Neuroendocrine tumors (NETs) have become significantly more common over the past two decades. Between 2000 and 2018, the age-adjusted incidence rose from 4.9 to 8.2 cases per 100,000 people, with the sharpest increases seen in grade 1 tumors, early-stage cases, and tumors of the appendix [1]. Alarmingly, the mortality rate grew more than threefold during the same period, despite better diagnostic tools.
Understanding Neuroendocrine Tumors
Although neuroendocrine tumors (NETs) are relatively rare compared to other cancers, their complexity makes them a distinct and challenging group of diseases. They can behave very differently depending on where they originate, how aggressive they are, and how early they’re detected. Understanding the basic features of these cancers is crucial for proper diagnosis and treatment.
Understanding How NETs Develop
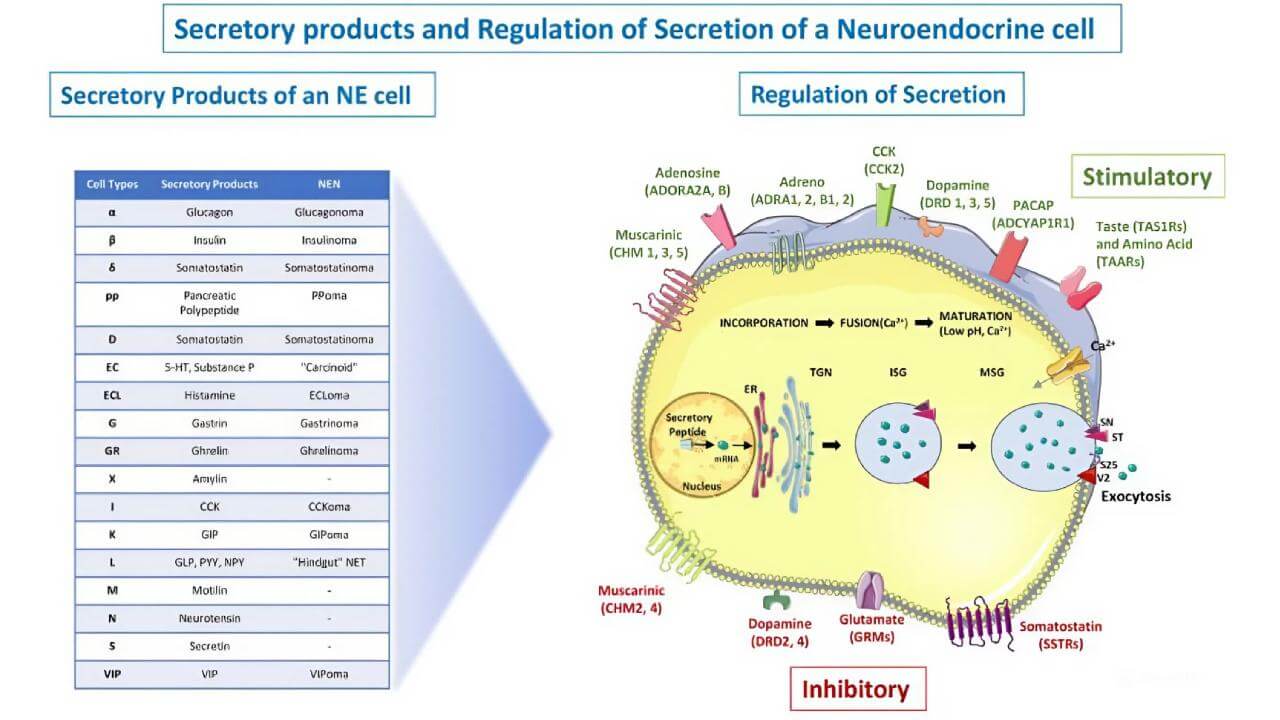
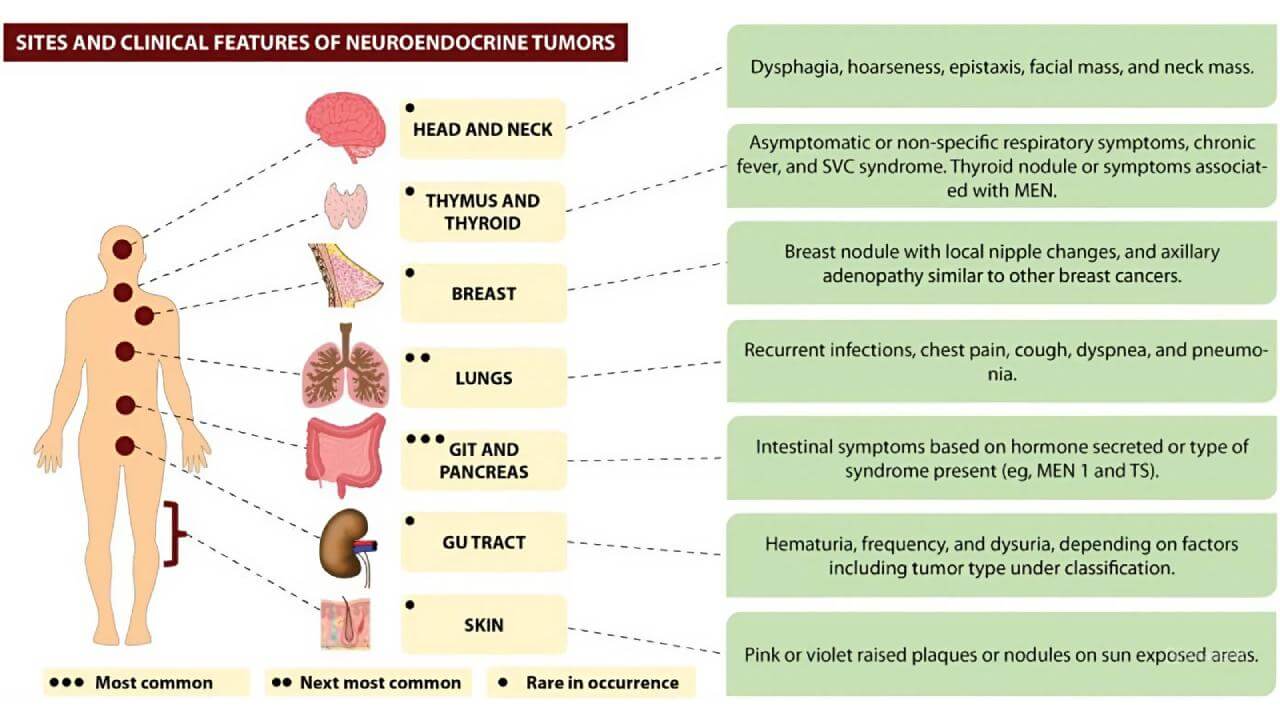
Neuroendocrine tumors arise from cells that have traits of both nerve and hormone-producing cells. These cells are scattered throughout the body, which is why NETs can occur in a variety of organs. What makes them unique is their ability to release hormones or hormone-like substances, sometimes causing distinct clinical syndromes.
Common Causes and Risk Factors of Neuroendocrine Tumors
In most cases, the exact cause of NETs is unknown. However, available information suggests that certain genetic conditions, such as multiple endocrine neoplasia type 1 (MEN1), can increase the risk. Other potential factors include chronic inflammation in the digestive tract, smoking (especially for lung NETs), and a family history of similar tumors. Still, many people develop NETs without any clear risk factors.
Symptoms of Neuroendocrine Tumors to Watch For
Symptoms of NETs vary widely depending on the tumor’s location and whether it produces hormones. Some tumors grow silently for years, while others cause noticeable signs early on. Common symptoms may include abdominal pain, changes in bowel habits, flushing, wheezing, unexplained weight loss, or fatigue. Hormone-secreting cancers can trigger syndromes like carcinoid syndrome, which includes diarrhea, skin flushing, and heart valve issues.
How NETs Are Classified
Neuroendocrine cancers are classified based on two main things: how much the tumor cells look like normal cells (this is called differentiation) and how quickly they’re dividing. Both factors help doctors understand how aggressive the tumor might be and choose the right treatment strategy.
The World Health Organization (WHO) divides NETs into three grades, depending on how fast the cells are growing [3]. This is measured by two markers:
- The mitotic rate – how many cells are dividing under the microscope
- The Ki‑67 index – a lab test that shows how many cells are in the active phase of growth
Here's a simplified breakdown:
- Grade 1 (G1): These are slow-growing tumors. Under the microscope, fewer than 2 cells per 10 high-power fields are dividing, and the Ki‑67 is below 3%.
- Grade 2 (G2): These tumors are more active, with 2 to 20 dividing cells and a Ki‑67 between 3% and 20%.
- Grade 3 (G3): These are fast-growing and potentially more aggressive tumors, with over 20 mitoses and Ki‑67 above 20%.
Most G1 and G2 tumors are called well-differentiated NETs and tend to grow more slowly. G3 tumors, on the other hand, are usually poorly differentiated and referred to as neuroendocrine carcinomas (NECs) - a more aggressive form.
Diagnostic Methods of NETs
Diagnosing NETs requires a combination of laboratory tests and advanced imaging techniques. Because these tumors can behave in unpredictable ways and often grow slowly, it’s essential to use multiple tools to detect them early, assess their activity, and guide treatment. In Germany, diagnostic protocols are comprehensive and include both standard and highly specialized tests.
Blood Tests and Tumor Markers of Neuroendocrine Tumors
A routine blood test is usually the first step. Doctors check for general indicators of health, including complete blood count and liver and kidney function, since NETs can sometimes affect these systems.
More specifically, several tumor markers are commonly measured:
- Chromogranin A (CgA) is the most frequently used NET marker
- Neuron-specific enolase (NSE) may be elevated in high-grade or poorly differentiated tumors
- Pancreatic polypeptide, gastrin, and serotonin metabolites (such as 5-HIAA) can also be helpful, depending on the tumor type
These markers aren’t always specific, but can be useful for monitoring treatment response and tracking disease progression.
Hormonal Testing in Neuroendocrine Tumors
For functioning NETs, which produce excess hormones, hormonal assays are key. Depending on symptoms and tumor location, doctors may measure:
- Serotonin and 5-HIAA (in urine or plasma), especially in carcinoid syndrome
- Insulin, gastrin, VIP, or somatostatin for pancreatic NETs
- ACTH or cortisol for adrenal-related NETs
These tests help identify hormone-secreting tumors and monitor the effectiveness of treatment.
Imaging Techniques for Neuroendocrine Tumors: CT, MRI, PET-CT
Imaging plays a central role in both diagnosis and staging [4].
- Contrast-enhanced CT scans are often the first-line imaging tool to detect the size, location, and spread of NETs
- MRI is especially useful for liver metastases and pancreatic NETs due to its higher soft-tissue resolution
- PET-CT is a highly sensitive imaging modality that detects tumors expressing somatostatin receptors. It’s now considered the gold standard in many cases
- FDG PET-CT may be used in high-grade or rapidly growing tumors where somatostatin receptor imaging is less effective
Combining these modalities helps build a complete picture of the disease.
Biopsy and Pathological Confirmation in Neuroendocrine Tumors
To make a definitive diagnosis, a biopsy is essential. Tissue samples are examined to confirm the presence of neuroendocrine cells, assess tumor grade, and calculate the Ki-67 index, which indicates how fast the tumor is growing. This information is crucial for staging and selecting the right treatment.
Standard Treatment Options for Neuroendocrine Tumors
Neuroendocrine tumors (NETs) vary widely in their behavior, so treatment must be tailored to the tumor’s location, grade, stage, and whether it produces hormones. In Germany, standard treatment protocols are well-established and focus on controlling the disease, relieving symptoms, and improving long-term survival.
Surgery to Remove The Neuroendocrine Tumor
Surgery remains the first-line treatment for many patients with neuroendocrine tumors, especially those detected early. In well-differentiated, low-grade tumors, complete surgical removal can be curative.
Procedures range from minimally invasive laparoscopic surgery to more extensive resections, depending on tumor size and spread. In some cases, even metastatic NETs may be partially removed to reduce tumor burden and improve quality of life.
For patients with appendiceal NETs or small tumors in the small intestine or pancreas, surgery is often the best option with curative potential.
Radiation Therapy for Neuroendocrine Tumors
Radiotherapy is not routinely used for most well-differentiated NETs, as they tend to be less sensitive to standard radiation. However, in high-grade neuroendocrine carcinomas (NECs), or when tumors are causing local symptoms such as pain or bleeding, targeted radiation can provide effective control.
Chemotherapy For Aggressive or Advanced Neuroendocrine Tumors
Chemotherapy is typically reserved for poorly differentiated, high-grade NETs or when the disease is advanced and rapidly progressing.
In some cases of well-differentiated but progressive NETs, chemotherapy may still be considered, particularly if targeted therapies are not effective. Treatment choice depends on tumor biology, patient condition, and prior therapy response.
Advanced and Innovative Therapies for Neuroendocrine Tumors
Standard treatment isn’t always enough for patients with advanced or complex neuroendocrine tumors. That’s why Germany has become a leading destination for cutting-edge therapies that offer new hope when traditional methods fall short.
Peptide Receptor Radionuclide Therapy (PRRT) for Neuroendocrine Tumors
Peptide Receptor Radionuclide Therapy (PRRT) is one of the most promising treatments for patients with well-differentiated, metastatic NETs. It works by delivering a radioactive isotope—Lutetium-177—directly to tumor cells through a molecule that binds to somatostatin receptors, which are highly expressed in many NETs.
Unlike traditional radiation, Lutetium targets cancer cells only, minimizing damage to healthy tissues. It not only helps reduce tumor size but can also control symptoms and delay disease progression for years.
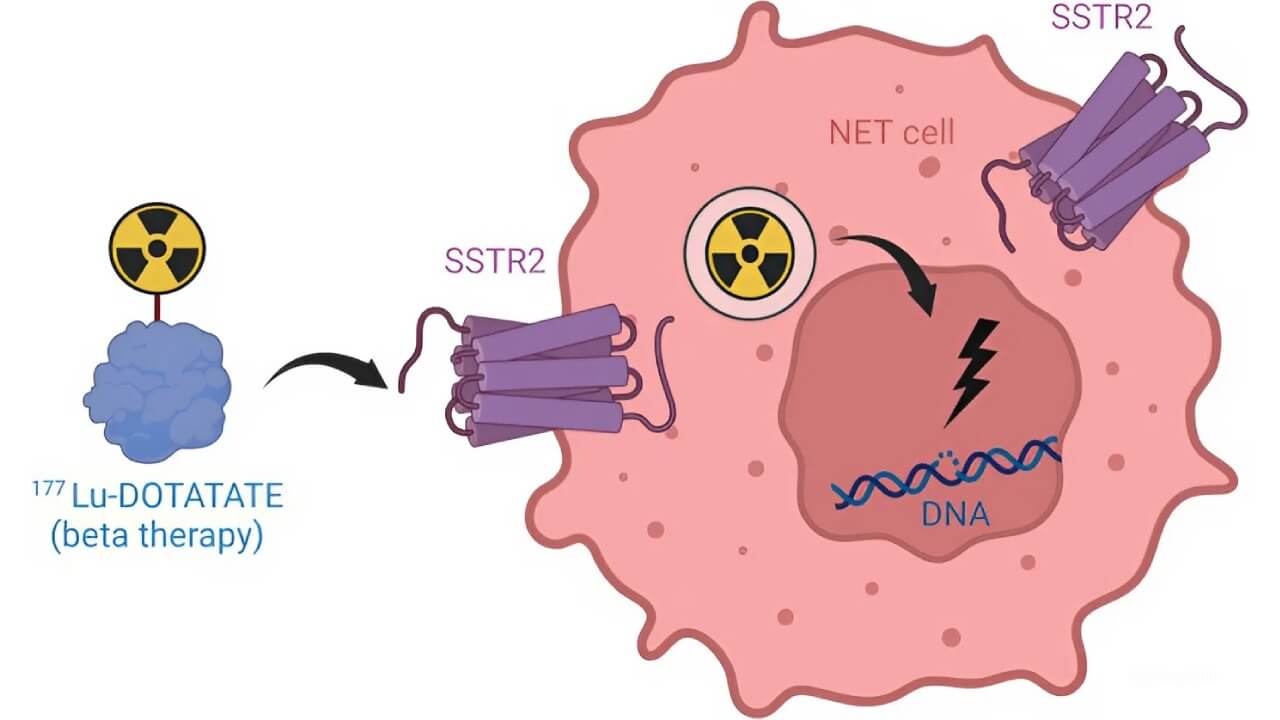
In Germany, PRRT is performed in specialized nuclear medicine centers, following strict safety protocols and international guidelines. For many patients, especially those with inoperable or treatment-resistant tumors, PRRT significantly improves both survival and quality of life.
Transarterial Chemoembolization (TACE) for Neuroendocrine Tumors
Transarterial Chemoembolization (TACE) is an advanced interventional technique used primarily for patients with neuroendocrine tumors that have spread to the liver. The procedure delivers chemotherapy directly into the arteries feeding the tumor, followed by tiny particles that block the blood supply—trapping the drug inside the tumor and starving it of oxygen.
This local approach allows for high concentrations of chemotherapy where it's needed most, with fewer systemic side effects. German interventional radiologists are among the most experienced in Europe, using the latest imaging and catheter-based systems to safely perform TACE on complex cases.
Dendritic Cell Immunotherapy for Neuroendocrine Tumors
Unlike conventional treatments that target the tumor directly, dendritic cell therapy works by rebooting the immune system to do the job itself. It starts by collecting a patient’s immune cells through a blood drawing. These cells are then exposed to tumor-specific antigens in a lab, trained to recognize the cancer, and finally injected back into the patient to mount a targeted immune attack.
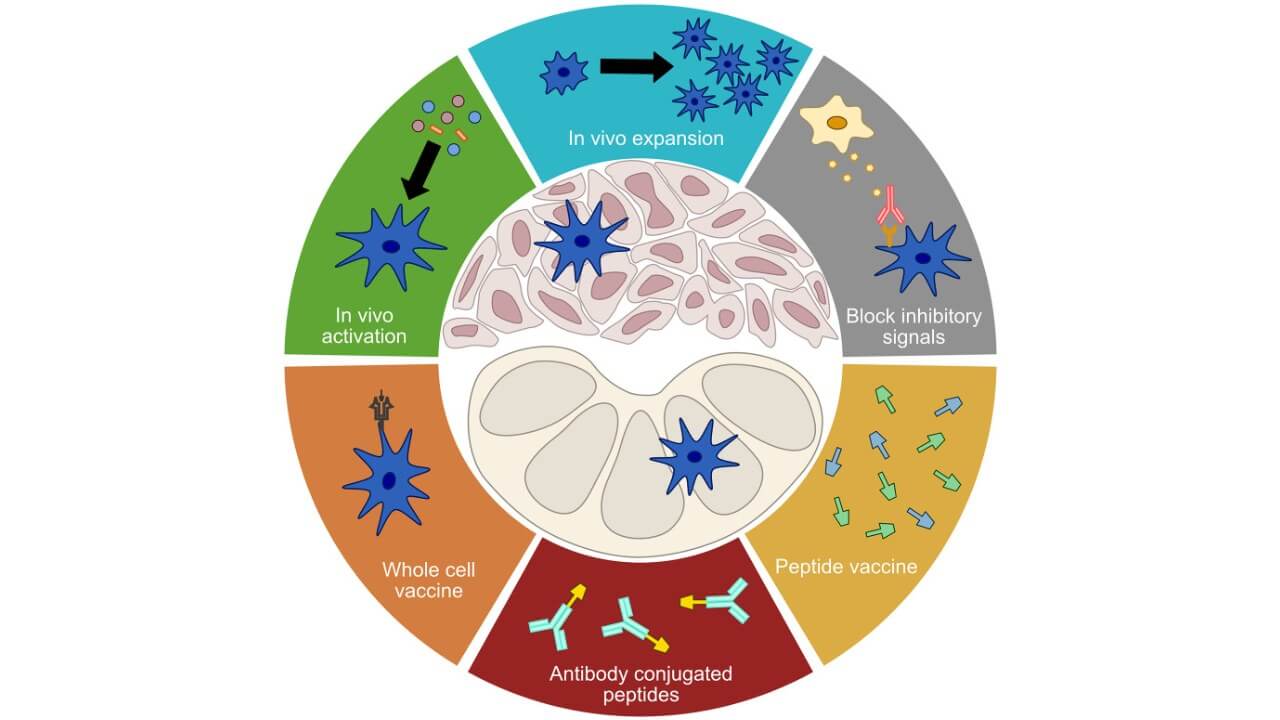
What makes this therapy so unique is its scientific foundation. Dendritic cells are the body’s key messengers between innate and adaptive immunity - something that wasn’t fully understood until their discovery fundamentally reshaped cancer immunology. That breakthrough earned global recognition in 2011, when Ralph Steinman’s work on dendritic cells was posthumously honored with the Nobel Prize [7].
In clinical practice, this approach has shown real-world benefits for patients with advanced or refractory neuroendocrine tumors: fewer side effects, better tolerance, and in many cases, meaningful tumor stabilization.
| Therapy Type | 2-Year Survival Rate | Response Rate | Duration | Side Effects |
|---|---|---|---|---|
| Standard Treatments | ~55-70% for early stages ~30% for advanced stages | ~40-60% | Several weeks to months | Moderate to severe (fatigue, nausea, infertility, bowel/bladder issues) |
| Innovative Methods | ~60-75% in select advanced/refractory cases | 45-65% | Multiple sessions are possible | Mild (fever, localized inflammation, flu-like symptoms) |
*Based on Booking Health clinical data and published outcomes. Actual results may vary depending on patient condition and treatment protocol.
Treatment of Neuroendocrine Tumors in Germany
Germany is widely recognized for its excellence in oncology and healthcare services, especially when it comes to managing complex and rare conditions like neuroendocrine tumors. With access to advanced diagnostics, multidisciplinary teams, and modern clinical treatment options, patients from around the world come to German hospitals in search of precise, personalized care.
Why Patients Choose NET Treatment in Germany
One major advantage of NET treatment in Germany is the high level of medical specialization. Many German hospitals operate within certified oncology networks, where surgeons, radiologists, endocrinologists, and nuclear medicine experts work as a team. These professionals are experienced in managing neuroendocrine cancers across all stages, from localized disease to widespread metastasis.
The availability of high-resolution imaging and comprehensive hormonal testing ensures accurate diagnosis and staging. This allows doctors to design tailored strategies using surgery, radiotherapy, Lutetium-based therapy, or immunotherapy.
With support from the coordinated healthcare service Booking Health, international patients can access this level of care without administrative complications.
Leading Hospitals and Oncology Centers for Neuroendocrine Tumors
Many clinical centers in Germany are internationally known for their focus on neuroendocrine tumor treatment. These hospitals not only offer advanced therapeutic options but also participate in ongoing clinical research, ensuring that patients benefit from the latest developments in medicine and healthcare.
Continuity of care is a major strength: patients are followed closely by their medical team throughout every stage—from first consultation through treatment and aftercare.
Cost and Organization of Neuroendocrine Tumors Treatment in Germany
When it comes to neuroendocrine tumor treatment in Germany, costs are transparent and fixed by law. Patients receive detailed quotes covering everything from diagnostics and surgery to hospital stay and follow-up care.
For international patients, Booking Health handles the full organization - from medical document review and hospital selection to appointment scheduling, translation, and cost control. This allows patients to focus on their recovery while all logistics and communication with German clinics are professionally managed.
| Cost of treatment | Standard Methods | Innovative Methods |
|---|---|---|
| Price of Treatment in Germany | $25,000 – $280,000 for a full course | $6,500 – $38,000 for full course |
| Price of Treatment in the UK | $26,000 – $320,000 for a full course | $25,000 – $60,000 for a full course |
| Price of Treatment in the USA | $100,000 – $350,000 for a full course | $40,000 – $150,000 for a full course |
From Misdiagnosis To Clarity: How Maria found Real Neuroendocrine Tumor Treatment Abroad
When Maria Estévez, a 46-year-old architect from Seville, started having episodes of facial flushing, abdominal pain, and unexplained fatigue, doctors initially thought it was early menopause. "I was told it was hormonal, stress-related. Nothing serious," she recalls.
But the symptoms didn’t go away. In fact, they got worse. Eventually, a scan revealed a neuroendocrine tumor (NET) in her pancreas, with liver metastases already present.
They began searching for more comprehensive treatment options and came across Booking Health, which helps patients arrange complex medical care in Germany.
"I filled out the form online late one evening," Javier says. "By the next morning, someone from Booking Health had already replied. They offered a detailed review of Maria’s case and suggested a leading oncology hospital in Munich that specializes in NET treatment with Lutetium therapy and immunotherapy."
Within two weeks, Maria was in Germany. Doctors confirmed the diagnosis and designed a personalized treatment plan that included PRRT with Lutetium-177, hormone-suppressing therapy, and nutrition support.
Booking Health managed all the practical things—appointments, paperwork, translations, and even helping with accommodations near the hospital. "We never felt lost," Javier says. "Their team was always one step ahead."
Now, after three therapy cycles, Maria’s disease is stable. Her symptoms have improved, and she’s back to part-time work, regaining energy and clarity.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex NET management programs in each individual case. As a reputable company, Booking Health offers personalized neuroendocrine tumor treatment plans with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for neuroendocrine tumors with leading specialists in this field.
FAQ: Neuroendocrine Tumors
Send request for treatmentNeuroendocrine tumors (NETs) are rare growths that start in hormone-producing cells. They can occur in the lungs, pancreas, intestines, or other organs and often grow slowly, sometimes without early symptoms.
The exact cause isn’t always clear, but genetic factors, certain syndromes, and chronic inflammation in the gut or pancreas can play a role in developing neuroendocrine tumors.
Yes, NETs are considered cancerous. Some grow slowly and behave more like benign tumors, while others are aggressive and spread quickly, especially high-grade neuroendocrine carcinomas.
Diagnosis involves blood tests, tumor markers, imaging (CT, MRI, or PET-CT), and biopsy. In Germany, advanced diagnostics help detect and classify neuroendocrine tumors with high precision.
Symptoms depend on tumor type and location. Common signs include flushing, diarrhea, abdominal pain, and unexplained weight loss. Hormone-producing tumors can cause additional systemic effects.
Treatment is highly individual and may include surgery, PRRT, TACE, or immunotherapy. Some of the best NET clinics in Germany offer comprehensive programs tailored to tumor grade and spread.
NETs can be cured, especially if found early and removed surgically. In advanced cases, NET treatment in Germany focuses on long-term control and improving quality of life.
PRRT (Peptide Receptor Radionuclide Therapy) uses radioactive Lutetium-177 to target tumor cells. PRRT in Germany is offered in specialized nuclear medicine clinics and is effective for many NETs.
Immunotherapy, including dendritic cell treatment, can be effective in select NET cases. In Germany, it's available through personalized programs, often when standard options are limited.
Top centers for neuroendocrine tumors in Germany include clinics in Munich, Heidelberg, and Essen. Many are part of certified oncology networks offering multidisciplinary care.
The cost of treatment in Germany depends on the therapy type. PRRT, surgery, and diagnostics are usually billed as fixed-price packages with full transparency through Booking Health.
NETs are treated by a team of specialists: oncologists, surgeons, endocrinologists, and nuclear medicine experts - especially in dedicated NET clinics in Germany.
Yes, many German hospitals offer expert second opinions. Booking Health can arrange case reviews by NET specialists, even before you travel, based on your existing medical documents.
You can contact Booking Health to coordinate every step - from medical record review and clinic selection to visa support and translation - ensuring smooth access to NET treatment in Germany.
Treatment for neuroendocrine tumors includes surgery, chemotherapy, and innovative therapies (e.g., peptide receptor radionuclide therapy (PRRT), transarterial chemoembolization (TACE), and dendritic cell immunotherapy). Typically, the choice depends on the tumor's grade, location, and stage.
Symptoms of neuroendocrine tumors (NETs) can vary by tumor location and hormone activity. Common signs include abdominal pain, diarrhea, flushing, wheezing, fatigue, and unexplained weight loss. Hormone-secreting NETs may also cause carcinoid syndrome with flushing and heart valve changes.
In Germany, standard neuroendocrine tumor (NET) treatment costs range from $25,000-$280,000, and innovative methods cost $6,500-$38,000. In the UK, prices range from $26,000-$320,000 and $25,000-$60,000, while in the USA, they reach $100,000-$350,000 and $40,000-$150,000, respectively. In contrast, Australia often has limited access to advanced NET therapies, and prices can be up to four times higher than in Europe.
The 2-year survival rate for neuroendocrine tumors (NETs) is about 55-70% with standard treatments. However, it can reach 60-75% with innovative methods such as PRRT, TACE, or immunotherapy, especially in advanced or refractory cases.
Response rates of neuroendocrine tumor (NET) treatment vary: 40-60% for standard treatments and 45-65% for advanced options (e.g., PRRT and dendritic cell therapy), which can provide higher tumor control and improved long-term outcomes.
During neuroendocrine tumor (NET) treatment, standard therapies can cause fatigue, nausea, bowel changes, infertility, or skin irritation. In turn, innovative methods typically result in mild flu-like symptoms or localized inflammation, offering better tolerance.
Standard neuroendocrine tumor (NET) therapy usually lasts several weeks to months. On the other hand, innovative treatments (e.g., PRRT, dendritic cell vaccination, etc.) involve multiple sessions over shorter periods. As such, these methods can allow quicker recovery and improved quality of life.
Choose treatment abroad and you will be sure to get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Peiwen Wu, Dongjie He, Hao Chang, Xiaozhi Zhang. Epidemiologic trends of and factors associated with overall survival in patients with neuroendocrine tumors over the last two decades in the USA. Endocr Connect. 2023 Nov 23;12(12):e230331. doi: 10.1530/EC-23-0331. Print 2023 Dec 1. [DOI] [PubMed]
[2] Qamar Sultana, Jill Kar, Amogh Verma at al. A Comprehensive Review on Neuroendocrine Neoplasms: Presentation, Pathophysiology and Management. J Clin Med. 2023 Aug 5;12(15):5138. doi: 10.3390/jcm12155138. [DOI] [PubMed]
[3] Bryan Oronsky, Patrick C Ma, Daniel Morgensztern, Corey A Carter. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia . 2017 Dec;19(12):991-1002. doi: 10.1016/j.neo.2017.09.002. Epub 2017 Nov 5. [DOI] [PubMed]
[4] Jessica E Maxwell, James R Howe. Imaging in neuroendocrine tumors: an update for the clinician. Int J Endocr Oncol. 2015;2(2):159-168. doi: 10.2217/ije.14.40. [DOI] [PubMed]
[5] Jelka Kuiper, Eline Zoetelief, Tessa Brabander, Wouter W de Herder, Johannes Hofland. Current status of peptide receptor radionuclide therapy in grade 1 and 2 gastroenteropancreatic neuroendocrine tumours. J Neuroendocrinol. 2025 Mar;37(3):e13469. doi: 10.1111/jne.13469. Epub 2024 Nov 20. [DOI] [PubMed]
[6] Alycia Gardner, Álvaro de Mingo Pulido, Brian Ruffell. Dendritic Cells and Their Role in Immunotherapy. Front Immunol. 2020 May 21;11:924. doi: 10.3389/fimmu.2020.00924. [DOI] [PMC free article]
[7] Nobel Prize. The Nobel Prize in Physiology or Medicine 2011 – Ralph Steinman. https://www.nobelprize.org/prizes/medicine/2011/steinman/facts/
Read:
New Effective Treatments for Stage 4 Cancer: Innovations in Oncology
Treatment of Gastrointestinal Neuroendocrine Tumors
Gastrointestinal oncology in the fight against cancer: meeting with experts
Article menu:
- Understanding Neuroendocrine Tumors
- Diagnostic Methods of NETs
- Standard Treatment Options for Neuroendocrine Tumors
- Advanced and Innovative Therapies
- Treatment of Neuroendocrine Tumors in Germany
- From Misdiagnosis To Clarity: How Maria found Real Neuroendocrine Tumor Treatment Abroad
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ: Neuroendocrine Tumors
Don't know where to start?
Contact Booking Health