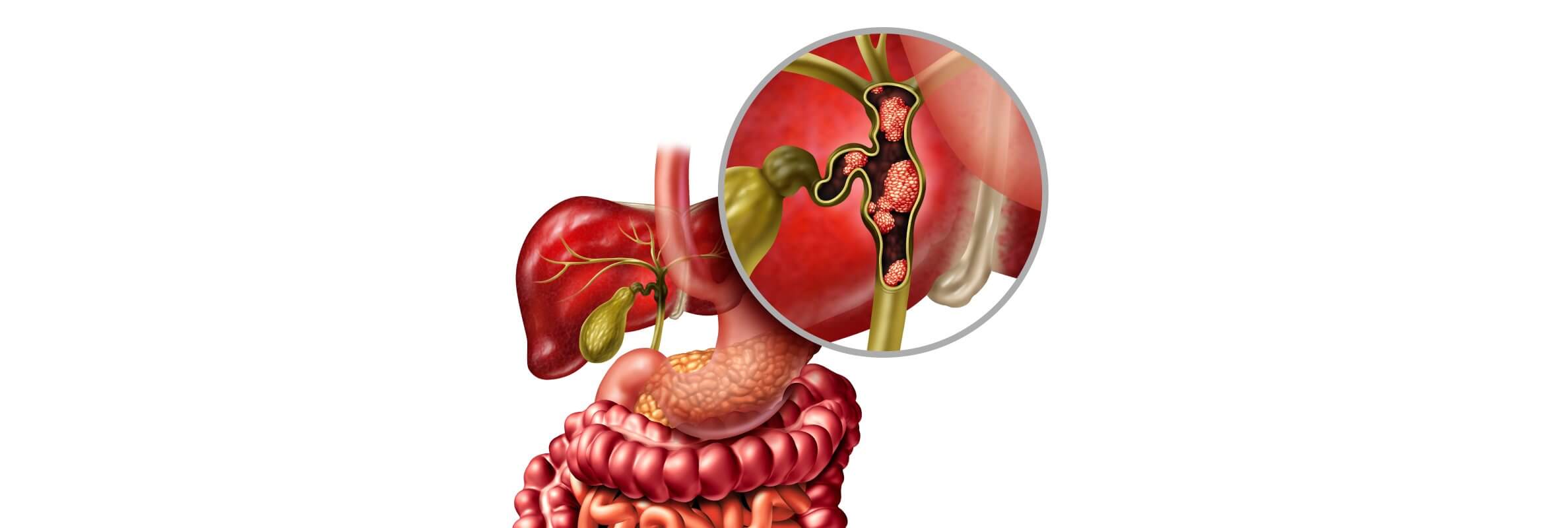
A Klatskin tumor, also known as perihilar cancer, is a type of extrahepatic cholangiocarcinoma, which starts in the area where the right and left bile ducts converge to form the common bile duct.
Classical Approaches to Klatskin Tumor Treatment
The standard Klatskin tumor treatment options typically include surgery, chemotherapy, and radiation therapy [1].
Surgical resection remains both the first-line therapy and the only curative option for perihilar cancer. However, tumor resectability is determined by several factors:
- Vascular involvement
- Liver function
- Tumor location
- The ability to get negative margins
However, surgery is usually associated with a whole range of complications and side effects that require intensive care. In addition, only around 20-35% of patients are candidates for surgery due to advanced local infiltration or fast distant spread of the malignant cells.
Systemic chemotherapy becomes the first-line treatment modality for patients with inoperable tumors or for those with recurrent disease. Neoadjuvant chemotherapy is also administered for select patients to downstage tumors before potential resection. Intensive chemotherapy, however, is often associated with severe side effects that prevent patients from continuing treatment.
Radiation therapy for Klatskin tumors plays more of a supportive, but increasingly defined role. It is often indicated as an adjuvant therapy after surgery or in cases of regional lymph node involvement. Radiotherapy is also preferred in palliative settings to alleviate local symptoms, such as those associated with bile duct obstruction. Even though novel technologies have enabled doctors to guarantee better tumor targeting, leading to reduced damage to the liver and other gastrointestinal structures, radiation therapy still causes systemic toxicity.
Innovations in Klatskin Tumor Treatment
The high number of severe adverse effects that caused patients to discontinue treatment, as well as the rapid growth of resistance, raised questions about the sustainability and, more importantly, the efficacy of the protocol treatment. This led to a search for novel, innovative therapies that are effective yet more patient-friendly. Immunotherapy, specifically dendritic cell vaccination, and interventional techniques, such as transarterial embolization, have emerged as a result.
Dendritic Cell Therapy for Klatskin Tumor
Dendritic cell therapy is an innovative, personalized type of immunotherapy that has recently gained traction for treating Klatskin tumors. Dendritic cells are antigen-presenting cells that play a crucial role in navigating immune responses by capturing tumor-associated antigens and presenting them to T cells. This interaction subsequently initiates a full-scale, tumor-specific cytotoxic response while minimizing damage to surrounding healthy tissues.
The significance of dendritic cells in immunology was recognized when Ralph Steinman, who first identified these cells, was awarded the Nobel Prize in Physiology or Medicine in 2011 [2]. Since then, researchers have actively investigated dendritic cell-based therapies, including those for perihilar cancer. Evidence suggests that dendritic cell therapy can be especially effective in unresectable or recurrent forms of perihilar tumors. A study of 36 post-operative patients, who underwent dendritic cell therapy, reported a slower disease progression as compared to patients who did not receive treatment. When used alongside systemic treatments, such as chemotherapy or radiotherapy, dendritic cells maintain a favorable safety profile, with adverse effects typically limited to mild symptoms, such as localized discomfort. Reports from various combined-modality treatments also indicate high tolerability, making dendritic cell therapy a preferred option, even for palliative patients.
Interventional Radiology for Klatskin Tumor
Interventional radiology has become an irreplaceable component in the multidisciplinary management of perihilar cholangiocarcinoma. It is particularly useful for patients with locally advanced or unresectable disease. These image-guided, minimally invasive procedures allow for tumor-targeted therapy with reduced systemic toxicity, which puts it on one line with surgery in some cases.
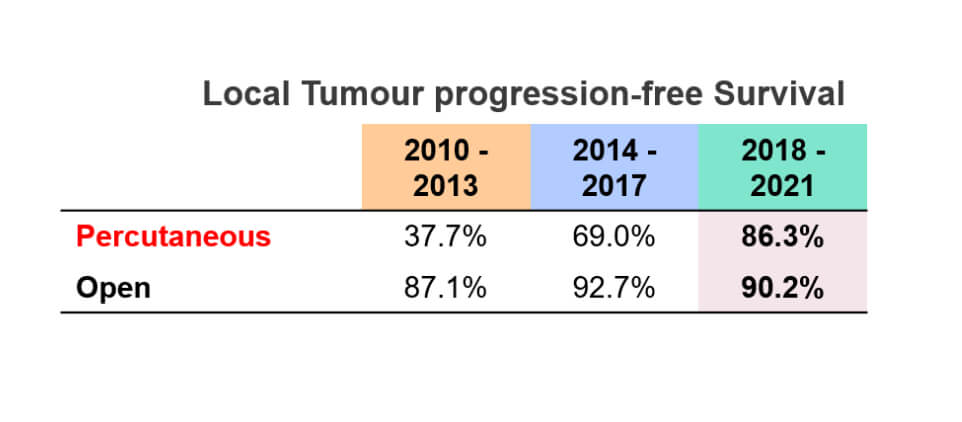
Thermal ablation, including radiofrequency and microwave ablation, uses heat to destroy malignant tissue precisely. [3] Recent reports suggest that thermal ablation may achieve local tumor control in up to 70% of lesions smaller than 3 cm when anatomical proximity to critical structures (such as portal vein) permits. Additionally, the progression-free time for thermal ablation is extremely high, helping to prevent disease recurrence. Meanwhile, microwave ablation allows for deeper penetration and faster heating, making it a viable option for lesions in surgically complex areas.
Cryoablation is an alternative minimally invasive therapy that applies subzero temperatures to induce cell death in tumors. It is especially crucial in cases where heat-based interventions may pose risks to nearby vessels. Clinical studies report local control rates of 60-80% and a favorable safety profile, which is especially vital for lesions in complex anatomical zones. Real-time monitoring of the ablation zone with top-tier imaging techniques adds to its high precision.
Electrochemotherapy (ECT) treatment for Klatskin tumor is a minimally invasive technique that combines electric pulses with regional chemotherapy [4]. Electro-chemotherapy increases the permeability of tumor cell membranes, thereby enhancing the cytotoxic effects. Although electrochemotherapy for Klatskin tumor is still being researched, early-phase studies report objective response rates exceeding 55% with minimal damage to surrounding tissues. What is more, ECT possesses an immunomodulating effect and can work synergistically with various immunotherapy modalities. Electrochemotherapy cost may not be that high when thinking about its value. You can find the cost of electrochemotherapy in different clinics on the Booking Health website.
Electrochemotherapy Explained: Why This "New Kid on the Block" is Changing Cancer Treatment
Regional Chemotherapy for a Klatskin Tumor
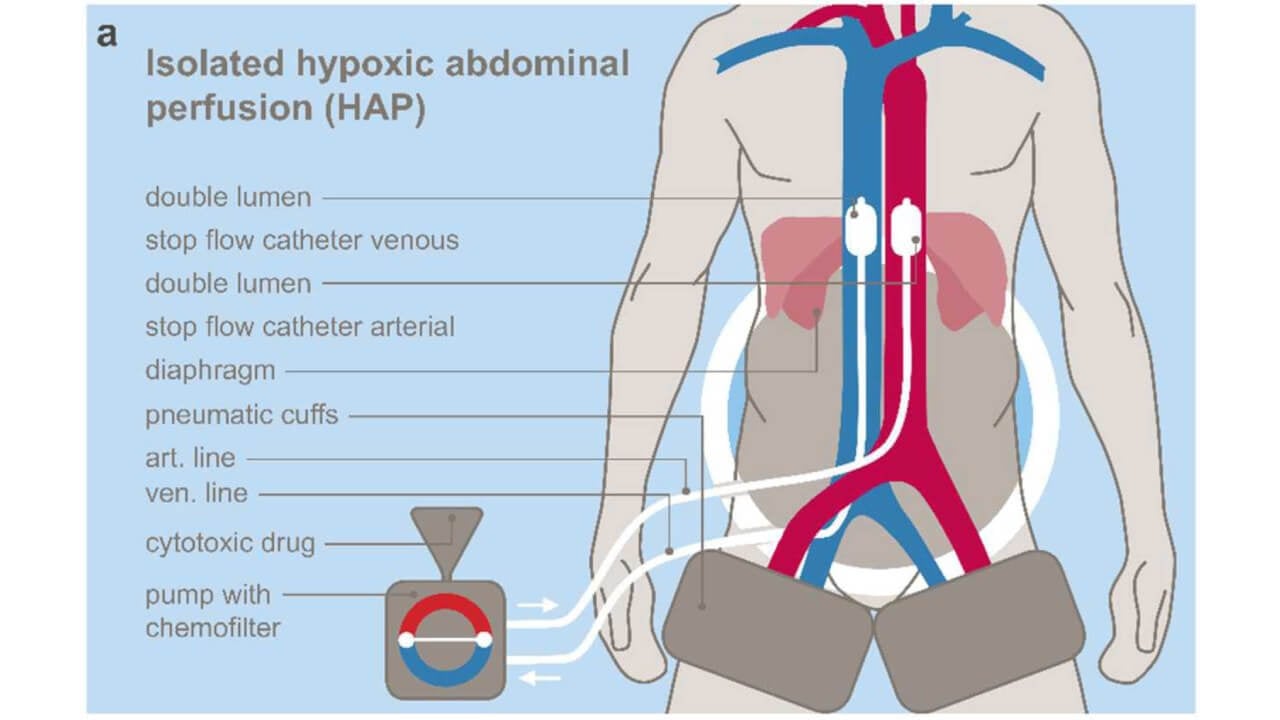
Perihilar cholangiocarcinoma presents unique treatment challenges. Regional chemotherapy for bile duct cancer emerged as a solution – targeting tumors precisely through arterial infusion and specialized perfusion techniques like hypoxic abdominal perfusion (HAP), upper abdominal perfusion (UAP), and isolated thoracic perfusion (ITP).
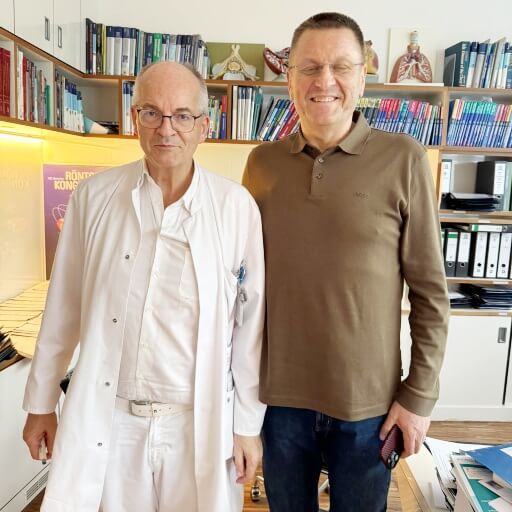
At Medias Klinikum Burghausen, Prof. Karl R. Aigner developed regional chemotherapy in Germany specifically for metastatic perihilar disease. His team treated patients across 189 cycles, with remarkable findings: median survival hit 23 months, 38% showed partial tumor response, another 41% achieved disease stabilization. The point is – these results surpass conventional systemic approaches significantly.
The process is charmingly simple. Blood flow gets isolated to tumor regions, concentrated agents flood the malignancy to destroy cancer cells, while chemo-filtration cleans venous blood before it re-enters circulation. This dual mechanism ensures maximum tumor impact with minimal systemic damage. Bile duct cancer regional chemotherapy treatments proved safe even for weakened patients (ECOG 2-3) – no grade III or IV complications occurred, making this vital for those who cannot tolerate standard intensive protocols.
Transarterial Chemoembolization for Klatskin Tumor
Transarterial chemoembolization (TACE) is a targeted, minimally invasive therapy increasingly applied for bile duct cancer treatment, particularly in advanced or stage IV Klatskin tumor cases [5]. This minimally invasive procedure implies delivering high concentrations of chemotherapeutic drugs directly into the tumor through the hepatic artery while simultaneously obstructing the tumor's blood supply. The dual mechanism significantly enhances tumor necrosis and minimizes systemic toxicity.
TACE has demonstrated encouraging results in patients with perihilar cancer. A retrospective study involving unresectable cases of Klatskin tumor demonstrated a median overall survival increasing from 3.3 months with supportive care to 12.2 months with TACE, underlining its potential to prolong life in advanced stages. Moreover, a comparative study of 64 patients with bile duct cancer, including Klatskin tumors, revealed that the 12-month survival rate after TACE treatment exceeded 50%. This rate was significantly higher than the 8.3% survival rate of those who received only supportive care. Additionally, when combined with systemic chemotherapy, TACE has shown synergistic effects, further improving treatment efficacy.
TACE has a favorable safety profile, making it a well-tolerated option, even for fragile patients. The minimally invasive nature of the intervention contributes to low complication rates. These characteristics, alongside a small number of side effects, position TACE as a viable alternative to systemic treatments for patients with unresectable tumors. [6]
| Characteristics/Therapy type | 2-Year Survival Rate | Response Rate | Duration | Side Effects |
|---|---|---|---|---|
| Standard Treatment | ~25% for advanced cancer | Less than 10% | Several cycles | Severe (nausea, fatigue, hair loss, immunosuppression, skin irritation) |
| Innovative Methods | ~60% for advanced cancer | 45-65% | Up to 4 sessions | Mild (localized discomfort) |
*Booking Health data
Comparison of Cost for Standard vs. Innovative Treatments for Klatskin Tumor
| Treatment Method | GERMANY* | Great Britain | USA |
|---|---|---|---|
| Standard Treatment | €80,000 - €150,000 full course | €90,000 - €165,000 full course | €100,000 - €180,000 full course |
| Innovative Methods | €25,000 - €60,000 full course | €70,000 - €120,000 full course | €100,000 - €150,000 full course |
*Costs may vary depending on the type and duration of the treatment, as well as the combinations of methods used for each individual clinical case
Leading Klatskin Tumor Clinics in Germany
Germany is considered one of the leading destinations for Klatskin tumors treatment. Here specialized Klatskin tumor hospitals combine many years of clinical experience, modern technologies and a multidisciplinary approach to the treatment of complex oncological cases. These key features allow achieving optimal results even in patients with locally advanced or unresectable tumors.
Klatskin tumor treatment centers in Germany work on the principle of close cooperation between different specialists (abdominal surgeons, oncologists, gastroenterologists, interventional radiologists and radiotherapists). Here individual treatment plans are developed – which may include surgical resection, systemic and regional chemotherapy, radiation therapy (as well as modern minimally invasive interventions). Thanks to this approach, hospitals for Klatskin tumor treatment in Germany demonstrate better survival rates and symptom control compared to standard protocols.
Below are three reputable Klatskin tumor clinics in Germany that are trusted by international patients and have strong expertise in bile duct tumors treatment.
University Hospital RWTH Aachen
University Hospital RWTH Aachen is a large university hospital with a strong scientific and clinical base – specializing in the treatment of complex oncological diseases of the abdominal cavity. The clinic is known for its high level of abdominal and hepatobiliary surgery.
A multidisciplinary approach is used here for Klatskin tumor treatment with a careful assessment of resectability, vascular involvement and functional state of the liver. Thanks to modern equipment and individual planning of interventions doctors strive to achieve radical treatment with minimal postoperative risks.
LMU University Hospital
LMU University Hospital in Munich is one of the largest university medical centers in Europe and boasts one of the world's top oncology schools. The clinic is widely known for its experience in the treatment of rare and aggressive tumors (including perihilar cholangiocarcinoma).
Patients with Klatskin tumors have access to modern surgical techniques, systemic and combination therapy, as well as innovative protocols – implemented within the framework of clinical programs. High survival rates make LMU one of the best hospitals for Klatskin tumor treatment.
Asklepios Hospital Barmbek
Asklepios Hospital Barmbek is a renowned multidisciplinary oncology center in Hamburg – this hospital has extensive experience in treating malignant tumors of the hepatobiliary system. The clinic specializes in systemic treatments and supportive care for patients with advanced forms of the disease.
Particular attention is paid here to preserving the quality of life, symptom control and the possibility of continuing treatment even in weakened patients. Thanks to this, Asklepios Hospital Barmbek is considered one of the best Klatskin tumor treatment centers in Germany.
Best Hospitals for Klatskin Tumor Treatment
| Clinic | City | Key Treatment Approaches |
|---|---|---|
| University Hospital RWTH | Aachen | Surgical procedures, adjuvant and neoadjuvant chemotherapy, radiation therapy, multidisciplinary management |
| LMU University Hospital | Munich | Advanced hepatobiliary surgery, systemic chemotherapy, combined chemoradiotherapy protocols, immunotherapy |
| Asklepios Hospital Barmbek | Hamburg | Systemic and palliative chemotherapy, supportive and symptom-oriented care, treatment of unresectable and metastatic Klatskin tumors, multidisciplinary oncology programs |
Fighting Off Klatskin Tumors At Advanced Stages: When Hope and Persistence Matter
A diagnosis of an advanced or metastatic Klatskin tumor can definitely feel devastating. Even though you may feel like giving up hope, you should remember that your treatment journey doesn't end here. Although traditional treatments may be less effective at advanced stages, cutting-edge innovations are changing the therapy landscape for Klatskin tumor in Germany. Emerging options like immunotherapy and interventional procedures now offer the patients real opportunities to slow disease progression, manage negative symptoms, and regain quality of life they thought was lost.
Many of these new approaches are personalized procedures tailored to your individual clinical scenario. They are also more patient-friendly, with fewer adverse effects and a shorter rehabilitation time. Klatskin tumor treatment in Germany makes novel medical technologies available to all patients regardless of staging. Therapies such as dendritic cells or chemoembolization are often delivered on an outpatient basis, which means a shorter hospital stay. Furthermore, interventional radiation techniques are associated with a reduced physical and emotional burden compared to standard and palliative care. Today, there is more reason than ever to hope, as breakthroughs in Klatskin tumor treatment grant patients time, strength, and a renewed sense of control.
When you feel like discovering treatment abroad, you don't need to start this whole process all over alone. Booking Health is your trusted partner that will take care of everything. Starting from finding the best oncology team among top hospitals in Germany and Europe to managing organizational questions on site, Booking Health utilizes its 10+ years of experience to arrange everything as smoothly as possible. Our all-inclusive services include:
- Document translation and on-site interpreting services
- Visa arrangements
- Transfer and hotel booking
- Transparent treatment costs with no hidden fees
- Absence of fees for international patients enabling them to save 40-70% on treatment costs
- Follow-up even after the completion of treatment
Innovations are indeed within your reach. Your medical journey has only started, and Booking Health will readily provide the navigating system to guide you through the world of top-tier technologies and breakthrough therapies for perihilar cancer.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
Frequently Asked Questions About Klatskin Tumor Treatment
Send request for treatmentA Klatskin tumor is a type of cholangiocarcinoma (bile duct cancer) that arises in the area where right and left bile ducts unite forming the common bile duct.
Diagnosis typically involves the following studies:
- Imaging (CT, MRI, PET, and ultrasound)
- Endoscopic techniques, such as ERCP (endoscopic retrograde cholangiopancreatography) and PTC (percutaneous transhepatic cholangiography), for visualizing the bile duct and taking a biopsy
- Tumor markers (CA 19-9)
Common symptoms include:
- Jaundice
- Skin itching
- Dark brownish urine
- Colorless stools
- Unintentional weight loss
- Fatigue
- Sometimes abdominal discomfort
Treatment may include:
- Surgical resection
- Systemic therapy (chemotherapy or radiation therapy)
- Percutaneous biliary drainage (endoscopic stenting) for palliative care
- Liver transplant (in select cases)
- Interventional techniques (TACE, thermal ablation)
- Immunotherapy (dendritic cells, targeted therapy)
Surgery is the preferred curative option, but it is only feasible in about 40-60% of cases due to late diagnosis. Non-surgical options such as immunotherapy are commonly used when the tumor is unresectable or when patients are not candidates for surgery.
A cure is possible with complete surgical resection with negative margins (R0 resection). However, recurrence is common, and long-term outcomes depend on early detection and tumor characteristics.
The prognosis is generally poor due to late presentation. The median survival rate is 12-24 months with treatment, though longer survival is possible with successful surgery.
Five-year survival is about 20-40% following curative surgery. In unresectable cases, the five-year survival drops below 10%.
Chemotherapy is primarily used for unresectable or metastatic disease. It may also be used as adjuvant therapy after surgery or in neoadjuvant settings before liver transplant.
Yes, but only for selected patients with early-stage disease and some cases of unresectable tumors who meet strict criteria. This treatment option is often used within a clinical protocol involving neoadjuvant chemotherapy.
An unresectable Klatskin tumor is the one that cannot be safely removed by surgery due to extensive vascular involvement, complex regional anatomy, presence of distant metastases, or overall poor patient condition.
Radiation therapy may be used as adjuvant treatment after surgery, in palliative setting for symptom control, or in combination with chemotherapy to improve local control in unresectable cases.
Targeted therapies are being explored for tumors with specific genetic alterations (FGFR2 fusions and/or IDH1 mutations). These are typically considered in advanced or refractory cases.
New treatments offered in Germany include personalized approaches, such as dendritic cell therapy, advanced radiology techniques (for example, thermal ablation or TACE), and liver transplant protocols for eligible patients.
In Germany, innovative treatments cost €25,000-€60,000 (for the full course), Great Britain charges €70,000-€120,000 and the USA – €100,000-€150,000. Costs vary depending on treatment type and duration.
2-year survival for advanced cancer with standard treatment is approximately 25%; innovative methods achieve higher – around 60%. Advanced therapies like dendritic cell immunotherapy and TACE are available in German hospitals.
Standard treatment shows less than 10% response rates; innovative methods demonstrate 45-65%. As for particular methods, thermal ablation achieves local tumor control in up to 70% of suitable lesions, and ECT reports objective response rates exceeding 55%.
Standard treatment requires several cycles over extended periods. Innovative methods typically involve limited number of sessions.
Standard treatment causes severe side effects: nausea, fatigue, hair loss, immunosuppression, etc. Innovative methods produce only mild effects, which is important for cancer patients.
Treatment of a Klatskin tumor depends on resectability and disease spread – management may include complex biliary surgery, interventional radiology, regional chemotherapy and others.
The best hospitals for Klatskin tumor treatment in Germany are high-volume hepatobiliary centers – these clinics have experience in advance treatments.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Science Direct. Klatskin Tumor. https://www.sciencedirect.com/topics/medicine-and-dentistry/klatskin-tumor
[2] PubMed. The 2011 Nobel Prize in physiology or medicine. https://pubmed.ncbi.nlm.nih.gov/22053831/
[3] Research Gate. Percutaneous Irreversible Electroporation of Unresectable Hilar Cholangiocarcinoma (Klatskin Tumor): A Case Report.
[4] European Review for Medical and Pharmacological Sciences. Electrochemotherapy of cholangiocellular carcinoma at hepatic hilum: a case report. https://www.europeanreview.org/wp/wp-content/uploads/7051-7057.pdf
[5] Journal of Liver Cancer. Transarterial chemoembolization for hepatocellular carcinoma: 2023 expert consensus-based practical recommendations of the Korean Liver Cancer Association. https://www.e-jlc.org/journal/view.php?doi=10.17998/jlc.2023.05.22
[6] Science Direct. The effect of trans arterial chemoembolization in the management of intrahepatic cholangiocarcinoma. A systematic review and meta-analysis. https://www.sciencedirect.com/science/article/abs/pii/S0748798322000105
[7] Yogesh Vashist, Kornelia Aigner, Sabine Gailhofer and Karl R. Aigner. Therapeutic Effect of Regional Chemotherapy in Diffuse Metastatic Cholangiocarcinoma. Cancers 2022, 14(15), 3701; https://doi.org/10.3390/cancers14153701. [DOI]
Read:
Bile Duct Cancer Treatment: Cholangiocarcinoma Treatment Options Guideline
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
Top 10 Leading Oncology Hospitals for Cancer Treatment in Germany
Article menu:
- Classical Approaches to Klatskin Tumor Treatment
- Innovations in Klatskin Tumor Treatment
- Comparative Table of Treatment Methods and Their Costs
- Leading Klatskin Tumor Clinics in Germany
- Fighting Off Klatskin Tumors At Advanced Stages: When Hope and Persistence Matte
- Frequently Asked Questions About Klatskin Tumor Treatment
Don't know where to start?
Contact Booking Health