combination of chemotherapy and radiation therapy, which provides better results with less morbidity [6]. Radiation therapy for anal cancer is a key component of standard treatment, as it allows for high local tumor control with the possibility of preserving the anal sphincter. Results from randomized clinical trials evaluating the efficacy and safety of combining chemotherapy with radiotherapy support the use of combination therapy in the treatment of anal carcinoma. Immunotherapy for anal carcinoma is used mainly for advanced or recurrent forms of the disease and is aimed at activating the immune response against the tumor, in particular with the help of checkpoint inhibitors.
According to current American and European guidelines, primary surgical treatment by colon and rectal surgeons with a radical goal is currently indicated only for highly differentiated T1, N0 anal margin carcinomas. Surgery for anal carcinoma (abdominoperineal resection) is required as a salvage procedure in approximately 10–30% of cases, and is performed due to local recurrence in approximately 19% of patients [7].
Most patients with stage II–III anal cancer experience treatment interruptions, especially long ones (>42 days), associated with worse progression-free survival (PFS) and overall survival (OS). Stage 4 anal carcinoma treatment involves primarily systemic therapy to control the disease, relieve symptoms, and prolong life, with the possible use of local methods in selected clinical situations. Interruptions are often due to chemoRT toxicity; acute complications (anoproctitis, perineal dermatitis) increase with increasing doses and shorter durations of radiation. Registry data suggest higher risk factors such as pelvic fractures in women ≥65 years of age after RT [5].
Modern treatment for anal carcinoma is based on chemoradiation therapy as the standard, with individual selection of innovative methods in case of advanced or recurrent disease.
Dendritic cells therapy for anal cancer
In 2011, Ralph Steinman, an American immunologist, received the Nobel Prize in Physiology or Medicine for his fundamental discovery [8]. Given that most anal cancers, including anal squamous cell carcinoma, are HPV infection-associated tumors, immunotherapeutic approaches are being actively investigated as potential treatment strategies. Dendritic cell therapy (DC therapy) is based on the use of dendritic cells modified to present cancer cells or viral antigens in order to activate a specific T-cell antitumor immune response. The idea of DC vaccines is to "teach" the weakened immune system to recognize tumor/human papillomavirus antigens (often E6/E7 of HPV16) through antigen presentation by dendritic cells, i.e. to create an activated T-cell response.
In this context, the practical experience of dendritic cell clinics is of considerable interest, both in terms of mechanisms of action and clinical limitations, indications and potential combinations with standard treatments. In the video below, Professor Gansauge, head of the dendritic cell therapy clinic, explains in detail the principles of dendritic cells, their application in oncology, clinical results, limitations of the method and prospects for the development of this area. The interview allows us to better understand what place dendritic cell therapy can take in future combination approaches to the treatment of anal carcinoma, and why it remains today a field of clinical research and individualized solutions.
The advantage of dendritic cell therapy is its high specificity, which allows to minimize the systemic toxicity characteristic of traditional chemotherapy and potentially provide long-term immune system control of the cancer cells. This is especially relevant for patients with recurrent anal cancer, in whom standard treatment options are limited.
Dendritic cell therapy for anal cancer is considered an innovative immunotherapeutic approach that can potentially enhance the antitumor immune response, especially in relapsed or refractory disease. In addition, dendritic cell therapy is considered as an adjunct to existing methods, not a replacement for them. It can potentially enhance the effectiveness of chemoradiotherapy or immunotherapy with checkpoint inhibitors, forming a more persistent antitumor immune system response. It is this possibility of integration into combination therapeutic strategies that makes dendritic cell therapy the subject of active clinical research.
Regional chemotherapy with isolated pelvic perfusion for anal cancer
In addition to standard systemic and locoregional approaches, regional chemotherapy methods are also being investigated in the treatment of anal carcinoma, aimed at increasing local antitumor efficacy while minimizing systemic toxicity. One such approach is regional chemotherapy with isolated pelvic perfusion, which involves temporary isolation of the pelvic circulation with subsequent administration of high concentrations of cytostatic drugs without their significant entry into the systemic bloodstream. Intra-arterial chemotherapy is a locoregional treatment method that allows chemotherapy drugs to be administered directly into the vessels that feed the tumor, providing high local efficacy with minimal systemic toxicity.
Isolated hypoxic pelvic perfusion increases the sensitivity of some chemotherapeutic agents. In addition, limiting the exposure of chemotherapy drugs to the pelvic area reduces systemic toxicity and, consequently, systemic side effects. Early clinical data indicate that hypoxic pelvic perfusion can provide high local response rates. At the same time, the use of hypoxic pelvic perfusion alone is limited by the difficulty of achieving complete coverage of the tumor volume [9].
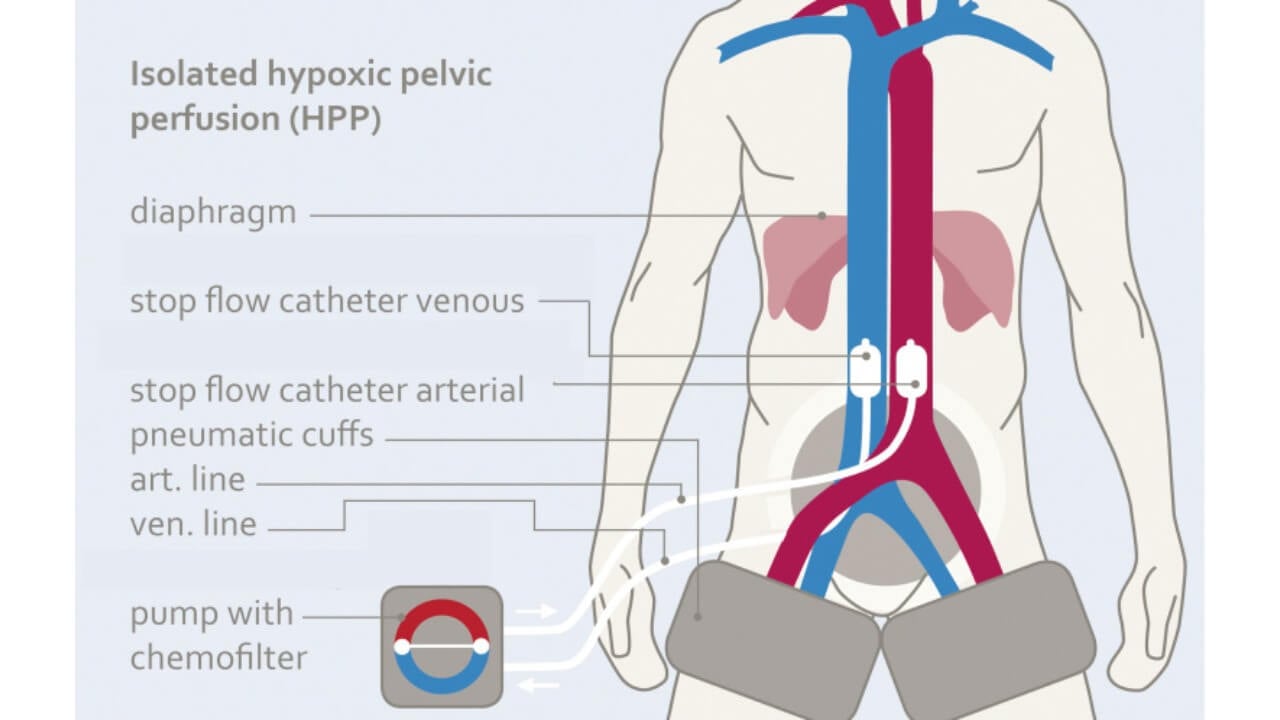
Chemotherapy is administered by rhythmic pulsating injections through the large perfusion channel of the aortic balloon catheter at intervals of 1–1.5 minutes in order to achieve high drug concentrations during the first pass. Immediately after this, both balloons are blocked with a diluted contrast medium. The five-minute so-called stop-flow phase creates a pronounced first-pass effect and, accordingly, a high uptake of cytostatics by the tumor tissue due to the high initial oxygenation. Isolated hypoxic perfusion is maintained for 15 minutes; the stop-flow phase is included in the total duration of isolated hypoxic perfusion.
Electrochemotherapy for anal cancer
Electrochemotherapy (ECT) is a local oncology treatment that combines the administration of a chemotherapeutic drug with short electrical pulses that temporarily increase the permeability of tumor cell membranes (electroporation).
Electroporation increases the permeability of cell membranes, thereby enhancing the efficacy of chemotherapy. Several clinical studies have shown that electroporation can improve local response, but its effectiveness is often limited by tumor depth and the difficulty of treating large or deeply located tumors. The combination of hypoxic pelvic perfusion and electroporation overcomes the limitations of either approach alone [10].
When combining isolated perfusion with reversible electroporation, three to four electrodes are initially placed near the tumor margins under direct visual control in the lithotomy position and connected to a pulse generator for adaptive electroporation.
After this, the patient is placed in a standard supine position, the inguinal area is disinfected, the femoral arteries and veins are cannulated. Chemotherapeutic drugs are administered during the delivery of electrical impulses.
This is demonstrated by studies in which there are both primary patients with anal cancer and patients with recurrence after radiochemotherapy. In two previously untreated patients, three and two procedures of isolated perfusion therapy were performed, respectively; in cases of relapse after radiochemotherapy, repeated intra-arterial infusion was insufficient due to the low local exposure of the cytostatic. Only isolated pelvic perfusion combined with electroporation achieved complete histological remission, which is explained by the increased drug uptake through the temporarily porous membranes of tumor cells due to the action of electrical pulses. The table below summarizes the key characteristics of standard and novel treatment strategies, including mechanism of action, indications, efficacy, toxicity profile, and clinical status of use. Such a comparison allows us to assess the potential advantages and limitations of innovative methods, as well as to determine their possible role in future combination treatment regimens.
| Treatment Type | Toxicity and side effects | Quality of life | Duration |
|---|---|---|---|
| Surgery | low; risk factors such as infections, pelvic organ dysfunction, formation of permanent colostomy | significantly reduced | one-time intervention, but with a long rehabilitation |
| Chemotherapy | high; hematologic, gastrointestinal side effects, nephro- and neurotoxicity | often temporarily impaired due to systemic side effects and the need for multiple courses | several months, repeated cycles with breaks |
| Radiation therapy | significant; acute dermatitis, proctitis, cytopenias and late fibrosis, stenoses, sexual dysfunction | may be significantly reduced during treatment and in the long term, despite organ preservation | usually 5-7 weeks of daily treatment; interruptions due to toxicity are possible |
| Dendritic cells therapy | low; usually limited to mild local or flu-like reactions | preserved; lack of significant systemic toxicity allows maintenance of usual level of activity | lifelong anticancer immunity after the single injection |
| Regional chemotherapy | low; limited to local exposure | better preserved due to high local efficacy and low systemic toxicity | usually several sessions with rapid recovery |
| Electrochemo-therapy | low-moderate; local pain or swelling | good, local treatment avoids systemic side effects | short procedure (several sessions) |
Innovative methods for anal cancer treatment in Germany
Treatment of most anal cancers in Germany today is based on the principles of organ preservation, personalized medicine and minimizing toxicity, which significantly distinguishes the German approach from the more aggressive or standardized models still used in many countries. The country's leading oncology centers are actively implementing minimally invasive and regional treatment methods, which allows achieving high local tumor control with a significantly better quality of life for patients.
Anal cancer treatment abroad is often chosen by patients seeking access to modern minimally invasive methods, a multidisciplinary approach, and high treatment effectiveness with optimal therapy timing. The standard anal cancer treatment in most countries of the world, in particular in the USA and Eastern Europe, remains chemoradiotherapy according to classical protocols. Although this approach is effective from an oncological point of view, it is often accompanied by significant acute and late toxicity, a long treatment period (5–7 weeks) and a pronounced impact on the physical and psychoemotional well-being of the patient.
Germany, unlike many other countries, emphasizes reducing the systemic load and localizing the therapeutic effect. In addition to modern chemoradiotherapy regimens, innovative methods are actively used here, such as regional chemotherapy (isolated pelvic or hypoxic perfusion), electrochemotherapy in selected clinical situations, as well as immunotherapeutic approaches, in particular dendritic cell therapy. Medical treatment in Germany for anal cancer includes modern, evidence-based approaches combining chemoradiotherapy as the standard, with an emphasis on organ preservation, as well as access to innovative methods, multidisciplinary management, and individualized therapy selection in the country's leading oncology centers.
For patients with anal carcinoma, the choice of country of treatment often depends not only on the availability of modern methods and clinical outcomes, but also on the financial burden. The cost of oncological care varies significantly between countries, depending on the structure of the health care system, the role of insurance coverage, the duration of treatment and the use of innovative technologies.
The table below compares the estimated cost of anal cancer treatment in the United States, Germany, Australia and the United Kingdom. This allows for a better assessment of the ratio of cost, effectiveness and accessibility of treatment in an international context.
| Treatment type | Cost Germany | Cost USA | Cost GB | Cost Australia |
|---|---|---|---|---|
| Surgery | €25,000 - €45,000 | €65,000 - €85,000 | €35,000 - €55,000 | €30,000 - €70,000 |
| Chemotherapy | €80,000 - €150,000 full course | €100,000 - €180,000 full course | €90,000 - €165,000 full course | €45,000 - €120,000 |
| Radiotherapy | €28,000 - €42,000 | €40,000 - €80,000 | €35,000 - €65,000 | €25,000 - €50,000 |
| DC therapy | €20,000 - €38,000 | €40,000 - €100,000 | not available | not available |
| Regional chemotherapy | €18,000 - €75,000 per session | €37,000 - €150,000 | €30,000 - €118,000 | €30,000 - €80,000 |
| Electrochemo-therapy | €6,500 - €24,000 per session | €40,000 - €100,000 | €25,000 - €45,000 | not available |
History of a patient with anal carcinoma
Alex has a complex oncological history. He was diagnosed with squamous cell carcinoma of the anal canal, initially a locally advanced form with a high degree of malignancy. After a standard course of chemoradiotherapy, only a partial response was achieved, and later a local tumor recurrence was recorded, which was accompanied by pain syndrome and a significant decrease in the quality of life. Repeated systemic therapy was limited due to pronounced toxicity and the risk factors.
Given the clinical situation, the patient was offered an innovative organ-sparing approach – regional chemotherapy in the form of isolated hypoxic pelvic perfusion in combination with electrochemotherapy. The goal of treatment was to achieve a high local concentration of cytostatics in the tumor tissue with minimizing systemic toxicity.
Despite the difficult initial prognosis received before the start of regional therapy, the patient maintains a good functional status, has returned to daily activities and does not require constant pain relief. Systemic side effects were minimal, which allowed avoiding long-term hospitalizations and maintaining a decent quality of life.
The patient's family expresses full confidence in the chosen treatment strategy and team of specialists, emphasizing the positive dynamics:
"From the first day we felt that this is not just a hospital. It is calm, bright and humane here. Thanks to the professionalism of the entire team, our dad got a chance that, according to previous forecasts, was almost nonexistent. Today he lives without constant pain, moves, plans for the future – and this is the most important thing for us. We sincerely believe in this treatment program and are grateful for every step we have taken together".
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex cancer management programs in each case. As a reputable company, Booking Health offers personalized anal carcinoma with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets.
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you on the way of pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for anal carcinoma with leading specialists in this field.
Modern Cancer Treatment: Patient Journeys with Booking Health
Frequently Asked Questions About Anal Cancer
Send request for treatmentThe most common anal cancer symptoms are rectal/anal bleeding, pain in the anus, a feeling of a "tightness" or nodule, itching, mucopurulent discharge, tenesmus, change in stool caliber, and impaired bowel control. As early signs of anal carcinoma are often disguised as "hemorrhoids" or fissures, symptoms require examination and verification.
The main treatment options include: chemoradiotherapy (standard in most non-metastatic cases), regional chemotherapy, electrochemotherapy, surgery (mainly for persistence/recurrence or some early perianal forms), systemic therapy for metastases (chemotherapy ± immunotherapy), and dendritic cell vaccination.
In non-metastatic squamous cell carcinoma of the anal canal, the most effective and standard best treatment for anal cancer is concurrent chemoradiotherapy; chemoradiotherapy effectiveness has been proven to provide high local control with the chance of avoiding difficult surgery.
Anal cancer diagnosis is based on: clinical examination + digital rectal examination, anoscopy/proctoscopy and mandatory biopsy for histological confirmation; then imaging (CT/MRI of the pelvis, often PET-CT) for staging.
Treatment cost or price of cancer treatment abroad varies greatly depending on the country, insurance coverage, duration of treatment (e.g., 5–7 weeks of RT/CRT), need for hospitalization and complications. For international patients, diagnostics, course of therapy and post-treatment monitoring are usually counted separately. For example, chemotherapy abroad costs from 45,000 to 180,000 euros.
Cost in Germany depends on protocol. In open sources, there are examples of the cost of combined programs (chemo+RT) at the level of €100,000-€150,000; however specifically for anal carcinoma, the amount is formed individually (stage, IMRT, hospitalization, support). This is the practical meaning of the key anal cancer treatment cost Germany.
The key benchmarks in this question are stage 4 anal cancer prognosis, life expectancy and survival statistics. According to population data, the 50-year relative survival for "distant" (metastatic) anal carcinoma is about 36% (depending on population).
In general anal carcinoma treatment in Germany is based on the evidence standards as in leading US/UE centers, but unlike other countries, anal cancer treatment Germany is successful, because it can include innovative methods.
For stage 3 advanced anal cancer treatment usually means radical chemoradiation with modern radiation techniques; for stage 4 anal carcinoma therapy – mainly systemic treatment and local methods are used to control symptoms.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Daria Sukhoruchenko. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Vicente Ramos Santillan, Anahat Kaur, Gopal Menon, Hani M. Babiker, Burt Cagir. Anal Carcinoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. 2025 Apr 12. [PubMed]
[2] Dimitrios Raptis, Ignaz Schneider, Klaus E Matzel et al. The Differential Diagnosis and Interdisciplinary Treatment of Anal Carcinoma. Dtsch Arztebl Int. 2015 Apr 3;112(14):243–249. doi: 10.3238/arztebl.2015.0243. [DOI] [PMC free article]
[3] Winnie W Y Tong, Fengyi Jin, Leo C McHugh, Tara Maher et al. Progression to and spontaneous regression of high-grade anal squamous intraepithelial lesions in HIV-infected and uninfected men. AIDS. 2013 Sep 10;27(14):2233-43. doi: 10.1097/QAD.0b013e3283633111. [DOI] [PubMed]
[4] Julie S Hong, Victoria Yuan, Roger Patron-Lozano, Steven Y Chao. Diagnosis of Anal Cancer: Symptoms, Imaging, and Endoscopy. Surg Oncol Clin N Am. 2025 Jan;34(1):37-48. doi: 10.1016/j.soc.2024.06.002. Epub 2024 Jul 23. [DOI] [PubMed]
[5] National comprehensive cancer network. https://www.nccn.org/
[6] Ramez Kouzy, Joseph Abi Jaoude, Daniel Lin et al. Patient-Reported GI Outcomes in Patients With Anal Cancer Receiving Modern Chemoradiation. JCO Oncol Pract. 2020 Jul 1;16(12):e1524–e1531. doi: 10.1200/OP.20.00122. [DOI] [PMC free article]
[7] N D Nigro, V K Vaitkevicius, B Considine Jr. Combined therapy for cancer of the anal canal: a preliminary report. Dis Colon Rectum. 1974 May-Jun;17(3):354-6. doi: 10.1007/BF02586980. [DOI] [PubMed]
[8] Roman Volchenkov, Florian Sprater, Petra Vogelsang, Silke Appel. The 2011 Nobel Prize in physiology or medicine. Scand J Immunol. 2012 Jan;75(1):1-4. doi: 10.1111/j.1365-3083.2011.02663.x. [DOI] [PubMed]
[9] Karl R Aigner, Kornelia Aigner, Marc J H Hendrikx et al. Isolated hypoxic pelvic perfusion combined with electroporation is a valid alternative to traditional therapies for anal squamous cell carcinoma: a case study. Front Oncol. 2025 Aug 27:15:1644317. doi: 10.3389/fonc.2025.1644317. eCollection 2025. [DOI] [PubMed]
[10] L Leichman, N Nigro, V K Vaitkevicius, B Considine. Cancer of the anal canal. Model for preoperative adjuvant combined modality therapy. Am J Med. 1985 Feb;78(2):211-5. doi: 10.1016/0002-9343(85)90428-0. [DOI] [PubMed]
Read:
Treatment of stage 4 rectal cancer in Germany
Article menu:
- What is anal carcinoma?
- Symptoms of anal carcinoma
- Diagnostic methods of anal cancer
- Stages of anal cancer
- Treatment options for anal cancer
- Innovative methods for anal cancer treatment in Germany
- History of a patient with anal carcinoma
- A Medical Journey: Every Step of the Way With Booking Health
- Frequently Asked Questions About Anal Cancer
Don't know where to start?
Contact Booking Health