CRS and HIPEC for Ovarian Cancer in Germany
Treatment prices are regulated by national law of the corresponding countries, but can also include additional hospital coefficients. In order to receive the individual cost calculation, please send us the request and medical records.

Department of Adult and Pediatric Gynecology, Mammology, Obstetrics
According to the Focus magazine, the Department of Adult and Pediatric Gynecology, Mammology, Obstetrics is included in the ranking of the top German departments specializing in obstetrics and breast cancer treatment! The department offers the full range of diagnostics and treatment of diseases of the female reproductive system, breast pathologies. Also, the specialists of the department provide a comprehensive management of pregnancy, childbirth and postpartum care for both mother and child. Key attention is paid to the treatment of female genital cancers, as well as breast cancer treatment. For this purpose, the department has all the modern therapeutic techniques, as well as its our own innovative developments by the department doctors.







Department of Adult and Pediatric Gynecology, Mammology, Obstetrics
The Department of Adult and Pediatric Gynecology, Mammology, Obstetrics offers high-precision diagnostics and effective treatment of the full range of diseases of the female reproductive system and breast pathologies. The medical facility also employs a competent team of obstetricians, whose responsibilities include comprehensive management of pregnancy, childbirth, and postnatal care for mother and baby. More than 3,000 babies are born in the department's delivery rooms annually. The department cooperates closely with the UniFee Reproductive Medicine Center, which allows gynecologists to treat female infertility together with reproductive medicine specialists. The department's gynecologists focus on women with reproductive system cancers. The medical facility is certified by the German Cancer Society (DKG) as a specialized center. The specialists also successfully treat endometriosis, one of the most common benign gynecologic diseases. In the field of mammology, priority is given to the provision of medical care to women with breast cancer. Doctors perform comprehensive diagnostics, surgical and conservative treatment, and reconstructive plastic surgery after mastectomy. The department's specialists use state-of-the-art technical resources and their professional skills to provide each patient with high-quality medical service.






Department of Adult and Pediatric Gynecology, Mammology, Obstetrics and Reproductive Medicine
The Department of Adult and Pediatric Gynecology, Mammology, Obstetrics and Reproductive Medicine offers the full range of surgical and conservative treatment of pathologies of the female reproductive system, breast, as well as top-class obstetric services, including management of birth and postnatal care for both mother and baby. The department also has a Center for Reproductive Medicine, where one can undergo comprehensive diagnostics to detect the causes of infertility and use modern assisted reproductive technologies. The department's excellent technical equipment, highly qualified medical staff and the availability of advanced treatment methods allow providing optimal and individualized treatment at the highest level. The treatment of female reproductive cancers is of primary interest to the department's gynecologists. The department also admits girls and young women with congenital anomalies of the genital organs, menstrual disorders, delayed or premature puberty.





- Understanding Ovarian Cancer
- Diagnostics of Ovarian Cancer
- What Is Cytoreductive Surgery (CRS)?
- Introduction to HIPEC (Hyperthermic Intraperitoneal Chemotherapy)
- CRS and HIPEC Combination for Ovarian Cancer
- Indications and Patient Profile for CRS + HIPEC in Germany
- Advantages of Receiving HIPEC in Germany
- Leading Hospitals for CRS and HIPEC in Germany
- Cost of CRS and HIPEC in Germany
- Hospital Stay, Recovery, and Follow-up Care
- A Medical Journey: Every Step of the Way with Booking Health
Ovarian cancer continues to pose a significant global health challenge – particularly because it is often diagnosed at an advanced stage when treatment becomes more complex and survival rates decline sharply. Globally, around 75 % of patients are diagnosed with advanced ovarian cancer (FIGO stage III-IV), where the disease has already spread throughout the peritoneal cavity [1].
In Germany, approximately 7,350 women were newly diagnosed in 2018, and roughly 5,291 died from the disease in 2019. Despite improved early-stage outcomes – with five-year survival rates up to 88 % in stage I – most cases are identified later, resulting in a 5‑year survival rate of only 42 % for advanced stages [2].
In this context, combining cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) has been recognized as a highly effective therapeutic strategy. Specifically, cytoreductive surgery (CRS) aims to remove all visible tumor burden, while hyperthermic intraperitoneal chemotherapy (HIPEC) delivers heated, localized chemotherapy directly into the abdominal cavity – enhancing drug penetration and effectiveness against residual microscopic disease.
International patients seeking advanced treatments, such as ovarian cancer CRS + HIPEC, can access this therapy in Germany, increasing their survival rates and quality of life. With modern facilities, experienced gynecologic oncology specialists, and personalized care approaches, the country offers some of the best clinical outcomes for complex cases of ovarian cancer, including with peritoneal metastases.
Understanding Ovarian Cancer
Ovarian cancer is relatively uncommon but poses a serious threat, especially in advanced stages with peritoneal metastases. For example, in the U.S., approximately 10.3 new cases per 100,000 women per year and 5.9 deaths per 100,000 women per year were reported between 2018 and 2022 [3].
Key risk factors include:
- Age: Incidence peaks in women aged 55-64, with a median diagnosis age of 63 [3].
- Genetics and family history: Women with BRCA1/BRCA2 mutations or a family history of ovarian or breast cancer are at significantly higher risk [4].
- Reproductive history: Nulliparity (never having given birth) increases risk, while pregnancy and breastfeeding have a protective effect [5].
- Obesity: Recognized as a risk enhancer.
- Fertility drugs (e.g., ovulation stimulants, IVF): Data remains inconclusive. However, some studies indicate a slightly higher risk in infertile women treated with ovulation-inducing medications – especially if nulliparous – but overall evidence quality is low [4, 5].
Types and Staging
Ovarian cancer includes several histologic subtypes, with epithelial tumors being the most common (around 90%) [6]. Standard staging follows the FIGO/AJCC system:
| Stage | Description | 5-Year Survival* |
|---|---|---|
| I | Confined to ovaries | ~40-90% |
| II | Spread to pelvic organs (e.g., uterus, fallopian tubes) | ~70% |
| III | Spread within pelvis and abdomen | ~41% |
| IV | Distant metastases (e.g., lung, liver) | ~31% |
*Survival ranges based on large cohort data – localized disease has significantly higher survival than advanced disease with peritoneal metastases [7].
Symptoms of Ovarian Cancer by Stage
Ovarian cancer is known as the "silent killer" due to its elusive early symptoms. Only about 20% of cases are diagnosed at stage I or II [8]. As previously noted, most patients (over 75%) present with advanced-stage disease because early symptoms are vague and easily misattributed [9].
| Category | Early-Stage Symptoms (Stage I–II) | Advanced-Stage Symptoms (Stage III–IV) |
|---|---|---|
| Digestive/Abdominal | Bloating, indigestion, mild pelvic discomfort, early satiety | Severe bloating (ascites), abdominal distension, bowel obstruction |
| Urinary | Increased frequency, urgency | Urinary obstruction or difficulty emptying bladder |
| Systemic | Fatigue, subtle weight loss | Cachexia (severe weight and muscle loss), anemia, profound fatigue |
| Pain | Pelvic pain, occasional back pain | Persistent pelvic/abdominal pain, back pain from tumor spread |
| Respiratory | Rare | Shortness of breath (pleural effusion due to metastases) |
| Other | Menstrual irregularities (sometimes) | Visible abdominal swelling, loss of appetite, nausea/vomiting |
As evident, early symptoms are common to many non-cancerous conditions (e.g., irritable bowel syndrome, urinary tract infection, or gastrointestinal issues). What distinguishes ovarian cancer is the persistence and worsening of these signs over weeks to months. Healthcare professionals often advise women to seek medical evaluation if such symptoms occur more than 12 times a month or progressively worsen despite routine treatments [8, 9].
Diagnostics of Ovarian Cancer
Early diagnosis of ovarian cancer remains one of the greatest challenges in gynecologic oncology. Nevertheless, a combination of laboratory tests, imaging studies, and surgical assessment helps improve diagnostic accuracy [8, 9].
Clinical Examination
- Pelvic examination: Detects adnexal masses or abnormal ovarian enlargement.
- Rectovaginal examination: May provide additional information about tumor spread in the pelvis.
While clinical findings are useful, they are rarely sufficient for a definitive diagnosis and must be supported by imaging and laboratory tests.
Imaging Techniques
Ultrasound (transvaginal and abdominal):
- First-line tool to assess adnexal masses.
- Solid, irregular, or heterogeneous tumors with increased vascularity raise suspicion of malignancy.
Computed Tomography (CT) with contrast:
- Evaluates disease extent, lymph node involvement, and peritoneal metastases.
- Helps determine surgical resectability prior to CRS.
Magnetic Resonance Imaging (MRI): Useful for complex adnexal masses when ultrasound results are inconclusive.
Positron Emission Tomography (PET-CT): Detects distant metastases or recurrence.
Laboratory Tests
- CA-125: Elevated in ~80% of women with advanced ovarian cancer but not specific to the disease.
- HE4 (Human Epididymis Protein 4): More specific than CA-125, particularly useful for distinguishing malignant from benign masses.
- ROMA Score (Risk of Ovarian Malignancy Algorithm): Combines CA-125 and HE4 with menopausal status to improve predictive accuracy.
Surgical and Pathological Diagnosis
The gold standard for confirming ovarian cancer is surgery with histological evaluation:
- Diagnostic laparoscopy or laparotomy: Allows direct visualization of tumor spread, biopsy of suspicious lesions, and sometimes simultaneous primary cytoreductive surgery.
- Histopathology: Determines the tumor subtype (serous, mucinous, endometrioid, clear cell) and guides treatment.
What Is Cytoreductive Surgery (CRS)?
Cytoreductive surgery (CRS) is a surgical technique aimed at removing as much visible tumor tissue as possible, particularly in cases of peritoneal carcinomatosis – commonly seen in advanced ovarian cancer. By reducing the tumor burden, CRS makes remaining cancer cells more vulnerable to chemotherapy and increases overall treatment efficacy. The primary goal is maximal tumor debulking, with "no macroscopic residual disease" being the ideal outcome.
Surgical Approaches: Primary Surgery vs. Interval Debulking
There are two main strategies for implementing CRS:
- Primary surgery (also called primary debulking surgery, or PDS): CRS is done before any chemotherapy.
- Interval debulking surgery (IDS): CRS follows several cycles of neoadjuvant chemotherapy (NACT), with the intention to shrink tumors before surgical removal.
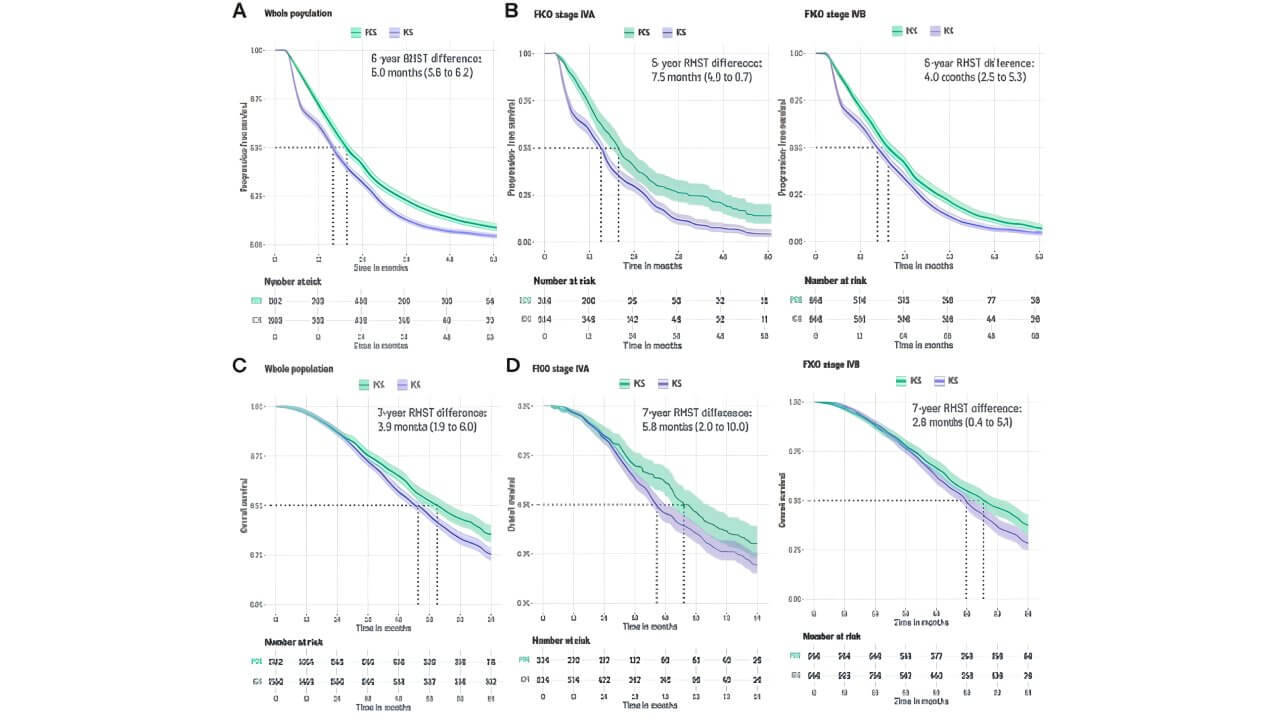
Clinical evidence shows clear benefits of primary surgery in appropriately selected patients. For example, a 2025 study demonstrated that primary cytoreductive surgery – when feasible – led to significantly longer progression-free survival (PFS): 19.7 months vs. 15.7 months, and a numerical gain in overall survival (OS): 63.1 months vs. 55.6 months. These findings established that PDS improved both 5-year PFS by around 5 months and 7-year OS by around 3.9 months when compared with interval surgery, even in the most advanced FIGO stage IVB cases [10].
Comparison of PCS vs ICS on Progression-Free and Overall Survival. [10]
Impact on Survival in Advanced Ovarian Carcinoma
Moreover, extensive data demonstrates a survival advantage when maximal cytoreduction is achieved. For example, a systematic meta-analysis highlighted that intrathoracic and abdominopelvic CRS substantially improves overall and progression-free survival in advanced ovarian cancer, with acceptable complication rates [11].
Introduction to HIPEC (Hyperthermic Intraperitoneal Chemotherapy)
Hyperthermic intraperitoneal chemotherapy (HIPEC) is a specialized form of intraperitoneal chemotherapy, involving the direct infusion of heated chemotherapeutic agents into the peritoneal cavity immediately following cytoreductive surgery (CRS). Unlike systemic chemotherapy – which circulates through the bloodstream and distributes body-wide – intraperitoneal hyperthermic chemotherapy delivers high drug concentrations directly to the site of tumor recurrence, reducing systemic exposure and related toxicity.
Mechanism – Heated Local Chemotherapy After CRS
In hyperthermic intraperitoneal chemotherapy (HIPEC), chemotherapeutic agents are heated (typically to 41-43 °C) and circulated within the abdominal cavity for a set duration (usually 60-90 minutes). This process enables better penetration into residual tumor tissue, especially microscopic disease that remains post-CRS [12].
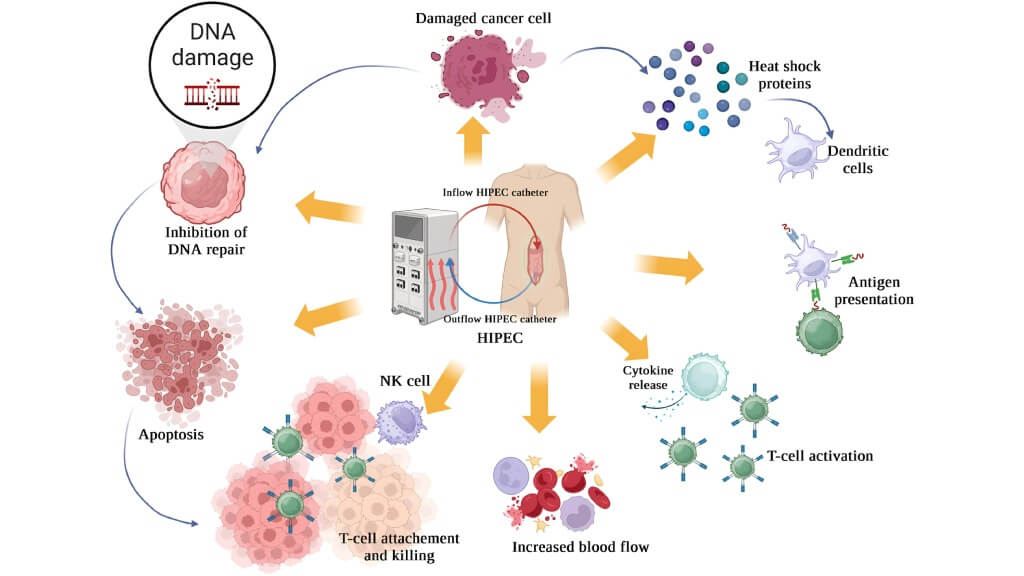
The Multidimensional Mechanism of Action of Hyperthermic Intraperitoneal Chemotherapy (HIPEC). [13]
Drug Penetration and Hyperthermia Effect
The approach of heated perfusion and localized delivery enhances therapeutic efficacy through multiple mechanisms [12, 13]:
- Enhanced drug uptake and deeper tissue penetration compared to systemic routes.
- Selective cytotoxicity: Hyperthermia disrupts cancer cell membranes and DNA repair, amplifying the chemotherapeutic effect.
- Plasma-peritoneal barrier limits systemic absorption – maximizing local concentration while minimizing systemic side effects.
Unique Advantages for Patients with Peritoneal Carcinomatosis Treated with HIPEC
Hyperthermic intraperitoneal chemotherapy (HIPEC) offers several distinct benefits for peritoneal carcinomatosis treated via CRS. Specifically, meta-analyses reveal improved disease-free survival (DFS) and OS, particularly when residual tumor is ≤1 cm or not visible [14].
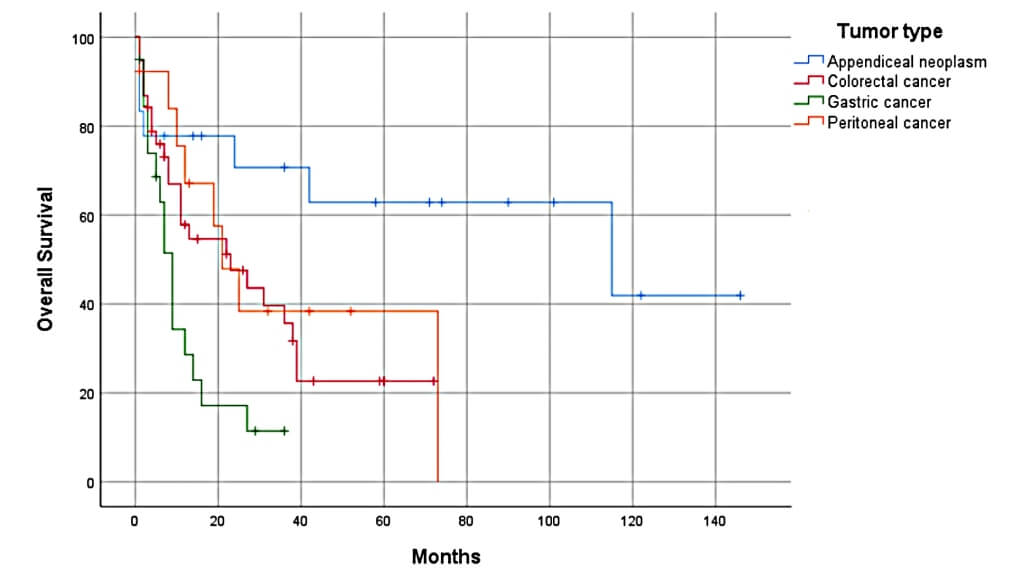
Moreover, before hyperthermic intraperitoneal chemotherapy (HIPEC), peritoneal carcinomatosis was largely untreatable, with average survival around six months. However, with CRS + HIPEC, long-term survival and even cures have been documented in select patients [12].
Overall Survival According to Primary Tumor Types. [12]
In addition, hyperthermic intraperitoneal chemotherapy (HIPEC) following CRS protects against microscopic recurrence by delivering heated chemotherapeutic flow across the entire peritoneal surface (a concept well-suited for ovarian cancers, which often remain confined within the peritoneal cavity) [15].
CRS and HIPEC Combination for Ovarian Cancer
As seen from the discussion provided above, the CRS and HIPEC combination pairs two complementary strategies: cytoreductive surgery (CRS) removes bulky, visible tumor tissue, while hyperthermic intraperitoneal chemotherapy (HIPEC) targets microscopic residual disease within the peritoneal cavity. By doing so, this approach exploits the strengths of both procedures – maximizing tumor clearance and enhancing the efficacy of chemotherapy directly at the tumor site.
Survival Benefits in Advanced Ovarian Cancer
Clinical data demonstrates tangible survival gains with the combined approach in advanced ovarian cancer. For example, a retrospective study showed that 5- and 10-year overall survival, disease-specific survival, and disease-free survival rates were significantly higher in patients treated with CRS and HIPEC (hyperthermic intraperitoneal chemotherapy). Specifically, these patients were 67% less likely to die from any cause, 75% less likely to die from cancer, and 46% less likely to develop recurrence compared to patients treated with CRS alone [16].
Indications and Patient Profile for CRS + HIPEC in Germany
In gynecologic oncology, the most common indication for CRS + HIPEC in Germany is advanced stage epithelial ovarian cancer with peritoneal metastases. This presentation is typical for more than 70 % of women at diagnosis [2]. Patients with primary ovarian cancer who have undergone neoadjuvant chemotherapy followed by interval cytoreductive surgery are among the most likely to benefit from the addition of hyperthermic intraperitoneal chemotherapy (HIPEC) [17].
CRS + HIPEC is also considered for [18]:
- Selected patients with recurrent ovarian cancer, if complete or near-complete macroscopic cytoreduction is achievable.
- Certain other peritoneal surface malignancies, provided the disease is confined to the abdominal cavity.
Contraindications to CRS + HIPEC
It is important to remember that CRS + HIPEC is a major surgical intervention with significant physiological demands. Contraindications for hyperthermic intraperitoneal intraoperative chemotherapy include:
- Poor performance status (ECOG ≥ 3)
- Severe comorbidities (e.g., uncontrolled cardiac or pulmonary disease)
- Extra-abdominal metastases (e.g., lung or brain)
- Inability to achieve complete or near-complete cytoreduction based on preoperative imaging
- Advanced malnutrition or hypoalbuminemia (<3.0 g/dL), which may impair postoperative recovery
Advantages of Receiving HIPEC in Germany
Germany is internationally recognized for its high-quality medical care, supported by excellent diagnostic capabilities, modern surgical approaches, and strict adherence to evidence-based protocols. Many German hospitals use advanced perfusion systems for hyperthermic intraperitoneal chemotherapy (HIPEC) that ensure precise temperature control and optimized drug distribution.
CRS + HIPEC is a technically demanding procedure that requires surgical expertise and deep knowledge of tumor biology. This is why Germany's experienced gynecologic oncologists are often trained in both oncologic surgery and peritoneal surface malignancy management.
Personalized Treatment Programs for Advanced Ovarian Carcinoma
Moreover, German certified cancer clinics follow the German Cancer Society (DKG) and European Society of Gynaecological Oncology (ESGO) guidelines, ensuring standardized yet highly individualized care. For patients with advanced ovarian carcinoma, treatment personalization includes:
- Detailed imaging and staging to determine resectability.
- Histopathological and molecular profiling to guide drug choice in hyperthermic intraperitoneal chemotherapy (HIPEC).
- Tailored perioperative care, including nutritional optimization and enhanced recovery after surgery (ERAS) protocols.
- Integration of systemic therapies post-HIPEC for optimal long-term disease control.
Personalization is critical: even among patients with similar disease stages, the choice between upfront surgery, interval CRS + HIPEC, or systemic therapy alone depends on individual tumor biology, treatment response, and surgical risk profile.
Leading Hospitals for CRS and HIPEC in Germany
Germany offers access to some of the best clinics in the world for advanced ovarian cancer treatment, providing high-quality CRS + HIPEC procedures. These institutions combine surgical expertise, modern technology, and multidisciplinary teamwork to achieve high success rates.
International patients can receive CRS + HIPEC treatment at:
- University Hospital Tübingen: Known for its strong surgical oncology department, the hospital's CRS + HIPEC program specializes in complex peritoneal surface malignancies, including ovarian cancer with peritoneal involvement.
- University Hospital Ulm: Offers a dedicated peritoneal cancer surgery unit with experienced surgeons performing high volumes of cytoreductive surgery annually. Their hyperthermic intraperitoneal chemotherapy (HIPEC) program follows ESG standards, ensuring optimal outcomes and comprehensive perioperative care.
- University Hospital Carl Gustav Carus Dresden: A leader in complex oncologic surgeries, Dresden's gynecologic oncology division has specialized expertise in advanced ovarian cancer. Their CRS + HIPEC approach is supported by advanced imaging, precision perfusion systems, and effective postoperative rehabilitation services.
Cost of CRS and HIPEC in Germany
In Germany, the treatment cost for cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) typically falls between €55,000 and €75,000. This range reflects base hospital charges for the procedure itself and varies according to the hospital's pricing policies, the patient's condition, and the scope of the operation. In specialized cancer centers, CRS + HIPEC pricing may be at the higher end due to advanced infrastructure and multidisciplinary care teams.
Several factors determine the final cost:
- Hospital: University and ESGO-certified centers may have higher fees due to advanced facilities.
- Disease stage: More advanced disease often requires longer surgery and additional interventions.
- Complexity of surgery: The number of organs involved, extent of tumor resection, and need for reconstruction can all increase expenses.
- Length of hospital stay: Recovery time and any complications can significantly add to the bill.
Patients should also account for costs beyond the surgical procedure itself:
- Follow-up care: Regular imaging and lab tests to monitor for recurrence.
- Rehabilitation: Physical therapy and nutritional support for optimal recovery.
- Travel and accommodation: Particularly relevant for international patients.
- Medical travel package: Includes flights, local transfers, translation services, and accommodation for patients and companions.
Hospital Stay, Recovery, and Follow-up Care
After CRS + HIPEC in Germany, the average hospital duration ranges from 10 to 21 days, depending on the extent of cytoreduction, patient health status, and post-surgical progress. In high-volume HIPEC (hyperthermic intraperitoneal chemotherapy) centers, enhanced recovery protocols can shorten stays without compromising safety [13].
Post-Op Recovery and Rehabilitation
Post-op recovery following CRS + HIPEC is a critical phase, as the procedure is both extensive and physiologically demanding. Patients are typically admitted to an intensive or intermediate care unit for the first 24-72 hours to closely monitor vital signs, fluid balance, and organ function.
Rehabilitation begins early – often within 48 hours – under the Enhanced Recovery After Surgery (ERAS) framework, which has been shown to reduce complications and speed up functional recovery. This includes:
- Guided mobilization and physiotherapy
- Nutritional optimization to support healing
- Pain management tailored to minimize opioid use
- Respiratory exercises to prevent postoperative pneumonia
Multidisciplinary support from oncologists, nutritionists, physiotherapists, and psycho-oncology specialists helps improve both physical and mental well-being during recovery.
Follow-Up Treatment Protocols
A structured follow-up treatment plan is essential to detect recurrence early and maintain quality of life. German oncology guidelines typically recommend:
- First year: Clinical exams and CA-125 tumor marker tests every 3 months, with imaging (CT/MRI) as indicated.
- Years 2-3: Check-ups every 4-6 months.
- After year 3: Annual follow-up unless symptoms arise.
In some patients, maintenance therapy – such as PARP inhibitors for BRCA-positive cases – may be introduced to reduce recurrence risk.
Patients traveling from abroad often continue follow-up in their home country, with German clinics providing detailed discharge summaries and recommendations for local oncology teams.
A Medical Journey: Every Step of the Way with Booking Health
Finding the most effective strategy for treating advanced ovarian cancer can be overwhelming. Patients often face a complex mix of medical opinions, previous treatments, and an urgent need for the right next step. In such circumstances, it is easy to default to the first available option or follow a standard therapy pathway, even if more advanced and individualized options exist.
For women with peritoneal disease, the CRS and HIPEC combination represents one of the most promising innovative methods in modern gynecologic oncology. This approach – available in the best clinics in Germany – pairs extensive tumor removal with heated, targeted chemotherapy to attack residual cancer cells directly.
To make an informed choice and receive a personalized treatment plan tailored to your unique condition, you can rely on the expertise of Booking Health. For more than 12 years, Booking Health has specialized in connecting patients with certified cancer clinics that lead in CRS + HIPEC (hyperthermic intraperitoneal chemotherapy) protocols for ovarian cancer.
Our services include:
- Comprehensive assessment and analysis of your medical reports
- Development of an individualized cancer treatment program
- Selection of the most suitable clinic from Germany's leading HIPEC centers
- Preparation and submission of medical documentation to your chosen hospital
- Scheduling pre-treatment consultations with your care team
- Expert guidance throughout your hospital stay
- Follow-up care coordination after returning to your home country
- Handling all administrative formalities
- Assistance with visas and travel arrangements
- A dedicated personal coordinator and interpreter available 24/7
- Booking Health cost estimation for clear, transparent budgeting with no hidden costs
By entrusting your care to Booking Health, you gain access not only to the best surgical and oncologic expertise but also to efficient organization of every practical detail. This allows you to focus entirely on recovery while we ensure the treatment process is stress-free.
Your health is invaluable, and managing something so critical should only be entrusted to professionals with proven experience and integrity.
If you or a loved one has been diagnosed with advanced ovarian cancer, now is the time to explore every available option. Contact a Booking Health medical consultant today to learn more about personalized treatment opportunities with the CRS and HIPEC combination at the best clinics in Germany.
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.