Living with small intestine cancer can be challenging, but there's reason for hope. Though rare, this condition now has more treatment pathways than ever before. The five-year survival rate for early-stage disease can exceed 80% with proper treatment, making timely, specialized care crucial. While conventional treatments like surgery, chemotherapy, and radiation form the foundation of care, innovative approaches such as HIPEC, PIPAC, TACE, and immunotherapy are transforming outcomes for patients. Don't surrender to a limited prognosis. Connecting with specialists who offer these breakthrough therapies could significantly improve your quality of life and extend survival beyond initial expectations.
The Hidden Challenge: Understanding Small Bowel Cancer
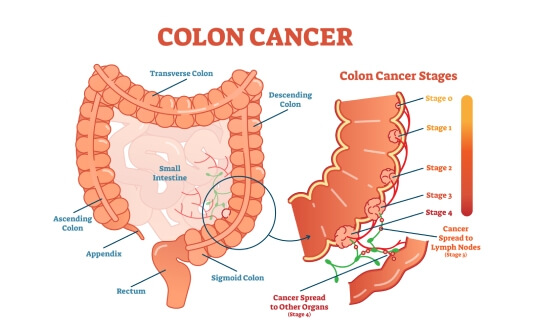
Small bowel cancer is a rare yet formidable diagnosis, accounting for only 3-5% of all gastrointestinal malignancies despite the small intestine comprising 90% of the GI tract's surface area. This discrepancy makes these cancers particularly challenging to detect and treat.
The five main small intestine cancer types include:
- Adenocarcinoma – most common in the duodenum, arising from glandular cells
- Neuroendocrine tumors – primarily found in the ileum, derived from hormone-producing cells
- Lymphoma – affects lymphatic tissue throughout the small bowel
- Gastrointestinal stromal tumors (GISTs) – arise from interstitial cells of Cajal
- Sarcoma – a rare tumor originating from muscle tissue
Diagnosis is often delayed due to vague symptoms like abdominal pain, weight loss, and occult bleeding. Five-year survival rates vary significantly: early-stage disease may exceed 80% with proper small intestine cancer treatment, while advanced cases with nodal involvement drop to approximately 40%. This stark contrast highlights the critical importance of early detection and innovative treatment approaches.
Foundation Treatments for Small Bowel Cancer: Surgery, Chemotherapy & Radiation
Standard treatments for cancer in small intestine provide a foundation for care but have recognized limitations:
Surgical resection:
- Primary treatment for localized disease
- Involves wide segmental removal with adjacent mesentery
- Whipple procedure may be necessary for tumors in the proximal duodenum
- Limitations: not viable for advanced or metastatic disease; complex anatomical considerations
Chemotherapy:
- Typically used as adjuvant therapy following surgery
- Limited effectiveness compared to other GI cancers due to the small number of clinical trials
- Significant side effects that impact quality of life
Radiation therapy:
- Less commonly used due to complications with abdominal radiation
- May be considered in specific localized cases
- Limited evidence for survival benefit
While these traditional approaches form the cornerstone of treatment for small intestine cancer, their effectiveness plateaus with advanced disease. This underscores the need for innovative therapies that can overcome the limitations of conventional methods, which we'll explore in the following sections.
HIPEC for Small Bowel Cancer: Cancer-Fighting Heat in the Abdominal Cavity
Hyperthermic intraperitoneal chemotherapy (HIPEC) represents a groundbreaking approach for treating cancer of small intestine with peritoneal metastasis – a condition once considered virtually untreatable. This dual-action procedure combines cytoreductive surgery with heated chemotherapy delivered directly into the abdominal cavity.
The key advantages of HIPEC include:
- Delivers chemotherapy concentrations up to 15 times higher than systemic methods
- Precisely targets microscopic cancer cells that surgery cannot remove
- Heat enhances drug penetration and cancer-killing effects
- Minimizes systemic side effects while maximizing therapeutic impact
- Offers hope for patients with limited conventional options
The HIPEC procedure begins with cytoreductive surgery – an open abdominal operation where surgeons meticulously remove all visible tumor tissue. After complete tumor removal, specialized silicone drains are placed throughout the abdominal cavity. The surgical team then circulates a heated chemotherapy solution (typically 40-43°C) throughout the abdomen for 60-90 minutes using a perfusion device. This precise delivery method allows the heated medication to reach areas conventional surgery cannot access. The entire procedure typically takes 5-10 hours, with patients requiring 10-14 days of hospital recovery.
Recent studies show HIPEC can extend survival to 9-32 months with five-year survival rates reaching 25-40% – remarkable for a condition that traditionally offered few treatment pathways. While traditional surgery addresses visible tumors, HIPEC attacks invisible cancer cells, representing a comprehensive approach to small bowel cancer treatment.
Watch our exclusive interview with Dr. Michael Lipp, a leading HIPEC specialist, as he explains how this innovative procedure is transforming outcomes for patients with cancer of the small bowel and peritoneal metastasis.
"HIPEC Treatment: A Breakthrough in Advanced Abdominal Cancer Care" - Interview with Dr. Michael Lipp
PIPAC for Small Bowel Cancer: Precision Chemotherapy Through Pressurized Delivery
Small bowel cancer patients with peritoneal metastasis can now benefit from an innovative approach that delivers chemotherapy directly where it's needed without extensive surgery. PIPAC (Pressurized Intraperitoneal Aerosol Chemotherapy) transforms liquid chemotherapy drugs into a fine pressurized spray that penetrates tumor tissues more effectively than conventional methods.
During this laparoscopic procedure, surgeons make two small incisions in the abdomen to insert specialized equipment. Chemotherapy is aerosolized and sprayed under pressure throughout the abdominal cavity, remaining for 30 minutes before removal. The entire procedure takes just 60-90 minutes, with patients typically staying in the hospital for only 2-3 days.
Key advantages of PIPAC:
- Minimally invasive approach requiring only two small incisions
- Repeatable treatment that can be administered every 6-8 weeks
- Compatibility with systemic chemotherapy as a complementary treatment
- Lower physical burden than HIPEC, making it suitable for patients who cannot tolerate major surgery
- Shorter hospital stays – typically 2-3 days compared to 10-14 days with HIPEC
- Potential bridge therapy that may eventually enable more aggressive treatments
PIPAC is particularly valuable for patients with extensive peritoneal metastasis who aren't candidates for HIPEC. By addressing microscopic cancer cells throughout the peritoneum with significantly less physical stress, PIPAC offers hope where traditional surgical interventions may not be possible.
TACE for Small Bowel Cancer: Targeting Tumors with Direct Chemotherapy Delivery
For small bowel cancer patients with liver metastasis, transarterial chemoembolization (TACE) offers a powerful targeted approach that delivers treatment directly to tumor sites while sparing healthy tissues.
During this minimally invasive procedure, interventional radiologists insert a thin catheter into a large artery in the arm or leg, then thread it precisely to the blood vessels feeding the tumor in the liver. Through this catheter, they deliver a specialized mixture of chemotherapy drugs and embolic materials (either an oily liquid or absorbable gelatin sponge) directly to the cancer site.
This dual-action approach creates a powerful anti-cancer effect:
- Chemotherapy drugs attack cancer cells with concentrations up to 20 times higher than systemic delivery
- Embolic materials block blood vessels feeding the tumor, cutting off oxygen and nutrients
- The blockage keeps chemotherapy drugs in contact with the tumor longer, enhancing effectiveness
Key advantages for patients include:
- Dramatically reduced systemic side effects compared to traditional chemotherapy
- Precise targeting of liver metastases while protecting healthy tissues
- Outpatient procedure with minimal recovery time (typically 24-48 hours)
- Option for patients who cannot tolerate more aggressive interventions
- Can be combined with other treatments as part of a comprehensive approach
TACE is particularly valuable for patients with inoperable metastatic small bowel cancer that has spread to the liver. It is also used in complex schemes of colon cancer treatment and rectal cancer treatment. The procedure's minimal invasiveness makes it suitable even for elderly patients or those with significant health challenges, offering hope for disease control and improved quality of life.
Learn more about advanced chemoembolization techniques in our interview with Prof. Attila Kovács.
Prof. Kovács: Why TACE Doubled Cancer Survival – What Patients Need to Know
Harnessing the Immune System: Dendritic Cell Therapy for Small Bowel Cancer
Dendritic cell therapy is one of the most promising types of immunotherapy for bowel cancer, particularly for those who have exhausted conventional treatment options. This Nobel Prize-winning treatment leverages the body's immune system to recognize and fight cancer cells throughout the body.
The therapy works by reprogramming the immune system to identify and attack cancer cells specifically. First, dendritic cells are collected from the patient's blood through a simple procedure similar to blood donation. These cells are then processed in a specialized laboratory where they're "educated" to recognize proteins from the patient's specific small bowel cancer. Once re-injected into the patient's bloodstream, these enhanced cells activate T-cells that seek out and destroy cancer cells throughout the body.
Key benefits for small bowel cancer patients:
- Personalized treatment tailored to each patient's unique cancer profile
- Minimal side effects compared to chemotherapy and radiation
- Whole-body approach that can address metastatic disease
- Compatible with other treatments, including surgery and targeted therapies
- Improved quality of life during and after treatment
- Option for patients with compromised health who cannot tolerate aggressive small intestine cancer treatments
- Prevention of recurrence, lifelong anticancer immunity after a single injection
German cancer centers have refined this approach specifically for gastrointestinal cancers, including colorectal cancer, with clinical data showing disease stabilization, reduced tumor burden, and extended survival beyond initial prognoses for some patients. Most importantly, many report significant quality of life improvements with better pain management and preserved daily function.
Hear more about this breakthrough approach in our exclusive interview with Professor Frank Gansauge, a leading expert in dendritic cell therapy for gastrointestinal cancers.
"Every Patient Deserves an Individual Approach": Interview with Renowned German Immunologist Prof. Gansauge
Minimally Invasive Approaches for Small Bowel Cancer
Advanced cancer of the small intestine treatment now includes several cutting-edge minimally invasive techniques that can destroy tumors without requiring major surgery. These approaches are especially valuable for patients with limited liver metastases or isolated tumors, offering targeted treatment with fewer complications and faster recovery times.
Heat-Based Tumor Destruction: RFA & Microwave Ablation for Small Bowel Cancer
Radiofrequency ablation (RFA) works by inserting a thin needle directly into tumors under imaging guidance, then delivering high-frequency electrical current that generates intense heat (60-100°C) to destroy cancer cells. This outpatient procedure can treat tumors up to 5cm in size in just 10-15 minutes, with most patients returning home the same day.
Microwave ablation represents the next generation of thermal treatment, using electromagnetic energy to create friction that heats and destroys cancer tissue. This approach can treat multiple tumors simultaneously and works effectively even in tissues with high water content or near blood vessels.
Key benefits include:
- Minimal recovery time compared to surgery
- Preservation of healthy surrounding tissue
- Lower complication rates than with resection
- Option for patients with compromised liver function
- Can be repeated if new tumors develop
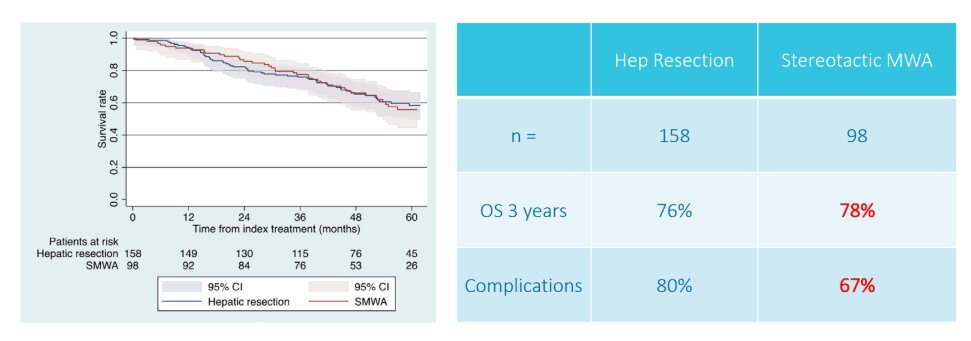
A prospective multicentre trial on survival after Microwave Ablation VErsus Resection for Resectable Colorectal liver metastases (MAVERRIC)
Freezing Cancer Cells: How Cryoablation for Small Bowel Cancer Works
Cryoablation harnesses extreme cold to destroy small bowel cancer tumors with exceptional precision. This technique creates ice crystals within cancer cells, rupturing cellular membranes and triggering natural cell death.
During the procedure, specialized probes are inserted into the tumor under imaging guidance. These probes rapidly cool to temperatures below -75°C, creating an "ice ball" that engulfs the cancer. The area is typically frozen, thawed, and refrozen to ensure complete cell destruction.
Distinct advantages of cryoablation include:
- Exceptional visibility of the treatment zone during the procedure
- Precise boundaries between treated and healthy tissue
- Minimal pain during recovery
- Effective near critical structures like blood vessels
- Treatment of tumors up to 4cm in size
- Can be performed via keyhole techniques
For small bowel cancer patients with isolated tumors or limited metastatic disease, cryoablation offers a targeted approach with minimal impact on surrounding healthy tissue.
| Characteristic | Standard Treatment | Innovative Methods |
|---|---|---|
| 2-Year Survival Rate | ~25% for advanced cancer | ~60% for advanced cancer |
| Response Rate | Less than 10% | 45-65% |
| Treatment Duration | Several cycles over months | Up to 4 sessions |
| Side Effects | Severe (nausea, fatigue, hair loss, immunosuppression, skin irritation) | Mild (localized pain) |
| Cost in Germany | €80,000 - €150,000 full course | €25,000 - €60,000 full course |
| Cost in Great Britain | €90,000 - €165,000 full course | €70,000 - €120,000 full course |
| Cost in the USA | €100,000 - €180,000 full course | €100,000 - €150,000 full course |
Booking Health data. Costs may vary based on case complexity, hospital stay duration, required follow-up care, and additional expenses such as diagnostics, travel, and accommodation.
From Diagnosis to Modern Small Bowel Cancer Treatment: A Patient's Journey
David's battle with small bowel cancer took a dramatic turn when scans revealed peritoneal carcinomatosis after his initial surgery and chemotherapy. "My oncologist told me there were limited options left," he recalls. "That's when my wife began researching specialized treatment centers abroad."
Within days of contacting an international treatment coordinator at Booking Health, David's case was reviewed by German specialists who recommended a comprehensive approach combining PIPAC with dendritic cell therapy – treatments unavailable in his home country.
"The first PIPAC procedure was remarkably straightforward compared to what I expected," David shares. "After three sessions combined with a dendritic cell vaccination, my follow-up scans showed significant tumor reduction, and my tumor markers normalized."
David has resumed many normal activities. "What impressed us most was how these innovative therapies complemented my conventional treatment while significantly reducing side effects. I've gained both quality time and renewed hope."
Advanced Cancer Treatment: Patient Success Stories with Booking Health
Regain Hope with Innovative Small Bowel Cancer Treatments
A small intestine cancer stage 4 diagnosis often comes with the devastating message that "options are limited." However, medical innovations are creating new possibilities where conventional treatments fall short.
For patients with stage 4 small intestine cancer, specialized centers worldwide now offer breakthrough approaches that can significantly improve quality of life and extend survival beyond initial prognoses. These innovative therapies include:
- Personalized dendritic cell therapy for colon cancer or small bowel cancer that trains your immune system to fight cancer cells
- Targeted PIPAC delivery that reaches peritoneal metastases with minimal side effects
- HIPEC procedures that combine surgery with heated chemotherapy
- Minimally invasive ablation techniques for treating isolated metastases
- TACE for addressing liver metastases with precision
Unlike conventional treatments that often come with debilitating side effects and lengthy hospital stays, many of these advanced therapies require just brief visits with remarkably fewer complications. While not promoted as cures, these approaches offer meaningful disease control and quality-of-life improvements for small bowel cancer stage 4 patients.
The key is connecting with specialists who stay at the forefront of these developing treatments. Don't surrender to a limited prognosis – innovative options exist that may transform your journey with stage 4 small bowel cancer.
Your Trusted Partner: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex cancer management programs in each individual case. As a reputable company, Booking Health offers personalized stage 4 small bowel cancer treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program/span>
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you on the way of pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for metastatic small bowel cancer with leading specialists in this field.
Frequently Asked Questions About Small Bowel Cancer Treatment
Send request for treatmentSmall bowel cancer is a malignant tumor that develops in the small intestine (duodenum, jejunum, and ileum). The five main types include adenocarcinoma, neuroendocrine tumors (including carcinoid), lymphoma, gastrointestinal stromal tumors, and sarcoma.
The exact cause remains unclear, but risk factors include genetic syndromes (FAP, Lynch's syndrome), Crohn's disease, celiac disease, and high alcohol intake. Chronic inflammation may trigger cell changes leading to malignant transformation in the small intestine.
Small bowel cancer is much rarer despite the small intestine comprising 90% of the GI tract. It's often diagnosed later and has different oncology treatment protocols. Small bowel cancer has a higher proportion of non-adenocarcinoma types compared to colon cancer.
Symptoms include abdominal pain, weight loss, fatigue, occult bleeding causing anemia, nausea, and vomiting. In advanced cases, intestinal obstruction may occur, causing severe pain and inability to pass gas or stool.
Diagnosis typically involves endoscopy, imaging studies like CT-scan, and tissue biopsy. For tumors in the ileum, colonoscopy with ileal intubation may be used. Some cases are diagnosed during surgery for other suspected conditions.
Small bowel cancer is rare, accounting for only 0.6% of all new cancer cases in the United States. Despite making up 90% of the GI tract's surface area, the small intestine has significantly fewer malignant tumors than the colon.
Treatment options include surgical resection, chemotherapy, radiation therapy, and innovative approaches such as HIPEC, PIPAC, TACE, and immunotherapy for advanced cases.
Surgery is the primary treatment for localized small bowel cancer, but may not be recommended for metastatic disease. In cases of intestinal obstruction, palliative surgery or stent placement might be necessary even when the cancer cannot be fully removed.
Yes, chemotherapy is commonly used both after surgery and for metastatic disease. In modern oncology, it may also be combined with novel treatment options like dendritic cell vaccination to enhance effectiveness while reducing side effects and improving quality of life.
Prognosis varies by stage, tumor type, and location. Five-year survival for early-stage disease may exceed 80%, while advanced cases with nodal involvement drop to approximately 40%. Carcinoid tumors generally have better outcomes than adenocarcinomas.
Small intestine cancer typically spreads first to regional lymph nodes, then to the liver through the portal venous system. Peritoneal metastasis is also common. Advanced imaging, like CT-scan can detect these metastases during staging.
Recovery varies by treatment. After major surgery, hospital stays average 10-14 days. PIPAC requires only 2-3 days of hospitalization. Endoscopy-based treatments often allow same-day discharge with minimal recovery time.
Five-year survival rates vary significantly: early-stage disease (80%+), node-positive (40%), and metastatic disease (11-19%). Overall survival has improved with earlier diagnosis and advanced treatment options.
Innovative treatments include HIPEC (heated intraperitoneal chemotherapy), PIPAC (pressurized chemotherapy spray), dendritic cell immunotherapy, and minimally invasive ablation techniques.
The two-year survival rate for small bowel cancer is around 25% with conventional treatment. However, innovative methods (e.g., HIPEC, PIPAC, TACE, and dendritic cell therapy) can increase survival to about 60%.
Early-stage small bowel cancer has a significantly higher survival rate, often exceeding 80%. On the other hand, advanced or metastatic stages show improved outcomes when modern therapies are added to standard care.
Traditional chemotherapy for small bowel cancer shows less than 10% response. In turn, new therapies (e.g., PIPAC and immunotherapy) reach 45-65% in suitable patients.
Standard therapy for small bowel cancer may last several months over multiple cycles. In contrast, targeted or minimally invasive methods (e.g., TACE or ablation) are typically completed within a few short sessions.
During small bowel cancer treatment, standard chemotherapy can cause fatigue, nausea, and hair loss. In comparison, modern approaches (e.g., HIPEC and immunotherapy) usually cause only mild, localized discomfort and faster recovery.
Patients with small bowel cancer receiving innovative therapies often experience fewer side effects, shorter hospital stays, and a quicker return to normal routines compared with conventional treatment.
In Germany, treatment costs range from €25,000 to €60,000 for innovative programs and up to €150,000 for standard therapy. Prices are generally higher in the UK and USA, and access to these advanced treatments in Australia is limited and often three to four times more expensive.
Management depends on tumor location, spread pattern and biology. For example peritoneal involvement may justify HIPEC or PIPAC. Liver-dominant metastases can be addressed with TACE. Dendritic cell therapy may be integrated as an adjunct to enhance tumor-specific immune activation.
Specialized gastrointestinal oncology centers with experience in rare tumors provide the most comprehensive care. German facilities (offering advanced treatment methods) ensure coordinated case-specific treatment strategies.
Countries with centralized oncology systems (particularly Germany) are preferred for rare gastrointestinal cancers. German multidisciplinary centers provide access to innovative therapies (within guideline-based frameworks) – tailored to advanced and metastatic disease.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
Read:
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
Immunotherapy for Cancer Treatment
Dendritic cell therapy in cancer treatment in Germany - Vaccination against cancer
Article menu:
- The Hidden Challenge: Understanding Small Bowel Cancer
- Foundation Treatments for Small Bowel Cancer: Surgery, Chemotherapy & Radiation
- HIPEC for Small Bowel Cancer: Cancer-Fighting Heat in the Abdominal Cavity
- PIPAC for Small Bowel Cancer: Precision Chemotherapy Through Pressurized Delivery
- TACE for Small Bowel Cancer: Targeting Tumors with Direct Chemotherapy Delivery
- Harnessing the Immune System: Dendritic Cell Therapy for Small Bowel Cancer
- Minimally Invasive Approaches for Small Bowel Cancer
- From Diagnosis to Modern Small Bowel Cancer Treatment: A Patient's Journey
- Regain Hope with Innovative Small Bowel Cancer Treatments
- Your Trusted Partner: Every Step of the Way With Booking Health
- Frequently Asked Questions About Small Bowel Cancer Treatment
Don't know where to start?
Contact Booking Health