The treatment of liver cancer and liver cancer metastases is one of the most complex and challenging tasks, with this oncology type representing the 6th most common cancer worldwide with 866,136 new cases diagnosed in 2022 [6]. The diversity of primary cancers poses significant difficulties for both doctors and patients. Even more critical is liver metastasis due to other cancers, with some tumors, such as colon or lung cancer, showing a particular predisposition to form liver metastases. Up to 70 percent of people with colorectal cancer eventually develop liver metastases [7].
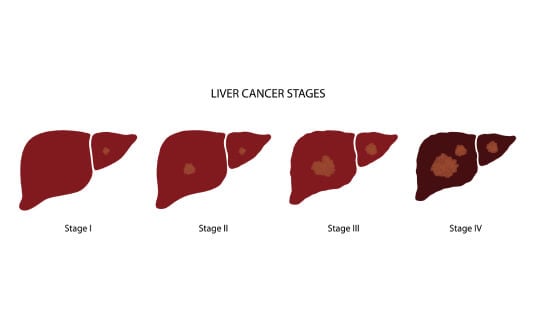
Liver involvement in cases of metastases at stage 4 is particularly severe, often indicating an incurable condition. This has led the medical community to delve deeper into the essence of this complex problem and develop specific treatment programs that include not only palliative procedures but can provide cancer control or even potentially cure the patient.
Etiology of the liver metastases in different cancer types
Most cases of primary liver cancer are hepatocellular carcinoma, which develops from hepatocytes (the main cells of the organ). Other types of primary liver cancer include cholangiocarcinoma, angiosarcoma, and hepatoblastoma, which originate from other cells and structures.
"Much more commonly, the liver is affected secondarily when cancer cells from other organs spread there through the blood vessels or lymphatic system."
Common types of oncology that often form secondary cancer loci in the liver include:
- Colorectal cancer. Cancer started in the cecum, colon, and rectum accounts for about 50% of metastatic liver cancer cases because blood from all unpaired abdominal organs enters the liver through the portal vein.
- Breast cancer. Approximately 30% of women with advanced breast cancer have liver metastases.
- Lung cancer. Approximately 30% of patients with cancer started in the lung have liver metastases on CT/MRI scans.
- Upper gastrointestinal tract cancer, most commonly stomach and esophageal cancers. Both lymphogenic/hematogenous and direct contact pathways of spread to the liver are relevant here, with the frequency of liver metastasis development ranging from 10 to 40%.
- Pancreatic cancer. Due to the peculiarities of the blood supply, up to 50% of patients with pancreatic cancer also have liver metastases.
The liver is an important detoxification organ that receives blood from all organs and tissues. It is therefore important to perform abdominal CT/MRI scans and exclude the presence of liver metastases for any advanced cancer.
Standard approaches to the treatment of metastatic liver cancer
The method of choice for the treatment of primary liver cancer and liver metastases is surgery combined with chemotherapy (regional or systemic; neoadjuvant, intraoperative, or adjuvant). The primary condition for a favorable treatment prognosis is the complete removal of all malignant foci.
Challenges faced by surgeons when performing operations for advanced primary cancer or metastatic cancer include:
- Extensive spread to the liver, due to which the patient has almost no organ parenchyma left uninvolved in the tumor process. Due to active blood flow, metastases often spread to both lobes.
- Decreased liver function after chemotherapy or prolonged use of other treatments.
- Decreased liver function due to concomitant diseases (cirrhosis or hepatitis) or age-related changes.
In this regard, patients with metastatic liver disease caused by other types of cancer or metastatic liver cancer could only be treated with palliative care for symptom relief. There was no talk that oncology could be controlled, and life expectancy increased. The situation changed with the advent of two-stage liver splitting surgery – ALPPS.
Principles of radical treatment of liver metastases and liver cancer
A unique feature of the liver is its ability to regenerate. It can fully restore its volume and normal function if at least 25% of healthy parenchyma remains after surgery. This gives surgical oncologists the ability to perform interventions that may seem absolutely impossible at first glance.
Curative (radical, that is, potentially bringing the disease under control) surgical treatment of primary and secondary malignant liver tumors has 2 basic principles:
- Total removal of all malignant foci in the liver, regional lymph nodes, and adjacent organs.
- Normal liver function in the postoperative period. This ensures detoxification, participation in all types of metabolism, synthesis of blood clotting factors, synthesis of bile for fat absorption, etc.
When cancer has spread to both lobes of the organ, it is very difficult to follow these principles because if the surgeon removes all the affected tissues, the patient will suffer from liver failure, a life-threatening condition, after surgery.
These requirements are met when performing an innovative operation – two-stage liver resection ALPPS (Associated Liver Partition and Portal Vein Ligation for Staged Hepatectomy) [1]. This surgical procedure allows the doctors to expand the possibility of radical treatment for unresectable or conditionally unresectable liver tumors and metastases, and gives patients a chance for recovery. Surgeons are no longer limited to classical anatomical resections, as ALPPS surgery is successfully performed for bilobar lesions and the preservation of less than 25% of healthy liver parenchyma [1].
How is liver surgery performed in liver metastases and liver cancer?
The success of the surgical intervention largely depends on its thorough planning. Preoperative preparation necessarily includes the following examinations:
- Imaging tests (ultrasound, CT/MRI) to assess the parameters of the primary tumor, the number and size of liver metastases, and the presence of fibrotic changes or steatosis
- Laboratory liver function tests, such as transaminase levels, bilirubin fractions, LDH, alkaline phosphatase, and protein fractions
- Blood tests for infections: all types of hepatitis and AIDS
During surgery planning, surgeons need to assess the volume of the future liver remnant (FLR) and its functional reserve. Nowadays, doctors can do this using modern computer programs, supplementing their clinical experience. For example, the Fraunhofer MEVIS team has developed software that analyzes data from imaging tests using mathematical models. The results of computer modeling allow surgeons to opt for complex surgery without any fear for the health of patients.
The first stage of the operation is splitting the liver totally or partially along the falciform ligament to the retrohepatic segment of the inferior vena cava with embolization or ligation of the right portal vein branch. The patient stays in the operating room for up to 3 hours. The surgeon sanitizes the left lobe of the liver, so it should not even contain microscopic malignant foci. This stage is followed by a blockage of blood flow in part of the portal vein. It leads to hypertrophy of the liver tissue, thus initiating the regeneration process.
The second stage of the operation is performed when the healthy parenchyma hypertrophies and liver function test parameters return to normal levels. This means that the functional reserve of the liver allows the doctors to proceed to the final stage of the operation, that is, extended right hemihepatectomy and removal of regional lymph nodes. Depending on the clinical case, there may be 1-2 weeks to 1-1.5 months between surgical procedures. The team of surgeons individually selects the optimal treatment for each patient.
Expert Insights on Advanced Liver Surgery Techniques in Liver Metastases and Liver Cancer
To provide deeper insight into the practical application of these innovative surgical approaches, we spoke with Dr. med. Michael Lipp, Head Physician of the Department of Abdominal and Colorectal Surgery at Asklepios Hospital Barmbek Hamburg, one of Germany's leading centers of excellence for liver surgery.
Dr. Lipp shares his experience with complex liver resections, including ALPPS procedures, and discusses how modern surgical techniques are expanding treatment possibilities for patients with liver metastases and primary liver tumors.
"Innovative Liver Resection Techniques: From ALPPS to Robotic Surgery" – Interview with Dr. Michael Lipp
Postoperative follow-up monitoring after treatment of liver metastases and liver cancer
The medical team pursues the following goals in the postoperative period:
- Make sure that the liver functional reserve is normal and that there is no liver failure
- Make sure that the treatment is radical and there is no tumor growth
- Provide patients with symptomatic treatment to improve their general health condition, and if necessary, plan rehabilitation
The patient spends the first day after surgery in the intensive care unit with constant monitoring of vital signs. In specialized clinics, this period is immediately followed by activation when the patient is transferred to a regular room, and they are allowed to move, gradually expanding the diet. Thanks to this, hypertrophy of the remaining hepatic parenchyma occurs more actively, and recovery is easier.
During the postoperative period, the team of oncologists can perform one or more courses of chemotherapy. After discharge from the hospital, the patient receives recommendations on nutrition and the intake of medicines, as well as information about follow-up examinations.
Combining Surgery with Other Advanced Liver Metastases and Liver Cancer Treatments
Modern metastatic liver cancer treatment achieves the best outcomes when surgery is combined with targeted therapies that attack cancer cells through multiple pathways. This comprehensive approach allows doctors to address both the primary tumor and microscopic cancer cells that may have spread throughout the body.
TACE for Liver Metastases and Liver Cancer: Delivering Chemotherapy Directly to Your Tumor
When tumors spread to the liver and cannot be surgically removed due to their size, location, or underlying liver conditions like cirrhosis, doctors can use a targeted approach called transarterial chemoembolization (TACE). This procedure allows physicians to deliver chemotherapy drugs directly to liver tumors while minimizing exposure to healthy tissue throughout the body.
During TACE, your doctor inserts a thin catheter through a blood vessel in your groin and carefully guides it to the hepatic artery that supplies blood to your liver tumor. Once positioned, chemotherapy drugs are injected directly into the tumor's blood supply, followed by tiny particles called emboli that block the blood vessel. This blockage serves two purposes: it traps the chemotherapy within the tumor for maximum effect and cuts off the tumor's oxygen and nutrient supply.
The advantages of chemoembolization over traditional chemotherapy include:
- Higher drug concentration: delivers chemotherapy doses up to 15 times higher directly to the tumor
- Reduced side effects: limits chemotherapy exposure to healthy organs throughout your body
- Extended tumor control: blocks blood supply to starve the tumor of oxygen and nutrients
- Preserved liver function: protects healthy liver tissue from unnecessary chemotherapy damage
Recent clinical trials have shown that combining TACE with newer immunotherapy and anti-angiogenesis drugs can significantly extend the time before cancer progresses, with patients experiencing 14-15 months of progression-free survival compared to 8-10 months with TACE alone [2].
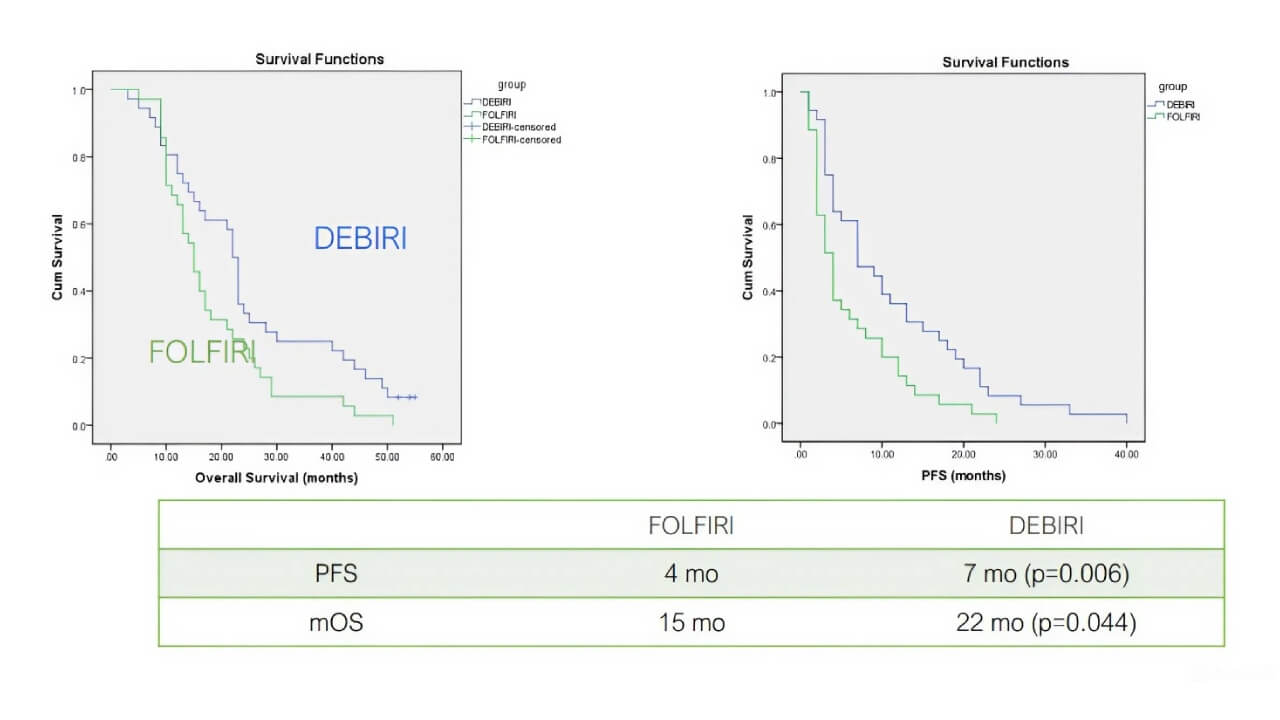
*i C et al Ancancer Res 2011;31:4581
Richardson A et al J Vasc Interv Radiol 2013;24:1209
This procedure is particularly valuable for intermediate-stage secondary liver cancer, where tumors haven't spread beyond the liver but cannot be surgically treated. To better understand how TACE works in practice, we spoke with Prof. Dr. Attila Kovács, a leading expert in interventional radiology.
Prof. Kovács: Why Interventional Oncology Should Be the Fourth Pillar of Cancer Care
Hyperthermia for Liver Metastases and Liver Cancer: Using Heat to Kill Cancer Cells
Hyperthermia therapy uses precisely controlled heat for treating liver metastases, offering an innovative approach for patients whose cancer cannot be surgically removed or for those seeking to enhance their existing treatments [3]. This thermal therapy raises tumor temperatures to 104-113°F, exploiting cancer cells' increased sensitivity to heat compared to healthy tissue.
The procedure involves different approaches depending on tumor location and size. Local hyperthermia uses radiofrequency ablation (RFA), where doctors insert a thin needle directly into the tumor under imaging guidance. The probe delivers high-frequency energy that creates targeted heat, destroying cancer cells within a specific area. Regional hyperthermia can heat larger liver sections, often combined with chemotherapy or radiation therapy.
The benefits of hyperthermia for secondary liver cancer patients are significant:
- Enhanced treatment effectiveness: increases chemotherapy and radiation therapy success rates by 30-50%
- Improved drug delivery: increased blood flow allows chemotherapy to penetrate deeper into tumors that have spread to the liver
- Immune system activation: heat triggers immune responses that help your body recognize and attack cancer cells
- Minimal side effects: precisely targeted treatment protects the surrounding healthy liver tissue
Research demonstrates that combining hyperthermia with radiation therapy increases complete response rates in tumors that have spread to the liver. The treatment is particularly valuable for tumors smaller than 2 inches and can be repeated if cancer returns. Most procedures are performed as outpatient treatments, allowing patients to maintain their quality of life while maximizing their cancer treatment effectiveness.
Dendritic Cells Vaccination for Liver Metastases and Liver Cancer: Training Your Immune System to Fight Cancer
Dendritic cell vaccination represents one of the most sophisticated approaches to cancer immunotherapy, building on groundbreaking research that earned Ralph Steinman the Nobel Prize in Physiology and Medicine in 2011 for discovering dendritic cells and their crucial role in immunity [5]. These specialized immune cells serve as powerful coordinators that recognize cancer cells and train other immune cells to attack them.
The treatment begins with collecting 150-200ml of your blood, from which dendritic cells are extracted and cultured in specialized laboratories for one week. During this time, these cells are "educated" using antigens from your specific cancer, creating a personalized vaccine tailored to your tumor's unique characteristics. The process operates under strict regulatory oversight, ensuring the highest safety standards.
Key advantages of dendritic cell vaccination include:
- Lifelong immunity: a single injection can boost your immune system's anticancer response for years
- Personalized treatment: vaccines are created using your own cells and tumor-specific antigens
- Minimal side effects: uses your body's natural immune mechanisms without toxic chemicals
- Complementary therapy: works alongside chemotherapy, radiation, and surgery without interference
For primary cancer and secondary liver cancer patients, dendritic cell therapy has shown effectiveness in constraining tumor growth and extending survival, particularly when patients cannot be effectively treated with conventional options [4]. The treatment is especially valuable for patients with liver metastases from other cancers or those requiring palliative care.
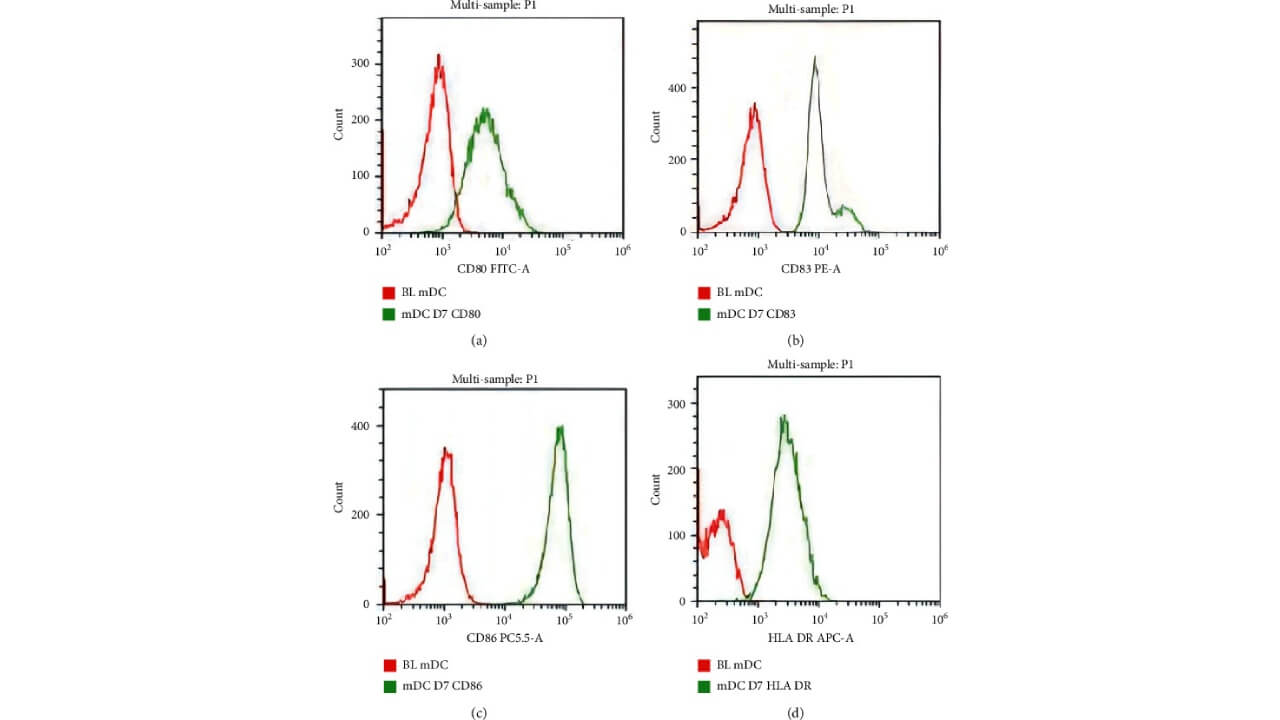
Copyright © 2022 Bohui Zhu et al.
To understand how this innovative therapy works in practice, we spoke with Professor Dr. Frank Gansauge, a leading immunotherapy specialist with over 22 years of experience in dendritic cell treatment.
Leading Immunotherapy Expert Prof. Frank Gansauge: "Revolutionizing Cancer Treatment with Dendritic Cell Therapy"
Liver cancer treatment options in European hospitals
When facing a liver cancer diagnosis, finding the right treatment center becomes one of your most important decisions. Clinical trials demonstrate that advanced procedures like ALPPS surgery can provide excellent long-term outcomes for patients with extensive liver lesions, multiple secondary cancer sites, or underlying conditions such as hepatitis or cirrhosis. These complex surgical interventions require surgeons with exceptional skill in delicately isolating blood vessels while preserving the function of healthy liver tissue.
The foundation of successful primary and secondary liver cancer treatment rests on having access to a multidisciplinary team that includes experienced hepatobiliary surgeons, interventional radiologists, medical oncologists, and specialized nursing staff. European medical centers, particularly those in Germany, have established themselves as leaders in comprehensive liver cancer care, combining cutting-edge technology with decades of clinical expertise.
If you're considering treatment abroad, taking time to research hospitals, review physician credentials, and understand treatment success rates will help you make an informed decision about your care. Many patients find it helpful to compare treatment options, from comprehensive programs that include initial diagnosis through rehabilitation, to specific procedures like ALPPS surgery, TACE, or immunotherapy.
When evaluating treatment centers, consider factors such as the hospital's experience with your specific condition, the availability of advanced treatment options, language support services, and coordination of care for international patients. Many specialized clinics offer assistance with medical record review, creating a treatment plan, and logistical support to help patients focus on their recovery rather than administrative concerns.
Remember that choosing the right treatment center is a personal decision that should align with your medical needs, comfort level, and treatment goals.
Best Hospitals for Liver Metastases Treatment in Germany
Modern liver metastases treatment requires high specialization, access to innovative technologies and coordinated work of a multidisciplinary team. That is why patients from all over the world are increasingly choosing treatment abroad (in particular in Germany). German clinics combine complex surgery, interventional oncology and modern systemic therapy. Individual treatment protocols for metastatic liver cancer are used here – which may include extended liver resections, ALPPS operations, TACE and immunotherapy. An important advantage is the consideration of each case by an interdisciplinary oncology team.
That is why Germany is considered one of the key destinations for patients looking for clinics for liver metastases treatment with predictable results, international safety standards and extensive clinical experience. Below are two leading German clinics, that specialize in the treatment of liver metastases and accept foreign patients.
Asklepios Hospital Barmbek Hamburg
Asklepios Hospital Barmbek is one of the leading centers for liver surgery and oncology in Germany. The clinic specializes in the treatment of complex and widespread metastatic liver lesions – including bilateral metastases and cases that are considered conditionally unresectable.
The clinic actively uses modern methods of liver metastases treatment. The high level of coordination between surgeons, oncologists and interventional radiologists allows the development of personalized treatment strategies even in complex clinical situations. Asklepios Hospital Barmbek is also known for its extensive experience in postoperative support and patient rehabilitation.
University Hospital of Ludwig Maximilian University of Munich
The University Hospital LMU Munich is one of the most prestigious academic medical centers in Europe and the undisputed leader among the best hospitals for liver metastases treatment. The clinic combines advanced scientific knowledge with extensive practical experience in the treatment of primary and secondary liver tumors.
Here a comprehensive approach to treatment for metastatic liver cancer is used – which includes highly accurate diagnostics, complex surgical interventions, interventional oncology and modern systemic therapy. Particular attention is paid to preserving the functional reserve of the liver and the patient's quality of life. Thanks to participation in international research, the clinic offers access to the latest treatment methods that have not yet become routine practice in many countries.
Best Hospitals for Liver Metastases Treatment
| Clinic | Country | Key Specialization |
|---|---|---|
| Asklepios Hospital Barmbek | Germany | Advanced liver surgery, ALPPS, interventional oncology |
| University Hospital of Ludwig Maximilian University | Germany | Surgical oncology, liver resection, systemic cancer therapy |
A Medical Journey: Every Step of the Way With Booking Health
Navigating complex liver cancer treatment decisions can feel overwhelming, especially when facing advanced disease or multiple treatment failures. With numerous specialists offering different opinions and treatment protocols varying significantly between medical centers, patients often struggle to identify the most effective approach for their specific situation.
Rather than settling for standard treatment protocols or first-available options, patients with liver cancer and liver metastases deserve access to the most advanced therapeutic interventions tailored to their unique clinical circumstances. This is where specialized medical expertise becomes invaluable.
Booking Health has spent over 12 years at the forefront of connecting patients with innovative liver cancer treatments, developing comprehensive expertise in complex hepatobiliary cases. Our medical coordinators are well-versed in the nuances of ALPPS surgery candidacy, TACE procedure selection, and the integration of immunotherapy for liver metastases management.
For patients considering advanced liver cancer treatment abroad, Booking Health provides:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
When facing liver cancer or liver metastases, your treatment decisions can significantly impact both survival outcomes and quality of life. Partnering with experienced medical coordinators who understand the complexities of advanced hepatobiliary treatments ensures that you receive personalized care tailored to your specific needs. Contact our medical consultant to learn more about the possibilities of treatment with innovative methods for liver cancer and liver metastases with leading specialists in this field.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
FAQ About Liver Metastases and Liver Cancer Treatment Options
Send request for treatmentThe newest treatments include ALPPS two-stage surgery for complex cases, TACE for delivering chemotherapy directly to tumors, hyperthermia therapy using controlled heat, and dendritic cell vaccination that trains your immune system to fight cancer cells.
Yes, non-surgical options include TACE, hyperthermia, HIPEC for certain cases, and immunotherapy with dendritic cells. These treatments can control tumor growth and extend survival when surgery isn't possible.
Leading clinics in Germany offer comprehensive liver cancer programs with advanced procedures like ALPPS surgery, TACE, and immunotherapy. These specialized centers provide multidisciplinary teams and cutting-edge technology for complex cases.
Treatment abroad provides access to specialized oncology centers with extensive experience in complex procedures, advanced technology, multidisciplinary care teams, and comprehensive support services for international patients throughout their treatment journey.
Unfortunately, early liver cancer has no symptoms and thus often not detected. Patients with advanced disease may complain of abdominal pain, weight loss and poor appetite, jaundice, etc.
The standard approaches are surgery combined with chemotherapy. For those seeking innovative treatments, ALPPS two-stage surgery, TACE, hyperthermia, and dendritic cell vaccination are available.
Dendritic cell therapy for liver cancer can cost €20,000-€38,000, TACE – €6,500-€24,000. The costs of ALPPS surgery depend on the complexity of the case. With Booking Health international patients receive transparent pricing without additional fees.
Innovative approaches such as transarterial chemoembolization, hyperthermia are the best treatment in difficult cases. These methods target cancer cells while sparing healthy tissue.
The best hospitals for liver cancer treatment are specialized centers with experience in interventional oncology and immunotherapy. Such hospitals have multidisciplinary teams, that combine advanced treatments for complex liver tumors.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Luigi Cioffi, Giulio Belli, Francesco Izzo et al. Minimally Invasive ALPPS Procedure: A Review of Feasibility and Short-Term Outcomes. Cancers (Basel). 2023 Mar 10;15(6):1700. doi: 10.3390/cancers15061700. [DOI] [PMC free article]
[2] NIH, National Cancer Institute. TACE-Based Treatment Combinations Effective Against Intermediate-Stage Liver Cancer. https://www.cancer.gov/news-events/cancer-currents-blog/2025/liver-cancer-tace-plus-targeted-and-immunotherapy
[3] P Moroz, S K Jones, B N Gray. Status of hyperthermia in the treatment of advanced liver cancer. J Surg Oncol. 2001 Aug;77(4):259-69. doi: 10.1002/jso.1106. [DOI] [PubMed]
[4] A H Lau, A W Thomson. Dendritic cells and immune regulation in the liver. Gut. 2003 Feb;52(2):307–314. doi: 10.1136/gut.52.2.307. [DOI] [PMC free article]
[5] Roman Volchenkov, Florian Sprater, Petra Vogelsang, Silke Appel. The 2011 Nobel Prize in physiology or medicine. Scand J Immunol. 2012 Jan;75(1):1-4. doi: 10.1111/j.1365-3083.2011.02663.x. [DOI] [PubMed]
[6] Statista. Rate of new liver cancer diagnoses in the U.S. as of 2021, by age. https://www.statista.com/statistics/951914/new-liver-cancer-cases-rate-by-age/
[7] Translational Cancer Research. Incidence and survival outcomes of secondary liver cancer: a Surveillance Epidemiology and End Results database analysis. https://tcr.amegroups.org/article/view/50241/html
[8] Bohui Zhu, Yiyuan Sun, Xiaoqing Wei et al. Dendritic Cell Vaccine Loaded with MG-7 Antigen Induces Cytotoxic T Lymphocyte Responses against Gastric Cancer. J Healthc Eng. 2022 Apr 18:2022:1964081. doi: 10.1155/2022/1964081. eCollection 2022. [DOI] [PubMed]
Read:
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
4 Stage Liver Cancer: Full Guide and Treatment Options
Treatment Methods and Advanced Therapies for Liver Metastases
Article menu:
- Etiology of the liver metastases in different cancer types
- Standard approaches to the treatment of metastatic liver cancer
- Principles of radical treatment of liver metastases and liver cancer
- How is liver surgery performed in liver metastases and liver cancer?
- Postoperative follow-up monitoring after treatment of liver metastases and liver cancer
- Combining Surgery with Other Advanced Liver Metastases and Liver Cancer Treatments
- Liver cancer treatment options in European hospitals
- Best Hospitals for Liver Metastases Treatment in Germany
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ About Liver Metastases and Liver Cancer Treatment Options
Don't know where to start?
Contact Booking Health