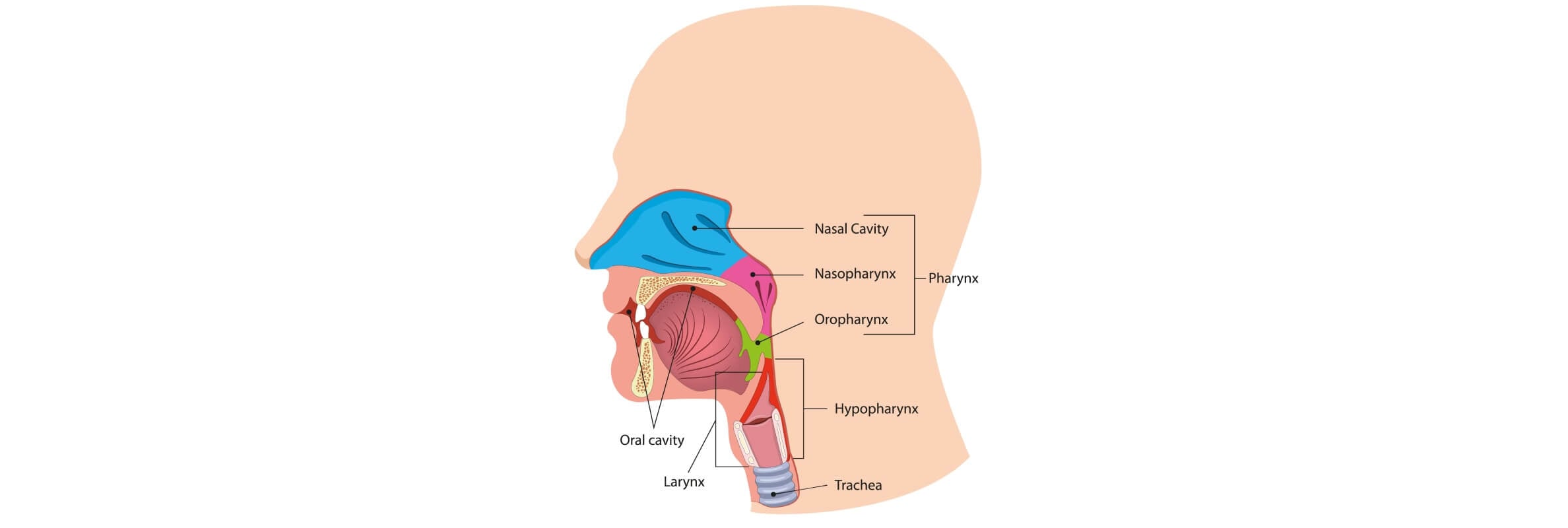
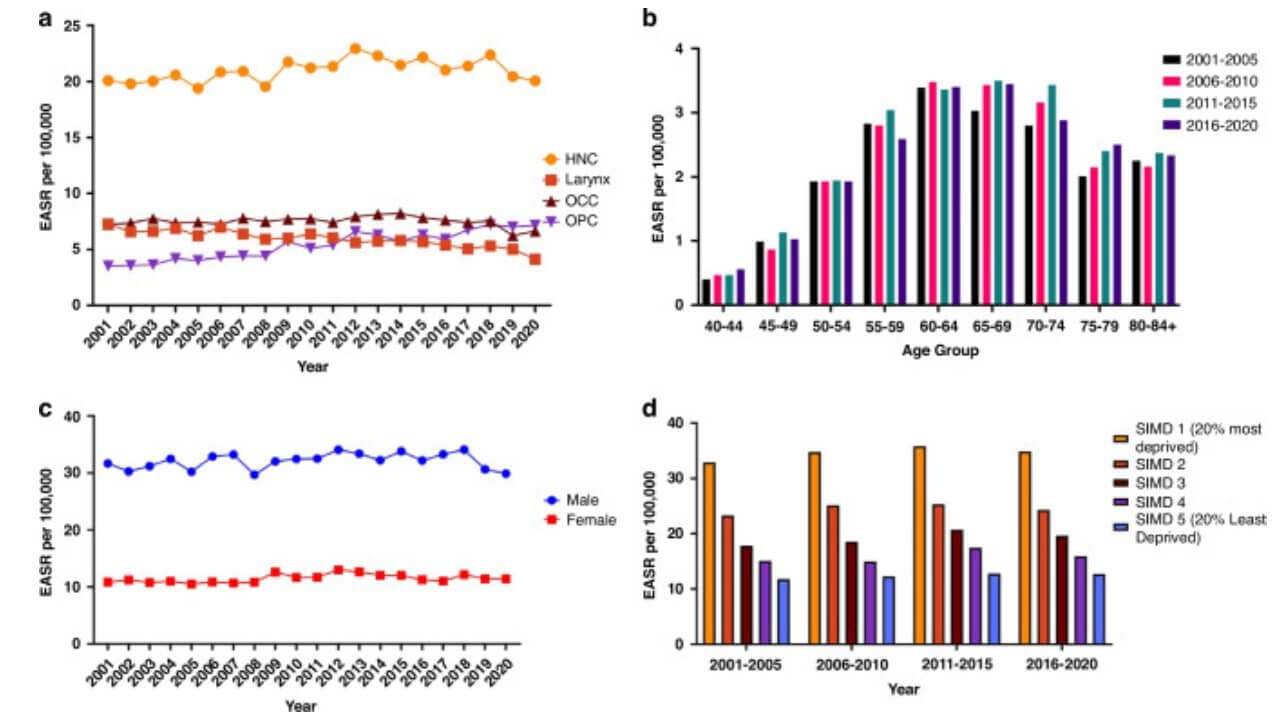
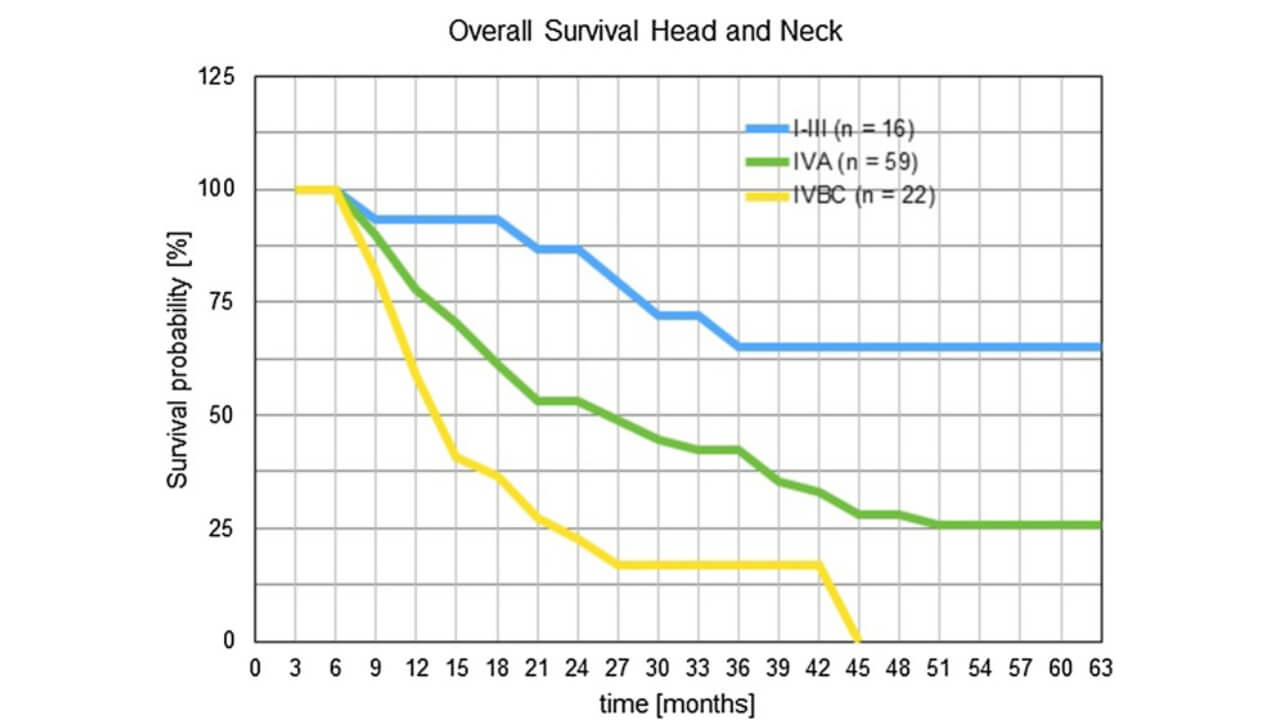
According to GLOBOCAN [1], head and neck cancers (HNC) were the sixth most common cancer in 2022, with 946,456 new cases. Head and neck cancers comprise a diverse group of malignancies that originate from the upper aerodigestive tract (cancers of the lip, oral cavity, nasal cavity, larynx, nasopharynx, oropharynx, hypopharynx and salivary glands). Among these cancers, squamous cell carcinoma is the predominant histologic type, representing more than 90% of all HNCs [2]. Its 5‐year (2005ー2014) survival rate was 87.4% at the localized stage, but it could also drop to 40.3% if the tumor had progressed into the advanced stage [3].
Radiochemotherapy (as the standard treatment for head and neck cancers) achieves a high rate of sustained complete remissions. These good clinical results, however, are partially clouded by side effects (significant aesthetic and functional deficit). After successful treatment of head and neck tumors, the side-effect-related suicide rate is the highest of all treated tumor entities [4ー7]. That is why modern oncology is actively seeking ways to localize and maximize targeted effects on cancer cells within the head and neck area. One such solution is intra-arterial regional chemotherapy ー a method that allows the drug to be injected directly into the arterial bed of the tumor, achieving high concentrations in the affected area and minimizing systemic toxicity.
Understanding Head and Neck Cancers
Head and neck cancers are a large group that affects vital functions in the head and neck area (speech, swallowing and breathing). Most head and neck cancers originate in the squamous epithelium of the mucous membranes ー squamous cell carcinomas. Early stage head and neck tumors often develop unnoticed. As it progresses, the cancer spreads to the lymph nodes and nearby structures making treatment more difficult.
Head and neck cancers involve the mouth, nose, oropharynx, larynx, trachea and salivary glands. In terms of oncology, this is one of the most heterogeneous groups, as each location has its own characteristics of growth, metastasis and response to treatment.
Main Risk Factors
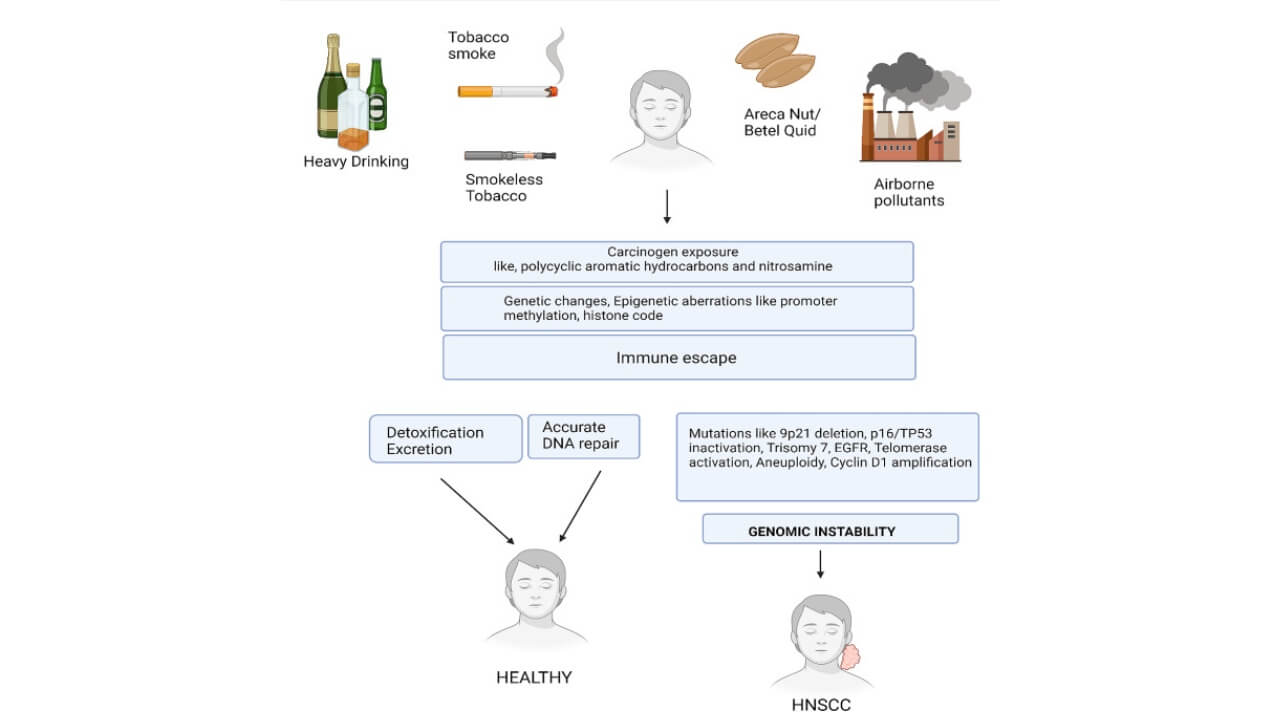
Factors that significantly increase the risk of developing head and neck cancers [9]:
- Long-term smoking and regular alcohol consumption are classic triggers for squamous cell tumors
- HPV infection
- Air pollution and industrial carcinogens
- Chronic inflammation of the mucous membranes
- Weak immune system
- Genetic predisposition
Some of the risks can be reduced through preventive measures, including the HPV vaccine.
Main Types of Head and Neck Cancers
The most common types include:
- Oral cancer
- Tongue cancer
- Tonsillar cancer
- Gum cancer
- Lip cancer
- Oropharyngeal cancer
- Nasopharyngeal cancer
- Laryngeal cancer (including vocal cord cancer)
- Tracheal cancer
- Salivary gland tumors
Each form has its own clinical characteristics, growth rate and response to treatment.
Symptoms of Head and Neck Cancers
The signs of the disease can vary significantly depending on localization:
- Oropharyngeal cancer ー foreign body sensation, difficulty swallowing, sore throat, enlarged cervical lymph nodes
- Nasopharyngeal cancer ー nasal congestion on one side, bleeding, pressure sensation in the nasopharynx and enlarged cervical nodes
- Laryngeal cancer ー hoarseness, voice change, pain when swallowing, difficulty breathing
- Salivary glands ーpainless nodes, facial asymmetry, possible facial nerve paresis
- Trachea ー stridor, cough, progressive shortness of breath
Any of these symptoms that persist for more than a few weeks requires consultation with a head and neck oncology specialist.
Diagnosis of Head and Neck Cancers
Modern oncology employs a comprehensive approach (clinical examination, biopsy, endoscopy and various imaging methods). The prevalence of head and neck cancers, especially nasopharyngeal carcinomas, emphasizes the importance of timely cancer diagnosis (in the early stages, symptoms are often mild or similar to common inflammatory processes). Early cancer diagnosis is crucial for successful treatment and improved survival.
Clinical examination and initial evaluation
The first stage of neck cancer care begins with a detailed examination of the head and neck area. The doctor assesses:
- The mucous membranes of the oral and nasal cavity
- The condition of the salivary glands
- The neck for the presence of nodes and seals
During the examination, attention is paid to changes in the voice, soreness, shortness of breath or difficulty swallowing (these symptoms may signal early head and neck cancers). The examination also includes palpation of the upper neck nodes to detect lymphadenopathy (including thyroid gland) which is often the first sign of metastasis.
Biopsy and histological examination
Biopsy is the gold standard in head and neck cancer diagnosis. The material is obtained from a suspicious area of the oral cavity, nasal cavity, larynx or salivary glands. Histological examination allows:
- To determine the type of head and neck tumor (squamous cell carcinoma, salivary gland cancer, etc.)
- To assess the aggressiveness of the tumor
- To prepare the optimal treatment plan
In cases of indeterminate results or hard-to-reach tumors, fine-needle aspiration biopsy (FNA) of the cervical nodes is used.
Endoscopic examination
Endoscopy allows doctors to examine hard-to-reach areas of the head and neck, including the oropharyngeal region, nasopharyngeal cavity, larynx, and trachea. Using an endoscope with video fixation helps:
- To assess the location and size of the tumor
- To take biopsy samples
- To plan neck surgery or a reconstructive procedure
For the early detection of nasopharyngeal cancer, endoscopy is a vital tool, especially when head and neck cancers are suspected without obvious symptoms.
Imaging: CT, MRI, PET-CT
Modern diagnostics of head and neck cancers are impossible without imaging methods:
- Computed tomography (CT) ー allows for the assessment of the size and spread of the tumor, its relationship with bone structures and lymph nodes.
- Magnetic resonance imaging (MRI) ー provides a detailed picture of the soft tissues of the head and neck area. Useful for determining the spread of head and neck tumors to the pharynx, larynx, salivary glands and neighboring structures.
- Positron emission tomography (PET-CT) ー assesses the metabolic activity of cancer cells, helps detect early metastases and second primary cancers.
The choice of a specific method depends on the localization, size of the tumor and suspicion of metastasis. A combination of CT and PET-CT is often used for the most accurate assessment of disease stage. The combination of clinical examination, biopsy, endoscopy and imaging allows for a complete treatment plan. This stage is critical for determining further head and neck cancer treatment.
Head and Neck Cancer Treatment Options
Treatment of head and neck cancers depends on the location of the tumor, its stage and the patient's general health. The goal of all methods is to fight cancer as effectively as possible while preserving healthy tissues and functions (speech, swallowing and breathing). Today, oral oncology employs an integrated approach that combines surgery, radiation treatment, systemic chemotherapy and innovative methods of local drug delivery.
Standard Treatments
Surgery remains the main treatment for oral, larynx, and salivary gland tumors especially in the early stages. Surgical treatment removes the primary cancer and regional lymph nodes which reduces the risk of recurrence. Radiation therapy is often used after surgery to destroy residual cancer cells. However, for large or difficult-to-locate tumors, surgery can be traumatic (a reconstructive procedure does not always fully restore function to the head and neck area). Patients are often left with noticeable cosmetic defects which significantly affect their psychological state, social integration and increase the risk of depression and even suicidal thoughts [10ー12].
Radiation therapy is an effective treatment method for squamous cell carcinoma. Modern technologies ー intensity-modulated radiation therapy (IMRT) ー allow for targeted therapy of head and neck tumors while sparing healthy tissue. However, with advanced disease, the effectiveness of radiation therapy is limited and side effects (damage to the mouth, larynx, and salivary glands) can be serious and long-lasting ー affecting nutrition, speech, and quality of life [10ー12].
Systemic chemotherapies destroy cancer cells throughout the body, inhibiting their division and survival mechanisms. It is effective for advanced stages (metastatic head and neck tumors), but at the same time it damages healthy tissue and weakens the immune system. Patients often experience severe intoxication, fatigue, nausea and loss of appetite, which limits the ability to use doses of drugs high enough for effective treatment. Combined with surgery and radiation therapy, these factors lead to depression, social isolation and high levels of suicidal risk among those, who have experienced significant cosmetic and functional impairment due to treatment.
Intra-arterial Regional Chemotherapy (RCT)
Intra-arterial regional chemotherapy (RCT) is an innovative method of treating malignant tumors that delivers high concentrations of drugs directly into the affected area, minimizing systemic toxicity. Compared to standard chemotherapy, RCT significantly reduces the risk of severe side effects (dysphagia, mucositis, dry skin or the need for tracheostomy or nasogastric tube) [13]. In addition, this method does not lead to horrific changes in appearance (often the case with standard treatment methods), which leads to a high suicide rate among this group of patients.
Mechanism of Action
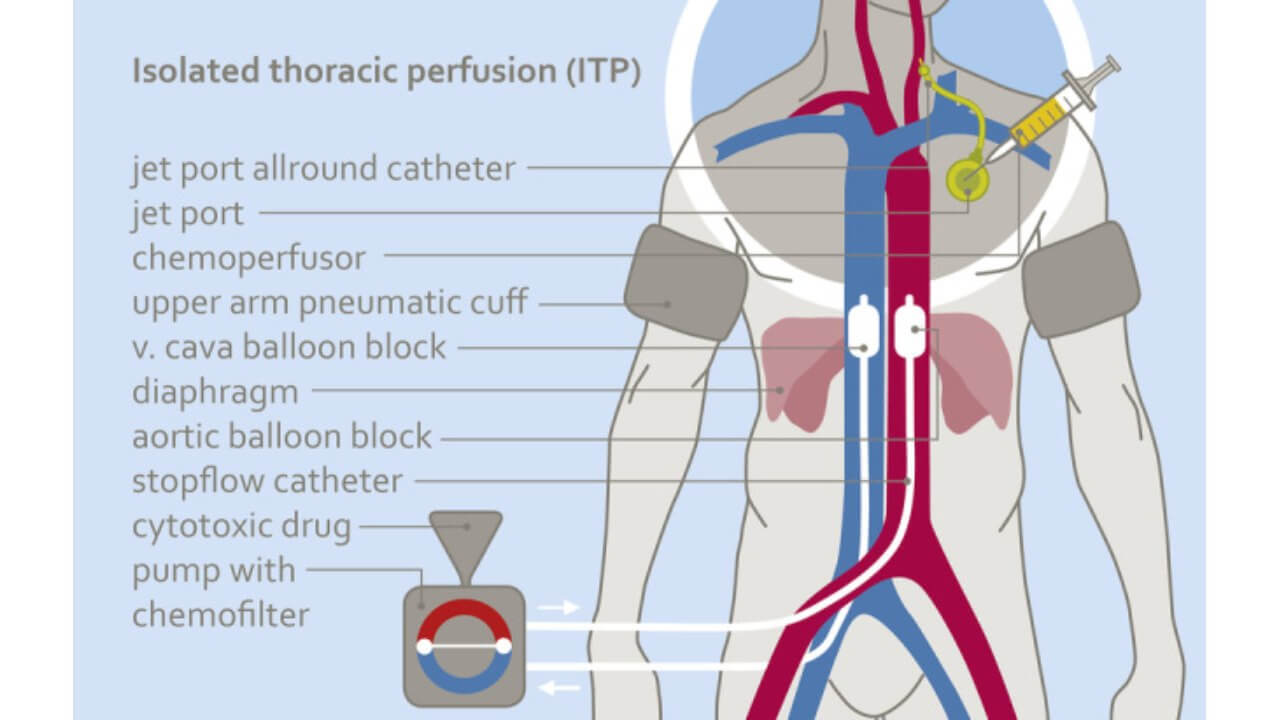
The basic idea of RCT is to deliver highly concentrated, localized infusions of chemo drugs through an arterial catheter inserted directly into the vessels supplying the tumor. To maximize the effect, isolated perfusion is used (such as isolated thoracic perfusion (ITP-F), where the catheter is equipped with balloons to block blood flow in the aorta and vena cava temporarily. This creates an isolated tumor circulation, allowing the chemo drugs to be "sealed" in the affected area for 10–15 minutes. After the infusion is complete, chemofiltration is performed to remove drug residues from the systemic circulation, reducing toxicity throughout the body [13].
Regional Chemotherapy Technique
The procedure begins with angiographic or surgical insertion of a catheter into the carotid artery or other vessels that feed the tumor. This enables the direct delivery of chemotherapy drugs to the affected area (resulting in high local concentrations of drugs).
In the case of isolated thoracic perfusion (ITP-F), a special balloon system is used to temporarily block the large vessels of the chest ー specifically the aorta and the inferior vena cava. The balloons are positioned to isolate the blood circulation in the perfusion area, allowing the chemotherapy drug to be "locked" in the tumor region for the entire time of infusion. In this case, blood from other parts of the body does not enter the isolated area, and systemic exposure to chemo remains minimal. The infusion is carried out for 5–15 minutes, providing an optimal balance between high local concentration and low systemic toxicity.
After administering the drugs, the balloons are gradually opened and blood circulation is restored. At the same time, chemofiltration is performed through a venous catheter (often inserted in the subclavian or jugular vein) which collects blood from the tumor area and filters the remains of cytostatics.
For catheterization and perfusion, modern balloon catheters are used, which enable simultaneous control of blood circulation and infusion of chemotherapy drugs. Their design provides hermetic isolation and safe delivery of medications to the desired area.
Thanks to this approach, RCT with ITP-F provides maximum drug concentration in the tumor, minimal systemic side effects and preservation of the patient's appearance and physiological functions, which is especially important in the treatment of head and neck tumors.
Advantages of RCT
- High local efficacy: drug concentration in the tumor is significantly higher
- Minimal systemic toxicity: сhemotherapy only works at the site of the tumor and does not spread throughout the body
- Preservation of quality of life and appearance: patients rarely need a tracheostomy or feeding tube; retain speech and swallowing functions; do not experience changes in appearance, which is typical for standard methods (especially for advanced stage head and neck cancers)
- Rapid clinical effect: in the absence of obstructive factors (for example, fibrosis after previous radiotherapy), the tumor may respond after the first session.
- Possibility of multiple use: the port system or catheter allows repeated cycles of chemotherapy without additional surgical interventions.
Treatment for Head and Neck Cancer Abroad
Patients with head and neck tumors often face the limitations of standard medicine in their home country. Traditional treatments (head and neck reconstructive surgery, radiotherapy and systemic chemotherapy) can be effective but are often accompanied by high toxicity, long-term side effects and the risk of functional and cosmetic impairment. That is why more and more patients are choosing to have their head and neck cancer treated abroad, where modern technologies and innovative methods are available.
Germany offers highly qualified head and neck cancer care. Head and neck cancer treatment in Germany provides the opportunity to combine standard methods with innovative ones, which enables the destruction of cancer cells (preserving healthy tissues, minimizing side effects, and improving the functions of the head and neck area). This approach significantly increases the effectiveness of head and neck cancer treatment, even with widespread or difficultly localized tumors, and gives patients a chance to restore their quality of life and social activity.
| Method | Systemic toxicity | Severe aesthetic effect | Duration | Cost of treatment |
|---|---|---|---|---|
| Regional chemotherapy | Low, no damage to healthy tissue | Absent | 2 months (completely replaces radiation, chemotherapy and surgery) | €45,000 |
| Standard treatment methods | High (especially systemic chemotherapy) | Significant aesthetic and functional deficit | up to 1 year | Up to €250,000 |
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods and with leading specialists in this field.
Cancer Treatment Abroad: Patient Experiences with Booking Health
FAQ: Comprehensive Guide to Head and Neck Cancers
Send request for treatmentThe most frequent tumor in the head and neck region is squamous cell carcinoma (arises from the lining of the oral cavity, pharynx, or larynx). Early recognition is crucial as cancer starts subtly with persistent lesions or discomfort.
Symptoms vary depending on the tumor’s location. Common head and neck cancer symptoms include persistent sores or ulcers in the oral cavity, difficulty swallowing, voice changes, neck lumps, nasal obstruction and unexplained bleeding.
Squamous cell carcinoma is the most common head and neck cancer type (linked to risk factors such as tobacco, alcohol and HPV infection). Early detection improves prognosis.
Stage 1 represents a small localized tumor without lymph node involvement. Proper head and neck cancer diagnosis at this stage allows for more effective treatment and better outcomes. Head and neck cancer starts here with subtle lesions.
Survival depends on stage, location and treatment. Early-stage tumors have a high cure rate while advanced stages require combined approaches. Outcomes improve significantly in centers specializing in modern oncology.
Many head and neck cancers are curable if detected early and treated correctly. Advanced tumors are more challenging but still treatable with multidisciplinary care.
Stage 4 is serious and often involves lymph nodes or distant spread but it is not always terminal. Treatment in Germany utilizing advanced protocols can improve survival. Cancer starts to spread more aggressively at this stage.
The oral cavity and oropharynx are the most frequent sites for head and neck tumors. Risk factors include tobacco, alcohol and exposure to human papillomavirus.
Standard head and neck cancer treatment options include surgery, radiation therapy, and chemotherapy. Innovative approaches (intra-arterial regional chemotherapy) can be used in specialized centers to target cancer cells more precisely with minimal side effects.
Treatment abroad varies by country and facility. Costs depend on access to advanced technology, specialized surgeons and comprehensive care from international clinics.
Head and neck cancer types include cancers of the oral cavity, oropharynx, nasopharynx, larynx, thyroid gland, salivary glands, and sinonasal regions. The risk factors include tobacco use, alcohol consumption, and human papillomavirus infection.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Freddie Bray, Mathieu Laversanne, Hyuna Sung et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024 May-Jun;74(3):229-263. doi: 10.3322/caac.21834. Epub 2024 Apr 4. [DOI] [PubMed]
[2] John Mendelsohn, Peter M. Howley, Mark A. Israel, Joe W. Gray, Craig B. Thompson. The Molecular Basis of Cancer
[3] Kangwen Guo, Weiliang Xiao, Xinggui Chen, Zhenying Zhao, Yuanxiong Lin, Ge Chen. Epidemiological Trends of Head and Neck Cancer: A Population-Based Study. Biomed Res Int. 2021 Jul 14;2021:1738932. doi: 10.1155/2021/1738932. [DOI] [PMC free article]
[4] Nosayaba Osazuwa-Peters, Eric Adjei Boakye, Ronald J Walker, Mark A Varvares. Suicide: A Major Threat to Head and Neck Cancer Survivorship. J Clin Oncol. 2016 Apr 1;34(10):1151. doi: 10.1200/JCO.2015.65.4673. [DOI] [PubMed]
[5] Stephanie Misono, Noel S Weiss, Jesse R Fann, Mary Redman, Bevan Yueh et al. Incidence of suicide in persons with cancer. J Clin Oncol. 2008 Oct 10;26(29):4731-8. doi: 10.1200/JCO.2007.13.8941. Epub 2008 Aug 11. [DOI] [PubMed]
See more
[6] Linda Anguiano, Deborah K Mayer, Mary Lynn Piven, Donald Rosenstein. A literature review of suicide in cancer patients. Cancer Nurs. 2012 Jul-Aug;35(4):E14-26. doi: 10.1097/NCC.0b013e31822fc76c. [DOI] [PubMed]
[7] Joshua Briscoe, Jason A Webb. Scratching the Surface of Suicide in Head and Neck Cancer. JAMA Otolaryngol Head Neck Surg. 2016 Jun 1;142(6):610. doi: 10.1001/jamaoto.2016.0255. [DOI] [PubMed]
[8] Craig D L Smith, Alex D McMahon, Mitana Purkayastha et al. Head and neck cancer incidence is rising but the sociodemographic profile is unchanging: a population epidemiological study (2001–2020). BJC Rep. 2024 Sep 17;2:71. doi: 10.1038/s44276-024-00089-z. [DOI] [PMC free article]
[9] Nicholas S Mastronikolis, Alexander Delides, Efthymios Kyrodimos et al. Insights into metastatic roadmap of head and neck cancer squamous cell carcinoma based on clinical, histopathological and molecular profiles. Mol Biol Rep. 2024 Apr 29;51(1):597. doi: 10.1007/s11033-024-09476-8. [DOI] [PMC free article]
[10] Shrinivas Rathod, Jonathan Livergant, Jonathan Klein, Ian Witterick, Jolie Ringash. A systematic review of quality of life in head and neck cancer treated with surgery with or without adjuvant treatment. Oral Oncol. 2015 Oct;51(10):888-900. doi: 10.1016/j.oraloncology.2015.07.002. Epub 2015 Jul 21. [DOI] [PubMed]
[11] Jolie Ringash. Survivorship and Quality of Life in Head and Neck Cancer. J Clin Oncol. 2015 Oct 10;33(29):3322-7. doi: 10.1200/JCO.2015.61.4115. [DOI] [PubMed]
[12] Jolie Ringash, Lori J Bernstein, David Cella et al. Outcomes toolbox for head and neck cancer research. Head Neck. 2015 Mar;37(3):425-39. doi: 10.1002/hed.23561. Epub 2015 Jan 22. [DOI]
[13] Karl R Aigner, Emir Selak, Kornelia Aigner. Short-term intra-arterial infusion chemotherapy for head and neck cancer patients maintaining quality of life. J Cancer Res Clin Oncol. 2018 Oct 31;145(1):261–268. doi: 10.1007/s00432-018-2784-4. [DOI]
Read:
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
Immunotherapy for Cancer Treatment
Dendritic cell therapy in cancer treatment in Germany - Vaccination against cancer
Article menu:
Don't know where to start?
Contact Booking Health