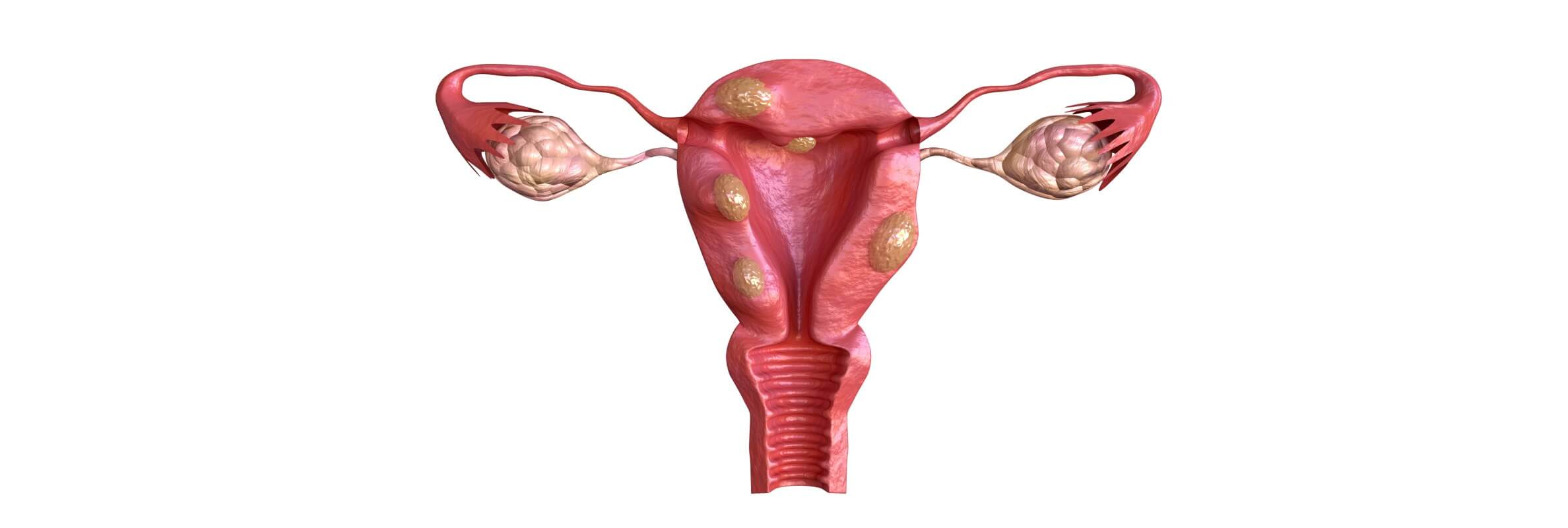
Uterine fibroids, or myomas, develop from the muscle layer of the uterus and the surrounding fibrous tissue. The pathology influences women of reproductive age, as its main cause is a high estradiol level. When elaborating the therapeutic regimen, doctors always consider the desire of a woman to have children in the future. Thus, therapeutic measures offered by specialized healthcare institutions may include pharmacotherapy and minimally invasive or open surgical interventions. Qualitative rehabilitation and relapse prevention also contribute to the improvement of a woman’s health state and ability to conceive and endure pregnancy in the future.
Content
- Clinical symptoms and possible complications
- Diagnostics and choosing the therapeutic regimen
- Non-surgical treatment options
- Surgeries and minimally invasive interventions
- Planning pregnancy with uterine fibroids
- Preventing the relapse of uterine fibroids
- World’s leading gynecology hospitals
- Treatment of uterine myoma with Booking Health
Clinical symptoms and possible complications
Appearing more frequently in women of African Caribbean origin, uterine fibroids affect around 1 out of 3 women aged 30 to 50. In most cases the pathology does not affect the quality of life or even manifest itself with any symptoms. Those women who have clinical manifestations may experience:
- heavy or painful periods, colicky abdominal pains during periods;
- mild to severe abdominal or lower back pain between periods;
- dyspareunia (discomfort or pain during sexual intercourse);
- frequent painful urination without obvious cause;
- constipation;
- general weakness, tiredness, and impaired concentration due to anemia;
- fertility and pregnancy problems;
- swelling of the lower abdomen (in large myomas).
Nevertheless, even asymptomatic fibroids are associated with a risk of miscarriage or premature labor. Visiting a specialist in gynecology is an obligatory part of annual check-ups in women of a reproductive age. Suspecting a nodular pathology of the womb, a doctor refers a woman for a set of diagnostic procedures. Timely diagnosis making is important, as myomas always continue growing until the menopause, when estradiol levels fall.
Diagnostics and choosing the therapeutic regimen
Clinically unsuspected fibroids are typically diagnosed during a routine pelvic examination (e.g. pelvic ultrasound). In other cases, the pathology is revealed with the help of targeted visualizing studies.
Ultrasound scan is a painless examination that uses high frequency sound waves to create an image of the internal organs. During an abdominal ultrasound examination, the ultrasound probe is placed on the lower abdomen. During a transvaginal ultrasound examination, another special probe is inserted inside the vagina. The images produced by the probe are immediately transmitted to the monitor. Thus, the doctor sees a real time picture of the uterus. An ultrasound scan may be supplemented by a Doppler scan for an assessment of the blood flow in the uterine arteries.
MRI is a noninvasive visualizing procedure that gives more detailed images of the uterus and nearby tissues. Based on the MRI results, a doctor can determine the quantity and size of the myomas.
Hysteroscopy is a more invasive procedure that implies the direct examination of the inner lining of the womb. The endoscope reaches the womb through the vagina. By using modern miniature equipment, this does not require any incisions to be made or anesthesia to be used. The whole procedure takes about 5-10 minutes. A hysteroscopy is helpful in detecting and treating submucosal fibroids.
Laparoscopy is a diagnostic surgery that is performed through small incisions in the abdomen. The endoscope, with a camera and light source, is passed inside and relays images of the outer surface of the womb and nearby organs to a monitor. As a laparoscopy is more invasive compared to a hysteroscopy, this intervention is performed under general anesthesia, i.e. the woman stays asleep during the whole procedure. A laparoscopy is informative for subserosal and intramural myomas.
Biopsy is typically performed during a hysteroscopy or laparoscopy. This involves harvesting small tissue samples, which are examined under a microscope. A biopsy is performed in unclear cases, when it is important to reveal the exact type of neoplasm in the uterus.
Instrumental studies are always supported by laboratory tests, including a complete blood count and blood coagulation test. This allows for preventing and timely treating anemia or coagulopathies.
Non-surgical treatment options
The etiological role of female steroid hormones in the development of uterine fibroids, is supported by the experimental, epidemiological, and clinical evidence. Thus, medications aimed at blocking the action of progesterone and estradiol are the first-line non-surgical treatments for patients of reproductive age. These include:
- Selective estradiol receptor modulators (SERM). Estradiol increases the availability of progesterone receptors and thus, potentiates the biological action of this hormone. Progesterone stimulates myoma development and the proliferation of its cells. Three SERMs are available now: tamoxifen (Nolvadex and Soltamox), raloxifene (Evista), and toremifene (Farestone).
- Selective progesterone receptor modulators (SPRMs) directly block the biological effects of progesterone. The hormone is still produced by the ovaries and adrenal glands, but cannot influence the uterus anymore. SPRM ulipristal acetate is now licensed for preoperative myomas treatment. Use of the drug for long-term disease management is still under research. Other SPRMs, such as mifepristone and asoprisnil, are used less often and demonstrate poor efficiency.
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists. GnRH agonists suppress ovaries and make them produce less progesterone and estradiol. In addition, they stop the menstrual cycle and thus, reduce blood loss and increase hemoglobin levels. GnRH antagonists suppress the pituitary gland, which controls the ovarian function, so the ovaries stop producing both progesterone and estradiol.
Other options of hormonal treatment are to take oral contraceptives or use a levonorgestrel intrauterine system. Birth control pills reduce bleeding during periods and alleviate pain. A levonorgestrel intrauterine system is also a contraceptive agent, but it can additionally stop the growth of myomatous nodes. Symptomatic treatments are also used. These include nonsteroidal anti-inflammatory drugs (NSAIDs) for reducing pain and iron preparations for restoring hemoglobin levels.
Surgeries and minimally invasive interventions
Surgery comes to the fore with the presence of secondary changes in the fibroid (e.g. necrosis or infection), rapid growth (adding 4-5 weeks of pregnancy per year), and a large size (12-14 week pregnancy), severe pain, uterine bleedings, infertility or repeated miscarriages, and dysfunction of the neighboring organs (e.g. bladder or intestine). Depending on the size and localization of the myoma in the uterine wall, the following techniques may be applied:
- Hysterectomy is a partial or total womb removal. This approach is suitable for large fibroids or fibroids that cause excessive bleeding. When possible, the surgeon preserves the ovaries and prevents early menopause and libido reduction.
- Myomectomy is removing only the fibroid that is located in the muscular layer of the uterus. Laparoscopic myomectomy of uterine fibroids is a sparing procedure that does not require opening the abdomen, as the surgical equipment is inserted through small incisions in the abdominal wall. Nevertheless, women with myomas that are located in certain parts of the uterus may need an open (abdominal) myomectomy. An open myomectomy provides better visualization and is more convenient for a surgeon.
- Organ-preserving robotic myomectomy with the da Vinci system. The modern da Vinci robot surgeon has 7 degrees of freedom and 2 degrees of axial rotation, which exceeds the usual surgeon’s abilities during an intervention. With the help of one of the robot arms, the surgeon controls the camera and obtains clear images of the operating field, the second and third robot arms imitate the surgeon's right and left hands, and the fourth one serves for additional manipulations, increasing the accuracy of the intervention. The use of the da Vinci robot allows the surgeon to see structures that are invisible to the naked eye, preserve the blood vessels of the uterus, make the postoperative period easier, and achieve an excellent cosmetic result.
- Hysteroscopic resection of fibroids is performed without cutting the abdominal wall, as surgical instruments are inserted through the vagina. Hysteroscopes relay images of the operative field to a monitor and the surgeon cuts the myoma with miniature surgical instruments under excellent visual control. Few insertions may be required to remove the fibroid tissue completely. The procedure is painless, as it is performed under general anesthetic.
- Hysteroscopic morcellation of fibroids is somewhat similar to a hysteroscopic resection, except that the surgical instruments are only inserted once. This reduces the risk of a uterus injury. The morcellator repeatedly cuts away and removes the fibroid tissue until the uterine wall becomes normal. The procedure requires general or spinal anesthetic.
- Endometrial ablation is removing the endometrium, which is the inner womb layer, with the help of temperature or radio waves (cryoablation, thermal balloon ablation, radiofrequency ablation). With endometrium removal, periods become less heavy. This significantly improves the clinical course of fibroids-caused anemia. Endometrial ablation is efficient in submucosal (i.e. superficial) myomas.
- Uterine artery embolization is a more sparing alternative to a myomectomy or even hysterectomy. Blocking the uterine artery with an embolus is performed under guidance of fluoroscopic X-ray imaging. An embolus reduces the blood supply of the uterus and thus, fibroids. This leads to the myoma shrinking.
- Uterine fibroid embolization is similar to uterine artery embolization, except it doesn’t block the entire uterine artery but its smaller branch, which feeds the neoplasm. Both procedures are carried out under local anesthetic.
- MRI-guided percutaneous laser ablation. First, the precise localization of the fibroid is determined with the help of an MRI scan. After that, a doctor reaches the targeted neoplasm with fine needles that are inserted through the skin, under visual guidance. The needles serve as the guide for the laser fiber device, which sends out laser light and destroys the myoma.
- MRI-guided focused ultrasound surgery is somewhat similar to the previous procedure, but it uses high energy ultrasound waves instead of laser light. The intervention is relatively new, its benefits and possible risks are still to be investigated.
The choice of treatment tactic depends to a large extent on a woman’s reproductive potential. In certain patients, surgery may even be postponed in order to not ruin their reproductive plans.
Planning pregnancy with uterine fibroids
In women of reproductive age, special consideration is given to preserving their childbearing potential. A doctor discusses two questions with a woman:
- How may the fibroid influence fertility and pregnancy? Does it require obligatory treatment?
- If treatment must be performed, then which technique will ensure the best long-term outcomes with regard to fertility and general health?
Small fibroids that are completely embedded in the wall of the womb (i.e. intramural nodules) and do not affect the inner lining of the uterus (endometrium) are not a significant obstacle to conceiving a child. In this case, it may be more beneficial to plan pregnancy as is, against the background of pharmacological support. Invasive surgical treatment may be postponed, as the postoperative rehabilitation period lasts for 6 months or longer.
In other cases, due to the size and localization, a myoma may affect a sperm’s ability to reach the egg or interfere with the implantation of an embryo or placentation. Thus, women with large fibroids located inside the womb (i.e. submucous fibroids) are eligible for surgery. Not all types of surgical procedures are suitable for women who want to preserve their fertility. A myomectomy, MRI-guided percutaneous laser ablation, MRI-guided focused ultrasound surgery, hysteroscopic resection, or morcellation of fibroids may be considered. Some women may need to deliver a baby via cesarean section, since the uterus does not recover completely after the intervention. In addition, doctors pay special attention to postoperative relapse prevention.
Preventing the relapse of uterine fibroids
When a woman is not concerned about preserving fertility, a doctor may carry out radical treatment as an ultimate secondary disease prevention measure. This includes performing a partial or total uterus resection (hysterectomy) or endometrial ablation (a minor procedure that removes the inner layer of the uterus). During other interventions, a surgeon tries to remove the fibroid completely, as its residual mass tends to grow and form a new fibroid.
In other cases, controlling the estradiol levels comes to the fore. A uterine myoma is a hormone-dependent neoplasm. It has been proven that estradiol stimulates both disease development and progression. Thus, maintaining low estradiol levels improves the long-term prognosis and lowers the postoperative recurrence rate. The most efficacious measures include the following:
- Maintaining normal body mass. Excessive body mass and obesity stimulate estradiol synthesis, as this hormone is produced not only by the ovaries, but also by the adipose tissue.
- Choosing a healthy lifestyle with a high content of fruits and vegetables in their diet.
- Taking birth control pills. In addition to controlling estradiol levels, hormonal contraceptives positively influence the menstrual cycle regularity and increase the chances of conceiving a baby after their withdrawal (the rebound effect).
- Controlling arterial hypertension. The connection between blood pressure and myoma development is not yet clear, but the research shows that a lot of women with large fibroids are also diagnosed with arterial hypertension.
- Receiving enough vitamin D.
World’s leading gynecology hospitals
A high estimated prevalence of uterine myomas, as well as significant direct and indirect costs associated with diagnosis making and treatment, are substantial factors for both healthcare providers and patients. Choosing a well-equipped hospital and an experienced surgeon is more cost-effective, as it improves the precision of diagnostics, reduces treatment-dependent complications, and leads to better outcomes. German healthcare institutions offer a full range of medical interventions, including all types of surgeries and follow-up diagnostic procedures. German specialists are experienced in the treatment of special patient populations, such as women of a reproductive age who want to preserve their fertility and women with asymptomatic neoplasms.
The list of the best hospitals in Germany includes, but is not limited to:
- University Hospital Rechts der Isar Munich, Department of Gynecology, Mammalogy, Obstetrics, and Perinatal Medicine
- University Hospital Tuebingen, Department of Adult and Pediatric Gynecology, Mammalogy, and Obstetrics
- Charite University Hospital Berlin, Department of Adult and Pediatric Gynecology and Mammalogy
- University Hospital Ulm, Department of Obstetrics, Adult and Pediatric Gynecology
- University Hospital Carl Gustav Carus Dresden, Department of Adult and Pediatric Gynecology, Mammalogy, and Obstetrics
In addition, Charite University Hospital in Berlin is included in the ranking of the world's best healthcare institutions, developed by Statista Inc. (the authoritative global medical market research and consumer data company) in 2019. The estimation considered medical key performance indicators, recommendations of the healthcare professionals, and results of independent patient surveys. According to the results, Germany was included in the first edition of ranking.
Treatment of uterine myoma with Booking Health
Choosing a hospital beyond the borders of their native country, means patients and their relatives face a number of organizational issues. Without experience of receiving treatment abroad, it may be difficult to take into account all the peculiarities of a foreign healthcare system. So that everything goes easily and safely, it is better to use the assistance of Booking Health. The Booking Health company is the international provider of medical tourism.
Having been engaged in the arrangement of uterine fibroids treatment abroad for over 15 years, Booking Health provides all-inclusive help to women and their relatives:
- help make your choice from the specialized clinics, based on the rating and the annual qualification profile;
- establishing communication with the chosen gynecologist and surgeon;
- elaborating the preliminary treatment program in advance, explaining all its stages;
- providing a favorable cost for treatment, without additional fees for foreign patients or overpricing (saving up to 50%);
- booking the appointment or room in the chosen department;
- monitoring the medical program at all its stages;
- insurance against the cost of treatment increase in case of complications (а coverage of €200,000, valid for 4 years);
- assistance with buying and forwarding of medications;
- communication with the hospital after the treatment’s completion;
- organization of additional procedures, follow-up tests, and rehabilitation;
- control of medical bills and return of unspent funds;
- service of the highest level: booking hotels and plane tickets, organization of transfers.
To start planning a medical trip, leave your request on the Booking Health website. A patient case manager or medical advisor will call you as soon as possible to discuss the details of your case. After choosing the hospital, doctor, and medical program, a personal medical coordinator will stay in touch with you 24/7, which is extremely helpful while you’re abroad.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
National Center for Biotechnology
Read:
Don't know where to start?
Contact Booking Health