Joint pain ranks among the most widespread musculoskeletal conditions in Europe, currently affecting over 57 million adults in Western Europe, which is more than a 50% increase since 1990. [1] Nearly 43% of these individuals are under the age of 65, which dispels the misconception that joint disorders only affect the elderly. [2] In addition, knee osteoarthritis, which is one of the most common sources of joint pain, accounts for approximately 1.28% of all years lived with disability in Europe. [3]
Traditional interventions such as physical therapy, non‑steroidal anti‑inflammatory medications, and surgery often alleviate symptoms but rarely address underlying joint degeneration. This gap in treatment efficacy has led to a growing interest in regenerative therapies.
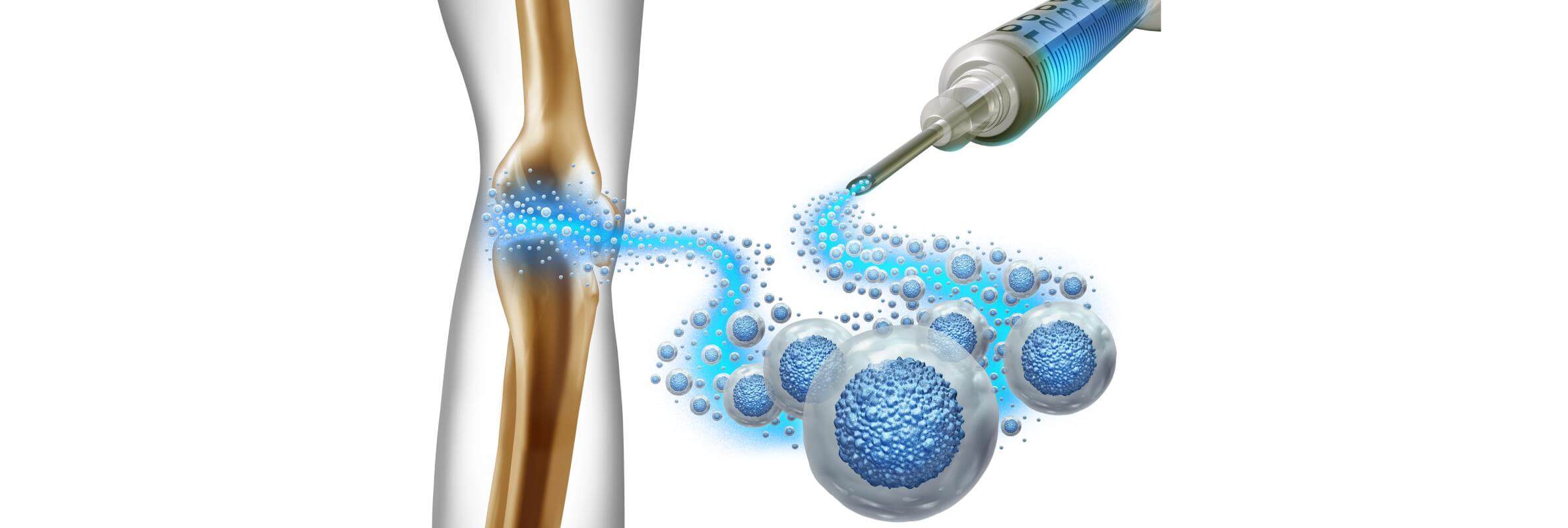
Stem cells for joint pain therapy have emerged as a promising approach, utilizing the body's own regenerative capacity to reduce inflammation, support repair, and potentially regenerate cartilage. By directly targeting tissue degeneration, it holds the potential to offer more sustained pain relief and delay, or even eliminate, the need for invasive procedures.
Unlocking Joint Renewal: Stem Cells in Action
Stem cells are undifferentiated, self-renewing cells with the remarkable ability to develop into various specialized cell types. They serve as the body's natural repair system, maintaining tissue homeostasis and facilitating regeneration after injury.
In the context of stem cell therapy for joint repair, the focus is primarily on mesenchymal stem cells (MSCs). These are adult stem cells typically harvested from bone marrow, adipose tissue, or umbilical cord tissue. Unlike embryonic stem cells, MSCs do not carry ethical concerns and are less likely to provoke immune rejection when used autologously.
This interview offers an insightful overview of how stem cell therapy is applied in real clinical practice and features a physician directly involved in this field.
"Leading German Stem Cell Expert": Dr. Siebenhüner on Modern Regenerative Medicine
How Stem Cell Therapy Works for Jonts' Pathology
MSCs (mesenchymal stem cells) are special cells that can turn into bone, cartilage, muscle, tendons, ligaments, or fat, which makes them great candidates for healing joint and orthopedic problems. But what really makes MSCs powerful is what they do once they get to the damaged tissue.
When an injury occurs, the damaged area releases signals, such as inflammatory molecules and growth factors, that act as beacons for MSCs. These stem cells sense those signals and move directly to where they're needed most. Once they arrive, MSCs don't just sit there waiting to turn into new tissue. Instead, they start releasing a mix of helpful molecules that do a lot of important jobs.
First, they calm down inflammation by sending out substances that quiet overactive immune cells and encourage the immune system to switch from a damaging, aggressive mode to a healing, peaceful one. They also protect nearby cells from dying by releasing factors that help those cells survive in the harsh environment of an injury.
On top of that, MSCs support the body's own repair crew. They release growth factors that boost blood vessel formation and encourage local repair cells to multiply and rebuild the damaged tissue. In joints, they even help the cartilage cells stop breaking down the matrix and start rebuilding it instead.
MSCs act as intelligent cellular responders at injury sites. They migrate toward inflammation, assess what local tissues need, and modulate immune responses to reduce damage. Whether it's knee joints, hip joints, facet joints, hand joints, or small, sensitive areas like the CMC joint affected by CMC joint arthritis, MSCs support regeneration and repair. Their ability to adapt to various joint environments also makes them a promising option in broader degenerative conditions like Muscular Dystrophy (Myolysis), where muscle breakdown and inflammation coexist with joint stress.
As one respected review put it:
"Mesenchymal stem cell transplantation reverts central sensitization and induces peripheral analgesia due to their anti‑inflammatory and immunomodulatory properties and by attenuation of specific pain pathways" [4]
In other words, MSC therapy doesn't just mask the symptoms. It actually tackles the pain mechanisms themselves, both centrally in the nervous system and locally in the joint. They're treating why it hurts, not just that it hurts.
Benefits of Joint Pain Stem Cell Treatment
MSCs therapy offers a regenerative approach to joint care that addresses both the symptoms and the root causes of joint degeneration. Unlike conventional treatments that primarily manage pain, MSCs actively modulate the joint environment to promote healing and long-term functional recovery.
Key advantages include:
- Pain reduction through immune modulation: MSCs release anti-inflammatory cytokines that interrupt the chronic inflammatory cycle common in osteoarthritis.
- Cartilage protection and potential regeneration: While not guaranteed, studies have shown evidence of improved cartilage integrity post-injection in some patients.
- Functional improvement: Many recipients report better mobility, decreased stiffness, and enhanced ability to perform daily tasks.
- Favorable safety profile: When harvested autologously, MSCs are well-tolerated with minimal risks of adverse immune responses.
A 2022 systematic review highlights this clinical impact:
"From the time point of view, the relief of pain by MSCs begins at most the third month after its injection, and the effective time lasts for at least 12 months." [5]
Rather than offering temporary symptom relief, MSC therapy introduces biologically active agents that can shift the trajectory of joint disease toward regeneration and repair. This approach is supported by an increasing amount of clinical evidence.
Limitations and Side Effects of Joint Pain Stem Cell Treatment
MSC-based therapy is considered safe and noninvasive. Most patients experience only mild, short-term effects such as slight swelling or temporary joint stiffness after the procedure. These typically resolve within a few days without the need for intervention.
Serious complications are exceptionally rare when treatment is performed by qualified specialists using clinical-grade protocols.
A large meta-analysis that examined over 3,500 participants across various conditions concluded:
"MSC administration was safe… no serious adverse events such as death and infection were discovered" [6]
When delivered by experienced clinicians using high-quality protocols, MSC therapy offers a low-risk alternative, free from the complications of surgery or chronic medication. This makes it an attractive, confidence-inspiring option for those seeking lasting joint relief.
| Parameter | Germany* | Great Britain | USA |
|---|---|---|---|
| Response rate | 75-85% | 70-80% | 70-85% |
| Effect duration | 12-24 months | 12-18 months | 12-24 months |
| Treatment course | Usually 1 session (outpatient) | 1-2 sessions | 1-2 sessions |
| Full course cost | €22,300 | €25,000-27,000 | €32,000-€35,000 |
*Booking Health offers individual treatment planning, so final costs may vary based on medical needs, hospital stay, and support services.
Back on Track: Elena's Journey to Pain-Free Movement with Stem Cell Treatment for Joint Pain
For Elena R., a 59-year-old teacher from Poland, knee pain from progressive osteoarthritis was making daily life harder. Walking became difficult, and even resting did not ease the swelling and stiffness. Her doctors recommended a knee replacement, but she wasn't ready for this option.
"I wanted something less invasive that could actually repair the joint," she says.
Looking for an alternative treatment for joint pain, her son found Booking Health, which helped her access advanced stem cell therapy for joints in Germany. She chose autologous stem cell therapy using her own bone marrow-derived mesenchymal stem cells.
The procedure involved a single stem cell joint injection into the affected knee joint. It was done as an outpatient visit and was quick and painless without the use of general anesthesia.
"It felt surprisingly simple," Elena recalls.
Within weeks, the inflammation and discomfort eased. By three months, she could walk long distances again and resumed light yoga. The stem cells helped restore cartilage cushioning and improved her mobility.
"I'm not just out of pain. I have my freedom back," she says. "Booking Health handled everything. I felt safe and supported throughout my entire treatment."
Elena's story shows how new joint pain treatment, like stem cell therapy for osteoarthritis, offers real hope beyond surgery. "It changed my life," she says. "And it all started with making the right decision."
Stem cells Therapy: Patient Stories with Booking Health
A New Era in Joint Pain Treatment with Stem Cells
As stem cell technology continues to evolve, it is reshaping the way we approach joint degeneration and chronic musculoskeletal conditions. For many patients, stem cell therapy for joints is more than just an innovation. It's a real alternative to invasive surgery, offering the possibility of healing rather than just symptom management. In cases like facet joint pain, where traditional options may fall short, stem cell therapy, often combined with PRP (platelet-rich plasma), is emerging as a new treatment that targets both inflammation and tissue repair at the source.
By harnessing the body's natural ability to regenerate, these therapies target the root of the problem: damaged cartilage, inflammation, and loss of mobility. Whether for the knee, hip, shoulder, elbow, or even smaller joints like the CMC joint, stem cells offer a personalized, minimally invasive solution that can significantly improve quality of life.
More and more individuals are choosing this path. The reason is not just to avoid knee replacement or long-term medication, but to reclaim their independence and return to the activities they love. The treatment is safe, performed on an outpatient basis, and uses the patient's own autologous stem cells, often combined with advanced biologics like PRP.
For those seeking an effective, science-backed, and forward-looking approach to joint pain treatment, stem cell therapy opens a door to real recovery, not just relief.
With the right guidance and access to trusted clinics, like those offered through Booking Health, this treatment becomes not just possible, but life-changing.
Regain Hope with Innovative Joint Treatments: Stem Cells
Diagnosis of advanced joint degeneration or chronic musculoskeletal pain can be frustrating and emotionally exhausting. There may be a feeling that "it is the end", and even the doctors may say that "our options are limited" or "there is little we can do". However, there is always hope, even when it seems like there is none.
Medicine is one of the most rapidly advancing fields, which means innovations appear constantly. Non-stop development of novel biologic therapies, advanced equipment (including image-guided injection systems), and new regenerative approaches is underway for the sake of preserving mobility and quality of life. Standard protocol methods, such as anti-inflammatory drugs, steroid injections, or joint replacement surgery, have been used for decades and can be effective in many cases. However, it is well-known that joints often respond less and less to these "classical" therapies. Side effects, dependency on medications, and limited long-term results often lead to a point where people stop treatment altogether. Endless physiotherapy sessions, chronic pain, or being told to "just wait until surgery is needed" can make you feel like giving up on your little progress and hope for improvement. Yet, it is exactly the moment when you can get a second wind with the help of novel treatment methods.
Stem cell therapy for joint pain, platelet-rich plasma (PRP), and other biological approaches are among the few interventions that can make a real difference for degenerative joint conditions. There is no need to spend countless days in the hospital because most of these procedures are performed on an outpatient basis with no general anesthesia and minimal recovery time. Having remarkably fewer side effects compared to standard methods, these innovative therapies demonstrate that joint treatment can be both effective and life-changing. By reducing inflammation, promoting cartilage regeneration, and restoring mobility, these advanced methods are not a miracle cure, but a powerful and science-based alternative to surgery.
Modern joint treatment techniques and specialists in regenerative orthopedics can now offer several brand-new approaches to managing chronic pain and degeneration. Do not abandon your hope for the better. Instead, explore innovations like stem cell therapy today.
Frequently Asked Questions About Stem Cell Therapy for Joints
Send request for treatmentStem cell therapy for joints involves injecting stem cells directly into the affected joint. These cells help repair damaged tissue, reduce inflammation, and promote healing, offering a promising new joint pain treatment and alternative to traditional options.
Stem cell joint injections reduce inflammation and encourage regeneration of damaged cartilage and tissue. This helps alleviate pain, improve joint function, and slow joint degeneration, making stem cell therapy for joint pain a cutting-edge option.
Stem cell treatment for joints can address osteoarthritis, rheumatoid arthritis, cartilage injuries, and facet joint pain. It's an alternative treatment for joint pain suitable for various degenerative and inflammatory joint conditions.
Yes, stem cell therapy for osteoarthritis, especially in the knee, has shown promising results in reducing pain and improving mobility by repairing cartilage and controlling inflammation, offering a new treatment for knee joint pain.
Results vary, but many patients notice improvements within weeks to months after stem cell joint injections. Healing and tissue regeneration are gradual processes, so full benefits may take up to 6 months.
Stem cell therapy is an effective method for improving symptoms and slowing joint degeneration. While it may not be a permanent solution, it significantly reduces inflammation and promotes natural repair, making it a valuable option for those looking to enhance their joint health and potentially delay the need for surgery.
Stem cell therapy for joints is generally safe with low risks. Possible side effects include mild swelling, pain at the injection site, or infection. Always consult a certified medical provider to minimize risks.
Stem cell therapy for joints in the U.S. can cost $32,000 - $35,000. In Germany, the same treatment is often more affordable, starting from €22,300, and may be partially covered by insurance, making it a cost-effective alternative with high medical standards.
Ideal candidates are patients with mild to moderate joint degeneration, osteoarthritis, or rheumatoid arthritis seeking joint pain alternative treatment who want to avoid or delay surgery.
Stem cell therapy is less invasive, with shorter recovery times and fewer risks. It aims to repair and regenerate tissue, while joint arthroplasty replaces damaged joints surgically. Both have roles depending on severity.
Yes, stem cell joint injections can be repeated depending on the patient's response and condition progression, offering a flexible option for ongoing joint repair and pain management.
Recovery is usually quick, with most patients resuming normal activities within a few days. Mild soreness or swelling may occur, but it typically resolves soon after stem cell joint injections.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Osteoarthritis in Europe. Economist Intelligence Unit. 2024. https://osteoarthritisineurope.eiu.com/infographic
[2] European Alliance of Associations for Rheumatology (EULAR). Recent advances in osteoarthritis. https://ard.eular.org/article/S0003-4967(24)14856-X/abstract
[3] Global Burden of Disease Study 2019. Prevalence and years lived with disability for knee osteoarthritis. https://pubmed.ncbi.nlm.nih.gov/37221154/
[4] Journal of Orthopaedic Surgery and Research and related biomedical sources. Various osteoarthritis studies. https://josr-online.biomedcentral.com
[5] National Library of Medicine and PMC articles on osteoarthritis. https://pubmed.ncbi.nlm.nih.gov
[6] The Lancet and Stem Cell Research biomedical articles. https://thelancet.com
Read:
Stem cell therapy and treatment in Germany
Treatment of joint diseases in Germany - effective techniques
Article menu:
- Unlocking Joint Renewal: Stem Cells in Action
- International Comparison of Stem Cell Therapy Outcomes and Costs
- Back on Track: Elena's Journey to Pain-Free Movement with Stem Cell Treatment for Joint Pain
- A New Era in Joint Pain Treatment with Stem Cells
- Regain Hope with Innovative Joint Treatments: Stem Cells
- Frequently Asked Questions About Stem Cell Therapy for Joints
Don't know where to start?
Contact Booking Health