Ependymomas (EPN) represent approximately 5% of all central nervous system cancers – rare enough that many oncologists encounter only a handful of cases throughout their careers [1]. The rarity creates a challenge: this brain tumor treatment protocols lack the robust evidence base found in more common cancers. That is why expertise concentration matters – and Germany's specialized neuro-oncology centers offer precisely this advantage through multidisciplinary teams experienced in managing these uncommon tumors.
Adult ependymomas differ substantially from pediatric variants in biology, location, and behavior. While 60% of ependymomas occur in children younger than 16 years, adults account for fewer than 4% of adult nervous system tumors when combining brain or spinal cord (SP-EPN) ependymomas [1]. The stakes are high – complete surgical resection remains the single most significant predictor of outcome, yet recurrence rates remain troubling. Disease-free survival after relapse approaches only 15% at 5 years [1]. Modern way to treat ependymoma demands precision: microsurgical techniques, advanced radiation modalities like proton therapy, and emerging immunotherapy options including dendritic cell therapy – all available in Germany.
Understanding Rare Brain and Spinal Cord Tumor – Ependymoma
Ependymomas arise from ependymal cells – specialized cells lining the cerebral ventricles, the central canal of the spinal cord and filum terminale [1]. The tumors grow slowly, yet their location often causes significant ependymoma symptoms before diagnosis.
Adults constitute a minority of ependymoma patients. Among primary CNS tumors, ependymomas represent fewer than 4% of adult nervous system neoplasms [1]. The typical adult presentation skews younger – age under 55 years predicts better outcomes than 55 years or older [4, 6]. Performance status significantly influences prognosis, emphasizing the importance of maintaining functional capacity through scheme to treat ependymoma.
The pathology reveals interesting characteristics: immunohistochemistry demonstrates vascular endothelial growth factor (VEGF) expression in most cases – a finding with direct therapeutic implications [2]. Unlike other primary brain tumors, genetic pathology in ependymomas remains incompletely characterized despite extensive analysis [1].
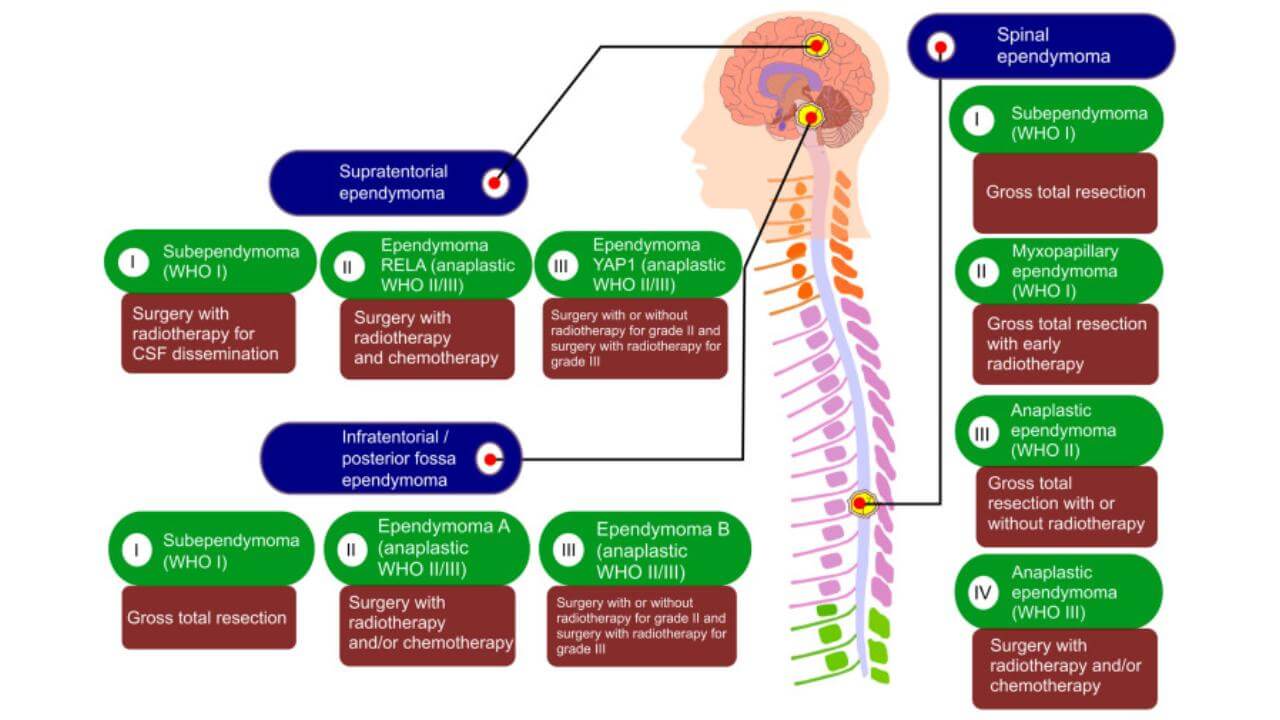
Approximately 60% of ependymomas are infratentorial, 40% supratentorial (ST-EPN). The single most common location is the fourth ventricle region. Spinal cord ependymomas, while less frequent in adults than brain tumors (BT), present distinct management challenges due to spinal cord radiation tolerance limits [9]. Cerebrospinal fluid (CSF) dissemination develops in 3-15% of intracranial ependymomas – more frequent with infratentorial and anaplastic variants [3].
WHO Brain Tumor Grading System: Grade 1, Grade 2, and Grade 3 Ependymoma
The World Health Organization classification divides ependymal tumors into three grades based on distinct histological features [6]:
Tumor Grade I encompasses subependymomas and myxopapillary ependymomas. Subependymomas are slow-growing benign neoplasms; myxopapillary variants occur mainly in the conus medullaris, cauda equina and filum terminale regions of the spinal cord in young adults. These are not cancers.
Tumor Grade II ependymomas represent slow-growing tumors of neoplastic ependymal cells – the most common category. These tumors show moderate cellularity without the aggressive features defining Grade III disease.
Tumor Grade III anaplastic ependymomas (AEPN) are malignant ependymomas. Grading relies on recognizing specific characteristics, like necrosis, mitotic activity, vascular proliferation, cytological atypia and cellularity degree. Mitotic activity measurement and endothelial proliferation particularly influence grade assignment. Low-grade tumors occur more commonly than high-grade variants [5].
The distinction carries prognostic weight. In a series of 152 intracranial ependymomas, 71.7% were Grade II and 28.3% Grade III. Five-year overall survival in high-grade disease reached approximately 60% compared to 95% in low-grade intracranial disease; at 10 years the figures were 45% versus 85% respectively [4].
Common Symptoms of Ependymoma in Adults
Clinical presentation varies dramatically with symptoms based on tumor location, size and grade [6]. Intraventricular ependymomas typically present with raised intracranial pressure secondary to mass influence or CSF pathway obstruction – brain tumor patients experience symptoms like nausea, vomiting, headaches, vertigo, ataxia and papilloedema.
Brain parenchymal tumors manifest through behavioral changes, memory loss or focal neurological deficits. Posterior fossa involvement produces visual disturbances, dizziness, ataxia and hydrocephalus.
The symptom complex often develops insidiously given the slow growth. Headaches may worsen over weeks to months. Visual changes might be subtle initially – double vision or peripheral field cuts. Ataxia presents as unsteadiness, difficulty with coordinated movements. At the same time, some patients experience acute decompensation when CSF flow becomes critically obstructed.
Spinal cord ependymomas present differently: with symptoms of backache, focal neurological deficits of upper or lower limbs [6]. The ependymoma symptoms depend on tumor level – cervical lesions may cause weakness or numbness in arms, thoracic tumors affect trunk sensation and coordination, lumbar involvement produces leg symptoms [9]. Bowel or bladder dysfunction can develop. Progressive motor weakness often brings brain tumor patients to medical attention.
Comprehensive Diagnosis of Ependymoma in Germany
Magnetic resonance imaging has superior diagnostic capability compared to computed tomography (CT) for determining diagnosis, brain tumor location and spread [6]. Ependymomas typically appear as well-detected lesions. Contrast enhancement degree varies according to grade – less likely in low-grade subependymomas, more pronounced in anaplastic variants. Brain parenchymal tumors prove difficult to distinguish from other brain tumor forms radiologically, which is why surgical resection serves both diagnostic and therapeutic purposes.
Complete staging requires MRI of brain and spine. For high-grade tumors, CSF examination is essential for diagnosis and brain tumor dissemination detecting. Thin-slice imaging, multiple sequences including T1-weighted with gadolinium, T2-weighted, FLAIR, and diffusion-weighted imaging – German centers have 3-Tesla MRI systems with specialized software.
When tumor location is suggested to allow safe resection, stereotactic biopsy provides tissue diagnosis with minimal risks. Frame-based or frameless navigation systems allow precise targeting. Tumor tissue undergoes standard histopathological examination evaluating the critical features: necrosis, mitotic activity, vascular proliferation, cytological atypia and cellularity [5].
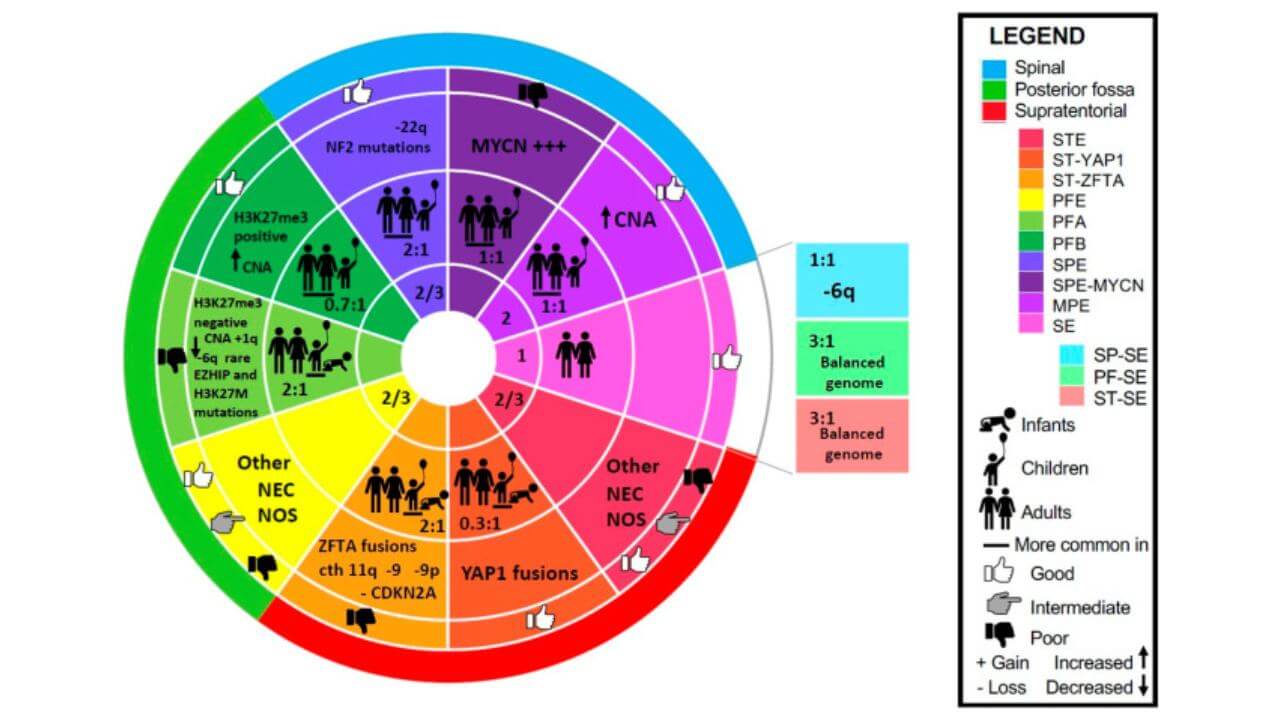
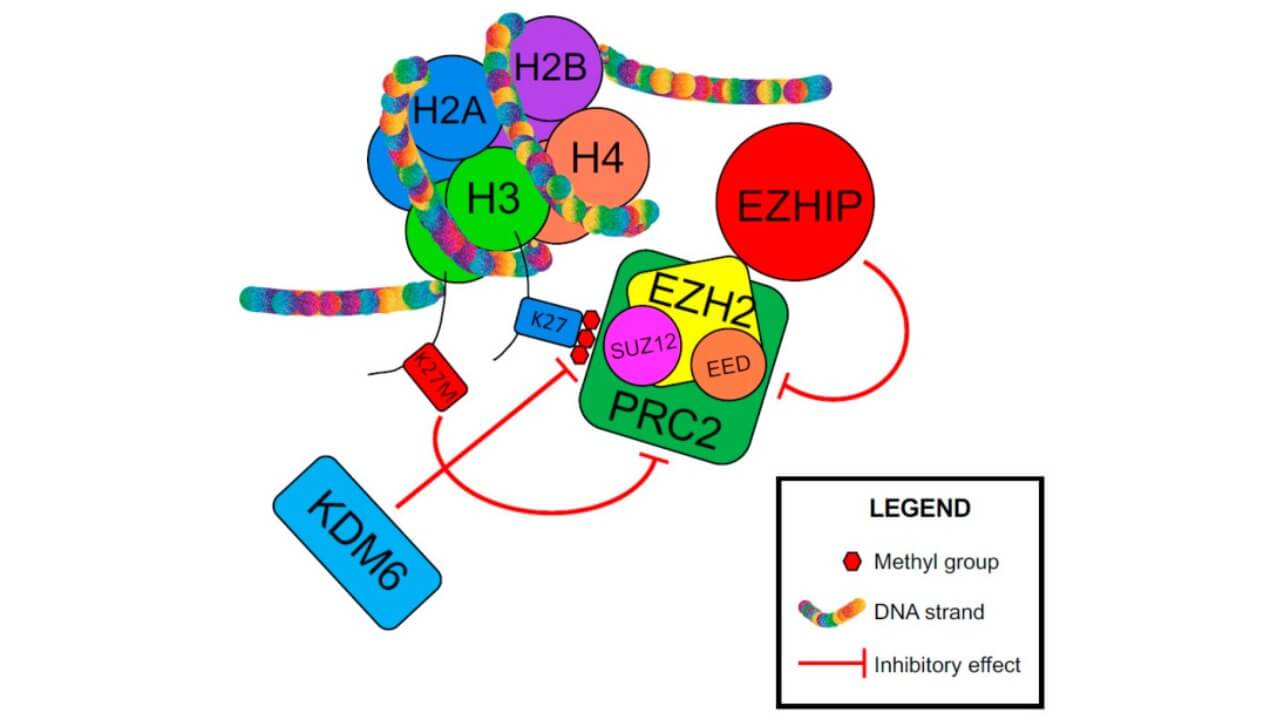
Ependymoma treatment in Germany increasingly incorporates molecular profiling. Testing evaluates chromosome 22q status, NF2 gene mutations particularly relevant in spinal ependymomas [4]. Assessment of RASSF1A methylation status and other epigenetic markers provides prognostic information. VEGF expression analysis – important given emerging role of targeted therapy (TMT) in recurrent disease [2].
German neuro-oncology centers employ multidisciplinary tumor boards where neurosurgeons, radiation therapy specialists, medical oncologists, neuroradiologists, and neuropathologists review each case collectively. This ensures diagnostic accuracy with consequent optimal treatment planning.
Ependymoma Treatment Options in Germany
Maximum possible surgical resection remains the mainstay of treatment. Numerous studies support more favorable prognosis with greater extent of resection – complete surgical resection is the most significant predictor of outcome. In localized cases where postoperative imaging shows residual tumor, "second look" ependymoma surgery is recommended unless contraindicated by proximity to eloquent structures [3].
When complete resection isn't possible, maximal debulking provides advantages: aids local control, provides histological diagnosis, and in some cases re-establishes CSF flow in obstructive lesions [6].
Neurosurgical Resection: The Foundation of Ependymoma Treatment in Germany
German centers of neuro surgery employ advanced microsurgical techniques including high-power microscope visualization, ultrasonic aspiration for tumor removal, and microsurgical instruments for delicate dissection. The goal – gross total resection whenever safely achievable – directly impacts long-term survival.
Intraoperative monitoring uses electrophysiological techniques to preserve neurological function during resection. Somatosensory evoked potentials monitor sensory pathway integrity. Motor evoked potentials assess corticospinal tract function in real-time. Cranial nerve monitoring – particularly vital for posterior fossa ependymoma – helps preserve function of nerves controlling eye movement, facial sensation, hearing, and swallowing. Intraoperative MRI available at select centers allows real-time assessment of resection completeness, reducing the need for repeat operations.
Radiation Therapy for Ependymoma
Radiotherapy (RT) is commonly used adjuvantly after complete surgical resection of localized high-grade ependymomas. In completely resected low-grade ependymomas, consensus is lacking on whether adjuvant radiotherapy is required. Each case should be decided on individual merit, considering histological characteristics spectrum and certainty of complete resection based on postoperative MRI [6]. There is broad agreement that radiotherapy is indicated for low- and high-grade lesions where residual disease is suspected after ependymoma surgery. Schild et al. quoted 5-year overall survival of 87% in low-grade and 27% in high-grade ependymomas with postoperative radiotherapy [5].
External beam radiation therapy (EBRT) forms the foundation of radiation treatment. Doses between 45 and 60 Gy represent general consensus. Most centers advocate 50.4–54 Gy to the tumor bed in lower grade cranial lesions with a margin of 2–2.5 cm from gross tumor volume to planning target volume. In higher grade disease, increasing the dose to 60 Gy is justified. In spinal sites, dose is usually limited by spinal cord radiation tolerance [9].
Intensity-modulated radiation therapy (IMRT) is designed for precise dose delivery to the tumor bed, it minimizes exposure to adjacent normal tissues. This sophisticated planning technique reduces toxicity significantly. Radiotherapy is conformally planned with fusion of preoperative imaging to define the tumor bed where appropriate.
Stereotactic radio surgery (SRS) delivers high-dose radiation in single or few fractions to small, well-defined targets. For ependymomas, it might have significant benefit when used as a boost to conventional radiotherapy and represents a reasonable option in recurrent disease. In the retrospective study of stereotactic radio surgery for recurrent ependymomas that included 17 lesions in 12 patients, in-field local control was achieved in 14 of 17 sites (82%); the estimated 3-year rate of local control was 68% [8].
Dr. Stoll discusses in this interview modern radiation therapy approaches for brain tumor treatment. He tells us about the precision techniques for ependymoma treatment in Germany and how technology advances improve outcomes.
Proton Therapy
Proton therapy represents an advanced radiation modality particularly valuable for ependymomas. Unlike conventional photon radiation, protons deposit most of their energy at a specific depth (the Bragg peak), minimizing exit dose to tissues beyond the tumor. This physical property allows higher doses to the cancer cells while sparing surrounding normal brain tissue.
For ependymomas – particularly those near critical structures like the brainstem, optic pathways of brain or spinal cord – proton therapy's precision offers substantial advantages. German proton centers employ pencil beam scanning technology for optimal dose distribution. The technique proves especially beneficial in young adults where long-term neurocognitive preservation matters significantly. Treatment planning actually uses the same target volumes as conventional radiotherapy does but achieves superior dose gradients.
Dendritic Cell Therapy (DCT): Immunotherapy Innovation
This is a worthy attention innovative immunotherapy approach available at specialized German centers. The 2011 Nobel Prize in Physiology or Medicine was awarded to Ralph Steinman for his discovery of dendritic cells, their role in adaptive immunity – recognition that underscores the therapy's value.
Dendritic cells are harvested from the patient's blood. They are then loaded with tumor cell antigens from the patient's blood (liquid biopsy) or tumor tissue, and matured in laboratory conditions before reinfusion – which is the final point of the medical intervention. Once returned to the patient, these activated dendritic cells train the immune system to recognize and attack remaining tumor cells. Lifelong anticancer immunity is created, the specialized one.
For ependymomas, DCT offers a personalized treatment option. German clinics with expertise in cellular immunotherapy attempt to integrate DCT into comprehensive treatment plans.
| Characteristic | Standard Treatment | Innovative Methods |
|---|---|---|
| 2-Year Survival Rate | ~30% for advanced-stage cases | ~55-65% in selected patients receiving multimodal therapies |
| Response Rate | Approx. 15% | 50-70% (depending on method and tumor cells profile) |
| Treatment Duration | 6-8 cycles over 4-6 months | Typically 3-5 sessions |
| Adverse Effects | High (nausea, immunosuppression, fatigue, hair loss) | Generally mild (localized pain, low systemic toxicity) |
| Ependymoma Cost in Germany | €80,000 - €150,000 full course | €25,000 - €60,000 full course |
*Based on clinical data from Booking Health.
Treatment Strategies for Recurrent or Metastatic Ependymoma
A significant number of patients – in one series 12 of 25, in another series 21 of 30 – with ependymomas will experience recurrence, and the dominant pattern is at the primary tumor site [6]. Because of the disease rarity, there is a paucity of available literature, making treatment of recurrent ependymomas very difficult. There is no standard salvage therapy of additional treatment. The prognosis of recurrent ependymomas treated with conventional methods is poor; survival is less than 15% at 5 years [6].
At relapse, all cases should be restaged with craniospinal MRI as leptomeningeal dissemination has been reported in 10% of patients with low-grade tumors and 30% with high-grade tumors [5]. The treatment options for ependymoma include surgery, radiotherapy and radio surgery, immunotherapy and systemic therapy.
Repeat Surgical Resection for Recurrent Ependymoma
In recurrent ependymomas, reoperation with attempted gross total resection should first be considered if at all possible. This is the case even if there is more than one site of recurrence. Multidisciplinary team discussion is essential. In one series, 2-year survival of 39% was achieved in a population of recurrent ependymoma patients with surgery at relapse in 90% of the cohort [10].
German neurosurgical centers approach repeat resection with the same meticulous technique as primary surgery – microsurgical dissection, intraoperative monitoring, and when available, intraoperative imaging. The surgical challenge often increases with recurrence due to scarring from previous operations and radiation changes.
First Radiation Therapy or Re-Irradiation
Despite a lack of randomised clinical data, general consensus exists that if a recurrent lesion is non-operable, radiotherapy should be offered to previously non-irradiated patients as an additional treatment [6]. In those previously treated, justification may exist to consider retreatment – either radio surgery for smaller lesions or external beam radiotherapy depending on previous treatment history and relative benefits.
There has been proven beneficial outcome with re craniospinal irradiation (CSI) in patients who already received radiotherapy. Kocak et al. reported three patients with recurrence of brain or spinal cord ependymomas treated with re-irradiation, with patients achieving a median disease progression-free period of 41 months [9]. For small volume suitable cases, radio surgery presents a radiation retreatment strategy with low morbidity; local control is achieved in most cases.
Recent data suggests that previous radiotherapy conditioning may actually enhance the effect of second-course radiotherapy – radiation-induced DNA damage appeared to show that previous radiotherapy was instrumental in achieving improved survival curves in re-irradiated patients [6]. Although these findings originated from pediatric studies, the phenomena warrant further investigation in an adult setting. German radiation oncology departments with extensive neuro-oncology experience can evaluate individual patients for re-irradiation candidacy.
Dendritic Cell Therapy (DCT)
Dendritic cell therapy holds particular promise in the recurrent setting where traditional options have been exhausted. For recurrent ependymoma, DCT can be administered as monotherapy or combined with other treatments. The personalized nature – using the patient's own tumor cell antigens – means each treatment is uniquely tailored. The DCT can be administered to patients who have had it in the complex scheme during the first treatment course and those who haven’t.
Professor Frank Gansauge discusses in this video dendritic cell therapy as an innovative immunotherapy option for patients with recurrent tumors. In simple words, he explains how this personalized approach harnesses the patient's own immune system to fight cancer.
Systemic and Targeted Therapy
Due to disease rarity, few data are available regarding chemotherapy role and there is no standard salvage chemotherapy for recurrent ependymomas in adult patients. Various chemotherapeutic regimens have been used with variable outcomes based on institutional experiences.
Platinum-based chemotherapy has been the hallmark of treatment. In the multicenter retrospective study, platinum-based regimens achieved response rates of 67% with median time to progression of 6 months; non-platinum regimens showed response rates of 13.3% with median time to progression of 10.9 months [7]. As is evident, platinum-based chemotherapy achieved higher response rates, but unfortunately, it did not prolong disease progression-free survival.
VEGF inhibitors represent an emerging therapeutic avenue. Green et al. showed reasonable response rates (75%) when using a VEGF inhibitor in combination with other agents as third-line treatment [2]. This suggests that earlier use in recurrent disease may be beneficial and should be subject of further studies [2]. The rationale is solid – ependymomas tend to show VEGF expression, making them theoretically susceptible to anti-angiogenic therapy [2].
German oncology centers with expertise in rare CNS tumors can access a broader range of systemic therapy options through compassionate use programs and clinical trials. Molecular profiling of recurrent tumors may identify additional targetable alterations for therapy selection.
Tumor ablation
To destroy small, recurrent tumors that cannot be removed via surgery, radiofrequency ablation or laser ablation may be used. These are minimally invasive approaches that use thermal energy to necrose tumor tissue and employ MRI guidance to deliver energy precisely. Real-time thermal monitoring ensures adequate treatment with protection of adjacent structures – every millimeter of brain tissue matters.
For ependymomas in locations where repeat surgery carries prohibitive risk – deep-seated lesions, proximity to eloquent cortex, or extensive scarring from previous operations – ablation offers an alternative. The procedure requires only a small burr hole rather than craniotomy that may result in mutilation; with ablation, recovery time and complications are minimal.
Professor Dr. Attila Kovács discusses in this informative video interventional cancer therapies beyond traditional surgery. These are thermal ablation techniques and more. He helps understand how to select the most appropriate interventional approach for individual patients.
Why Choose Germany for Ependymoma Treatment? Advantages for International Patients
Germany's healthcare system offers distinct advantages for international patients seeking ependymoma treatment. Specialized neuro-oncology centers concentrate expertise in managing rare CNS tumors – and that experience translates to better outcomes. Multidisciplinary tumor boards ensure every case receives comprehensive evaluation by neurosurgeons, radiation oncologists, medical oncologists, and other specialists working collaboratively.
Germany has advanced of even unique treatment options for ependymoma unavailable in many countries. German quality standards for medical care rank among the world's highest – with regulations ensuring patient safety and treatment efficacy.
Cost transparency is another important for international patients advantage. Ependymoma treatment in Germany means detailed cost estimates before treatment, and many accept international health insurance. For rare tumors like ependymoma where specialized expertise matters profoundly, the investment in German care offers access to comprehensive, cutting-edge treatment that may not be available elsewhere.
All of these make Germany a desired destination for ependymoma treatment – particularly for patients facing recurrent disease where treatment options are, unfortunately, limited and expertise is paramount.
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized ependymoma management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex cancer management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for different types of cancer with leading specialists in this field.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
FAQ: Ependymoma Treatment
Send request for treatmentCitizens and international patients can benefit here from multimodal approaches. Doctors choose among microsurgical resection, intraoperative monitoring, advanced radiation therapy (IMRT, stereotactic radiosurgery), proton therapy, innovative dendritic cell immunotherapy and other ependymoma treatment options in Germany – specialized centers offer all of these.
Ependymoma treatment cost can be from €80,000 to €150,000 for standard multimodal therapy; innovative approaches cost €25,000 to €60,000. Booking Health will help you navigate prices.
When tumors involve eloquent brain structures or spinal cord, brain surgery isn't always feasible. The most significant predictor of favorauble outcome is complete surgical resection. Stereotactic biopsy provides diagnosis, followed by radiotherapy or proton therapy. For inoperable recurrences, ablation techniques or DCT offer alternatives in such cases.
Survival rates vary significantly by grade and resection extent. Low-grade intracranial ependymomas show 95% 5-year survival with complete resection with no ependymoma symptoms. High-grade disease reaches approximately 60% at 5 years.
In Grade I and II tumors complete surgical resection offers best chance for cure. However ependymoma prognosis is complicated by recurrence risk — disease-free survival after relapse approaches only 15% at 5 years. That is why gross total resection is vital. Low-grade tumors with complete resection have excellent long-term outcomes, while high-grade variants require adjuvant therapy.
The exact cause remains unknown. Ependymomas arise from ependymal cells lining the ventricles and spinal cord central canal. Genetic factors play a role – chromosome 22q alterations and NF2 mutations appear in spinal variants.
Dendritic cell immunotherapy represents the most innovative ependymoma treatment advance. This personalized approach trains immune system to recognize tumor cells, creating lifelong anticancer immunity. German centers also offer proton therapy – minimizing radiation to healthy tissue, and VEGF inhibitors showing 75% response rates in recurrent disease. These methods demonstrate superior outcomes compared to conventional chemotherapy.
Specialized expertise matters for rare tumors like ependymoma. Proton therapy, dendritic cell immunotherapy are options unavailable widely. Cost of brain tumor surgery and all the interventions is transparent.
Comprehensive MRI staging, multidisciplinary tumor board review are the beginning. Microsurgical resection uses electrophysiological monitoring to preserve function and remove brain tumor signs. Advanced radiation includes IMRT and proton therapy. German centers integrate molecular profiling to guide therapy selection and offer innovative immunotherapy options.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Massimino M, Buttarelli FR, Antonelli M, Gandola L, Garrè ML, Gatta G, et al. Intracranial ependymoma: factors affecting outcome. Future Oncol. 2009;5(2):207-16. doi:10.2217/14796694.5.2.207. [DOI]
[2] Green RM, Cloughesy TF, Stupp R, DeAngelis LM, Woyshner EA, Ney DE, et al. Bev-mab for recurrent ependymoma. Neurology. 2009;73(20):1677-80. doi:10.1212/WNL.0b013e3181c1df34. [DOI]
[3] Kawabata Y, Takahashi JA, Arakawa Y, Hashimoto N. Long-term outcome in patients harboring intracranial ependymoma. J Neurosurg. 2005;103(1):31-7. doi:10.3171/jns.2005.103.1.0031. [DOI]
[4] Metellus P, Barrie M, Figarella-Branger D, Chinot O, Giorgi R, Gouvernet J, et al. Multicentric French study on adult intracranial ependymomas: prognostic factors analysis and therapeutic considerations from a cohort of 152 patients. Brain. 2007;130(Pt 5):1338-49. doi:10.1093/brain/awm046. [DOI]
[5] Schild SE, Nisi K, Scheithauer BW, Wong WW, Lyons MK, Schomberg PJ, et al. The results of radiotherapy for ependymomas: the Mayo Clinic experience. Int J Radiat Oncol Biol Phys. 1998;42(5):953-8. doi:10.1016/s0360-3016(98)00350-2. [DOI]
See more
[6] Reni M, Gatta G, Mazza E, Vecht C. Ependymoma. Crit Rev Oncol Hematol. 2007;63(1):81-9. doi:10.1016/j.critrevonc.2007.03.004. [DOI]
[7] Brandes AA, Cavallo G, Reni M, Tosoni A, Nicolardi L, Scopece L, et al. A multicenter retrospective study of chemotherapy for recurrent intracranial ependymal tumors in adults by the Gruppo Italiano Cooperativo di Neuro-Oncologia. Cancer. 2005;104(1):143-8. doi:10.1002/cncr.21110. [DOI]
[8] Stafford SL, Pollock BE, Foote RL, Link MJ, Gorman DA, Schomberg PJ, et al. Stereotactic radiosurgery for recurrent ependymoma. Cancer. 2000;88(4):870-5. https://doi.org/10.1002/(SICI)1097-0142(20000215)88:4<870::AID-CNCR18>3.0.CO;2-I. [DOI]
[9] Kocak Z, Garipagaoglu M, Adli M, Uzal MC, Kurtman C. Spinal cord ependymomas in adults: analysis of 15 cases. J Exp Clin Cancer Res. 2004 Jun;23(2):201-6. Review. [PubMed]
[10] Chowdhary S, Green MR, Chamberlain M. Ependymomas. Curr Treat Options Neurol. 2006;8(4):309-18. 10.1007/s11940-006-0021-y. [DOI]
[11] Larrew T, et al. Molecular Classification and Therapeutic Targets in Ependymoma. Neuro-Oncology. 2021;23(9):1287-1301. doi:10.3390/cancers13246218. [DOI]
[12] Seo SH, Paul SK, Shikder M, Khanam M, Ghosh P, Hasib TA, Ahmed KA, Sikdar S, Uddin MJ, Kwon Y. An insight into pathophysiological features and therapeutic advances on ependymoma. Cancers. 2021;13(13):3221. doi:10.3390/cancers13133221. [DOI]
Read:
Brain cancer treatments in Germany
Brain Astrocytoma Treatment – Full Guide: All New Astrocytoma Treatment Options
Article menu:
- Understanding Rare Brain and Spinal Cord Tumor – Ependymoma
- Common Symptoms of Ependymoma in Adults
- Comprehensive Diagnosis of Ependymoma in Germany
- Ependymoma Treatment Options in Germany
- Treatment Strategies for Recurrent or Metastatic Ependymoma
- Why Choose Germany for Ependymoma Treatment? Advantages for International Patients
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ: Ependymoma Treatment
Don't know where to start?
Contact Booking Health