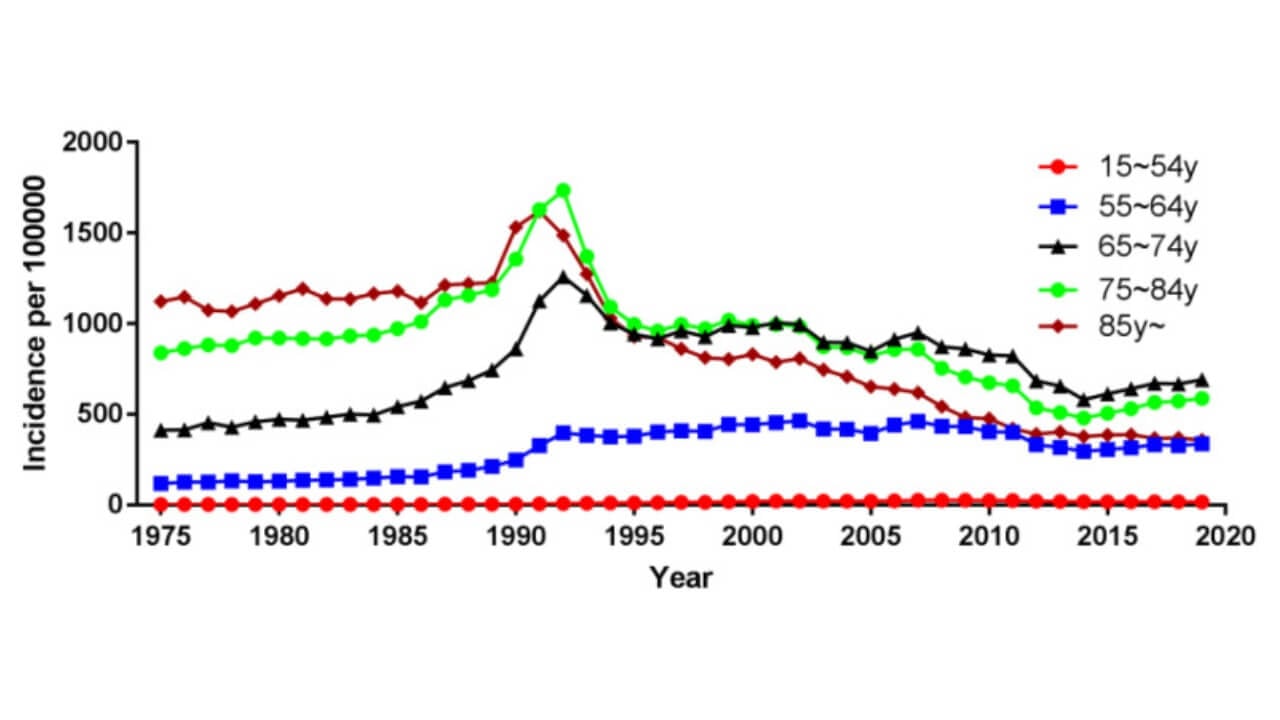
Prostate cancer is the second most common cancer diagnosis among men and remains one of the leading causes of cancer-related deaths worldwide. According to GLOBOCAN 2018, more than 1,276,000 new cases were reported globally, with a particularly high incidence in developed countries [1]. The risk of developing prostate cancer increases with age, especially after 65, and African-American men are more likely to be diagnosed with prostate cancer at a younger age and often face a more aggressive cancer compared to white men.
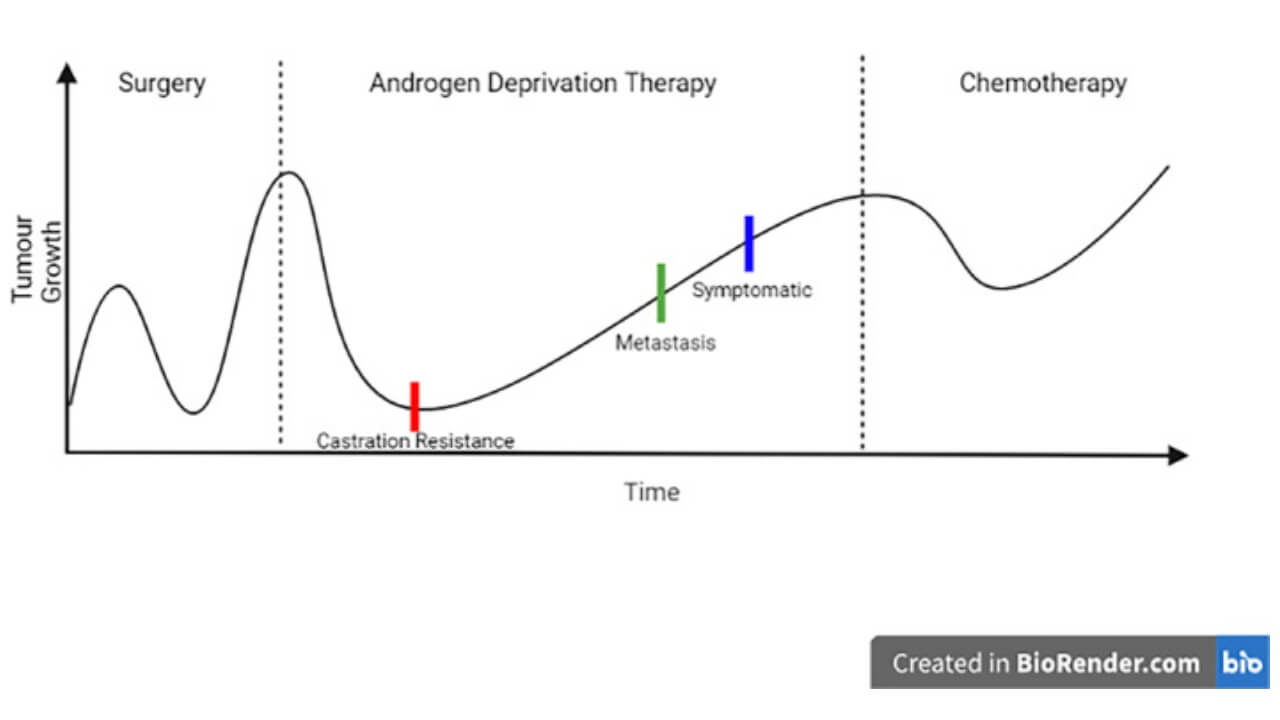
Although most prostate cancers progress slowly, the absence of symptoms in the early stages makes the diagnosis for prostate cancer challenging. This is why prostate cancer early detection programs, including prostate cancer screening with the PSA test and modern imaging tests, play a crucial role. When identified before the cancer has spread beyond the prostate gland or nearby lymph nodes, patients usually have excellent chances with timely prostate cancer treatment, including surgery, radiation therapy, or hormone therapy.
Localized prostate cancer is often curable. However, once the cancer cells escape the prostate tissue and the cancer spreads, the disease may require systemic approaches and advanced therapies. Therefore, early and precise prostate cancer diagnosis remains the cornerstone for improving outcomes and even surviving prostate cancer.
How is Prostate Cancer Diagnosed?
The first step in the diagnosis of prostate cancer usually begins with a blood test to measure the level of prostate-specific antigen (PSA). Elevated PSA may indicate prostate cancer cells, but it can also be linked to benign prostatic hyperplasia—an enlarged prostate. For this reason, the PSA test serves as a screening tool rather than a definitive method to diagnose prostate cancer.
Screening Tests and Clinical Evaluation
When the PSA test results are abnormal, doctors recommend further screening tests and a clinical examination. The diagnostic pathway often includes:
- Digital rectal examination to evaluate the prostate gland
- Transrectal ultrasound to visualize suspicious areas
- Imaging tests such as magnetic resonance imaging (prostate MRI) or CT scan to identify lesions and assess whether the cancer has spread to surrounding tissues or lymph nodes
These diagnostic tests help determine whether a patient requires tissue confirmation for a specific condition.
Prostate Biopsy as the Gold Standard
A prostate biopsy remains the only reliable method to confirm the presence of cancer cells. During the procedure, doctors take a tissue sample from the prostate tissue. Examination of prostate biopsy samples under a microscope allows pathologists to confirm malignancy and determine the prostate cancer grade.
Types of biopsy include:
- Transrectal biopsy–the most widely used technique, often guided by ultrasound
- MRI-guided biopsy–used to improve accuracy in detecting localized prostate cancer
The final prostate biopsy results show whether most prostate cancer cells are still confined to the gland or if the cancer has spread.
Importance of Early Detection
Since early stages rarely cause specific symptoms, it is difficult to diagnose prostate cancer based only on clinical signs. That is why regular prostate cancer screening with the PSA test is recommended for men over 50, as well as those with increased prostate cancer risk.
A timely prostate cancer diagnosis makes it possible to plan effective prostate cancer treatment, such as radical prostatectomy, radiation therapy, or hormone therapy, before the cancer spreads further. This strategy provides the best outcomes for prostate cancer patients and prevents progression to advanced prostate cancer.
How is the Prostate Cancer Test Called?
The most common test for prostate cancer diagnosis is the PSA test (measurement of prostate-specific antigen in the blood). It is the cornerstone of prostate cancer early detection programs. Elevated PSA levels often raise suspicion of prostate cancer cells, but this marker is not always specific. Therefore, the blood test requires confirmation with other diagnostic tests to accurately diagnose prostate cancer.
Why PSA Levels May Be Elevated
An increase in PSA does not always indicate the presence of cancer cells in the prostate gland. The PSA concentration may rise due to:
- Prostatitis (inflammation of the prostate tissue)
- Benign prostatic hyperplasia—enlarged prostate
- Recent urological surgery or prostate procedures
- Prostate biopsy or prostate massage
- Catheterization of the bladder, cystoscopy, and colonoscopy
- Certain medications
This is why PSA screening alone cannot serve as a definitive cancer diagnosis.
PSA Fractions: Total and Free
There are two main fractions of PSA in the blood:
- Total PSA–the sum of free PSA and PSA bound to proteins
- Free PSA–the unbound fraction
Measuring both helps physicians assess the risk of developing prostate cancer and decide whether to perform a prostate biopsy.
PSA Levels and Risk of Prostate Cancer
- If PSA is below 4 ng/ml, the probability of detecting most prostate cancers is very low, and the likelihood of finding cancer cells during a prostate biopsy does not exceed 0.5%.
- If PSA is above 20 ng/ml, the probability that the cancer has spread or that aggressive cancer is present rises dramatically, up to 75%. In such cases, a prostate biopsy and histological tissue sample examination are mandatory.
- The "gray zone" (PSA between 4 and 10 ng/ml) presents the greatest challenge. In this range, it is difficult to confirm a prostate cancer diagnosis without additional imaging tests or repeat PSA monitoring.
The Need for Additional Diagnostic Methods
Since the PSA test is not fully reliable, additional procedures such as transrectal ultrasound, prostate MRI, or CT scan are often used to increase the specificity of diagnostic tests. These help determine whether a prostate biopsy is required and whether cancer has spread to nearby lymph nodes.
Ultimately, while the PSA level remains the foundation of prostate cancer screening, it must always be combined with other approaches to accurately diagnose prostate cancer and plan effective prostate cancer treatment.
Differential Diagnostics
Differential diagnostics are essential to distinguish prostate cancer from other conditions, such as benign prostatic hyperplasia or prostatitis, since PSA test results alone cannot confirm a prostate cancer diagnosis. Men in the "gray zone," with PSA levels between 4 and 10 ng/ml, require additional evaluation with diagnostic tests, clinical assessment, and calculation of specific indices to assess the risk of developing prostate cancer.
Factors Considered in Differential Diagnostics
Doctors take several factors into account to determine the likelihood of prostate cancer:
- Age of the patient–PSA levels naturally increase with age. For men under 50, normal PSA usually does not exceed 2.5 ng/ml, while after 70, PSA up to 6 ng/ml can be normal. This is important for assessing the prostate cancer risk.
- Ratio of PSA fractions–The proportion of free to total prostate-specific antigen helps differentiate between benign hyperplasia and prostate cancer cells.
- Below 15%–high probability of a tumor
- 15–23%–moderate risk
- Above 23%–low risk (most likely the PSA increase is due to benign prostatic hyperplasia)
Studies indicate that when the ratio is below 10%, the chance of detecting prostate cancer during a prostate biopsy reaches 44%. A ratio of 10–15% corresponds to a 33% probability, while above 26%, the likelihood of finding cancer cells falls below 11%.
- PSA density index–This calculation considers both the volume of the prostate gland (assessed via transrectal ultrasound) and the PSA level. In prostate cancer, the density usually exceeds 0.15 ng/ml per cubic centimeter. Lower values suggest a low probability of malignancy.
- Dynamics of PSA increase–Normally, total PSA should rise by no more than 0.75 ng/ml per year. Faster increases may indicate the presence of aggressive cancer and warrant further diagnostic tests.
Importance of Differential Diagnostics
Careful evaluation of PSA levels, PSA fractions, density index, and their dynamics allows clinicians to decide whether to perform a prostate biopsy. This helps accurately identify localized prostate cancer, determine if the cancer has spread to lymph nodes, and select the most appropriate prostate cancer treatment for the patient.
Biochemical Recurrence of Prostate Cancer
The PSA test is important not only for the initial prostate cancer diagnosis, but also for follow-up after prostate cancer treatment. Regular measurement of prostate-specific antigen (PSA) helps doctors track whether the disease returns, evaluate therapy results, and adjust care for prostate cancer patients.
Role of PSA in Detecting Recurrence
After radical prostatectomy or radiation therapy, PSA levels provide valuable insight into the presence of prostate cancer cells:
- Detection of metastases – a rising PSA may mean the cancer has spread to lymph nodes or distant organs, signaling advanced prostate cancer.
- Stage evaluation – PSA dynamics help define the current stage and influence the choice of further prostate cancer treatment.
- Recurrence monitoring – biochemical relapse is diagnosed when PSA begins to rise again after therapy.
- Treatment success – effective surgery usually lowers PSA to ≤0.2 ng/ml, while successful radiation therapy keeps it around 1 ng/ml or less.
Indicators of Relapse
In men after prostate cancer surgery, the pace of PSA doubling is highly informative:
- Rapid doubling (within 4.3 months) often points to systemic relapse and calls for therapies such as hormone therapy or external beam radiation therapy.
- Doubling within 11.7 months usually indicates local recurrence, which can often be managed with targeted measures.
Tracking PSA trends makes it possible to identify aggressive cancer early. This approach improves outcomes for surviving prostate cancer patients and helps prevent further cancer spread.
Clinical Diagnosis
Clinical evaluation plays a key role in prostate cancer diagnosis. Although PSA testing is the main screening tool, examination of the prostate gland by digital rectal examination helps detect localized prostate cancer before invasive procedures are considered.
Role of Digital Rectal Examination
This test is usually done after the PSA test, because manipulation of the prostate tissue can raise prostate-specific antigen (PSA) levels and cause a false positive. The method cannot reliably separate prostate cancer from prostatitis or benign prostatic hyperplasia (BPH), but it allows doctors to notice a tumor-like formation if one is present.
Patients are then divided into groups:
- With a palpable tumor – further evaluation is needed
- Without a palpable tumor – if PSA is in the gray zone, additional studies may not be necessary
Additional Tests for Patients with Palpable Tumor
When a palpable tumor is found, several diagnostic tests help estimate the risk and decide on the need for a prostate biopsy. These include measuring free PSA and its ratio to total PSA, Transrectal ultrasound to check prostate size, calculation of the PSA density index, and monitoring the dynamics of PSA increase.
Although none of these methods can fully confirm the presence of prostate cancer cells, they guide the decision to perform a biopsy. Such an approach ensures that prostate cancer patients receive timely evaluation and, if cancer is proven, effective prostate cancer treatment.
Can Prostate Cancer Be Seen on the Ultrasound?
Ultrasound is widely used as part of diagnostic tests in the evaluation of prostate cancer, but it is not conclusive. Prostate cancer cells cannot be definitively identified with standard ultrasound alone, and additional imaging tests are often required to confirm the prostate cancer diagnosis.
The doctor can estimate:
- Size of the prostate gland
- Presence of hyperechoic or hypoechoic areas, which reflect variations in prostate tissue density
- Echogenicity patterns that may suggest localized prostate cancer or abnormalities in the prostate cells
Objectives of Ultrasound in Prostate Cancer Diagnosis
- Identify additional signs of prostate cancer and determine the need for prostate biopsy
- Detect hypo- and hyperechoic areas to improve biopsy accuracy by guiding tissue sampling for histological analysis (prostate biopsy samples)
Ultrasound Appearance of Prostate Cancer
Classically, prostate cancer appears as hypoechoic focal zones on the periphery of an enlarged prostate. As tumors grow, the structure becomes heterogeneous, with both hypo- and hyperechoic areas. However, more than a third of cases show isoechoic areas, making tumors visually similar to healthy prostate tissue.
Limitations of Ultrasound
Ultrasound cannot reliably distinguish benign prostatic hyperplasia or adenoma from malignant tumors, nor can it detect early metastatic prostate cancer. However, when combined with PSA test results, PSA density index, or the ratio of free and total PSA, ultrasound findings help determine the urgency and location for a transrectal biopsy. Advanced imaging tests, such as magnetic resonance imaging (prostate MRI) or CT scan, are often recommended to improve diagnostic accuracy and guide treatment decisions for prostate cancer patients.
Confirmation of prostate cancer diagnosis
All diagnostic tests, including the PSA test, ultrasound, and clinical diagnosis, aim to determine the need for a prostate biopsy in each patient, as prostate cancer can only be confirmed through histological examination of prostate biopsy samples. Other tests may indicate suspicion of prostate cancer cells, but they cannot establish a definitive cancer diagnosis.
Many prostate cancer patients are concerned about a biopsy because it is an invasive procedure. Some ask whether it is possible to diagnose prostate cancer without a biopsy. In advanced stages, particularly in metastatic prostate cancer, extremely high PSA levels may make the tumor evident, but a biopsy is still necessary. It is used not only to confirm prostate cancer, but also to determine the prostate cancer grade, assess prognosis, and plan prostate cancer treatment, which may include radical prostatectomy, external beam radiation therapy, internal radiation therapy, or hormone therapy.
During a prostate biopsy, a needle is inserted into the prostate gland through the rectum, usually taking multiple tissue samples from different parts of the prostate tissue. Modern techniques make the procedure less painful using infiltration anesthesia.
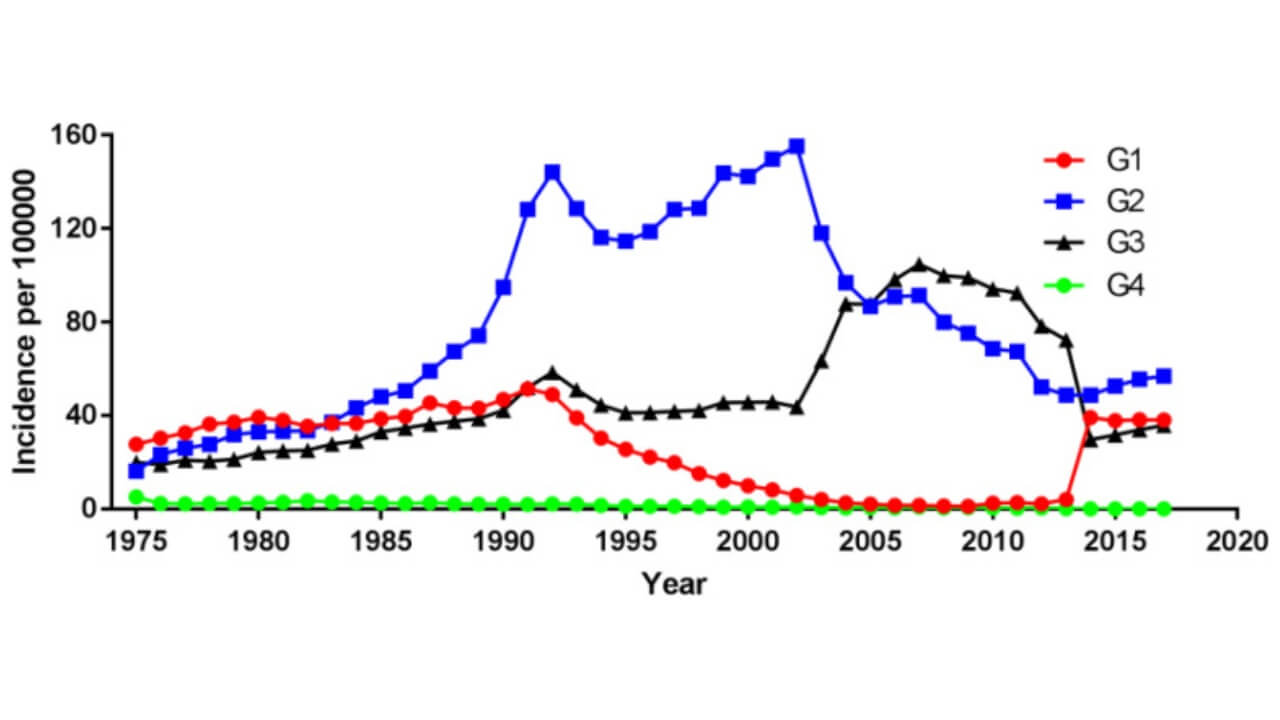
The prostate biopsy results also allow evaluation of tumor aggressiveness using the Gleason scale, which assigns a prostate cancer grade from 2 to 10 based on the most prevalent patterns of prostate cancer cells in the samples. Scores from 6 indicate the presence of prostate cancer, with higher numbers reflecting aggressive cancer. The Grade Group system refines prognosis assessment, guiding therapy for both localized prostate cancer and metastatic prostate cancer.
Ultimately, PSA test, ultrasound, and digital rectal examination are indicative, but only the prostate biopsy provides a definitive prostate cancer diagnosis and informs appropriate prostate cancer treatment for prostate cancer patients. Even though the biopsy may be uncomfortable, it is essential for accurate assessment of prostate cancer cells and planning of therapy.
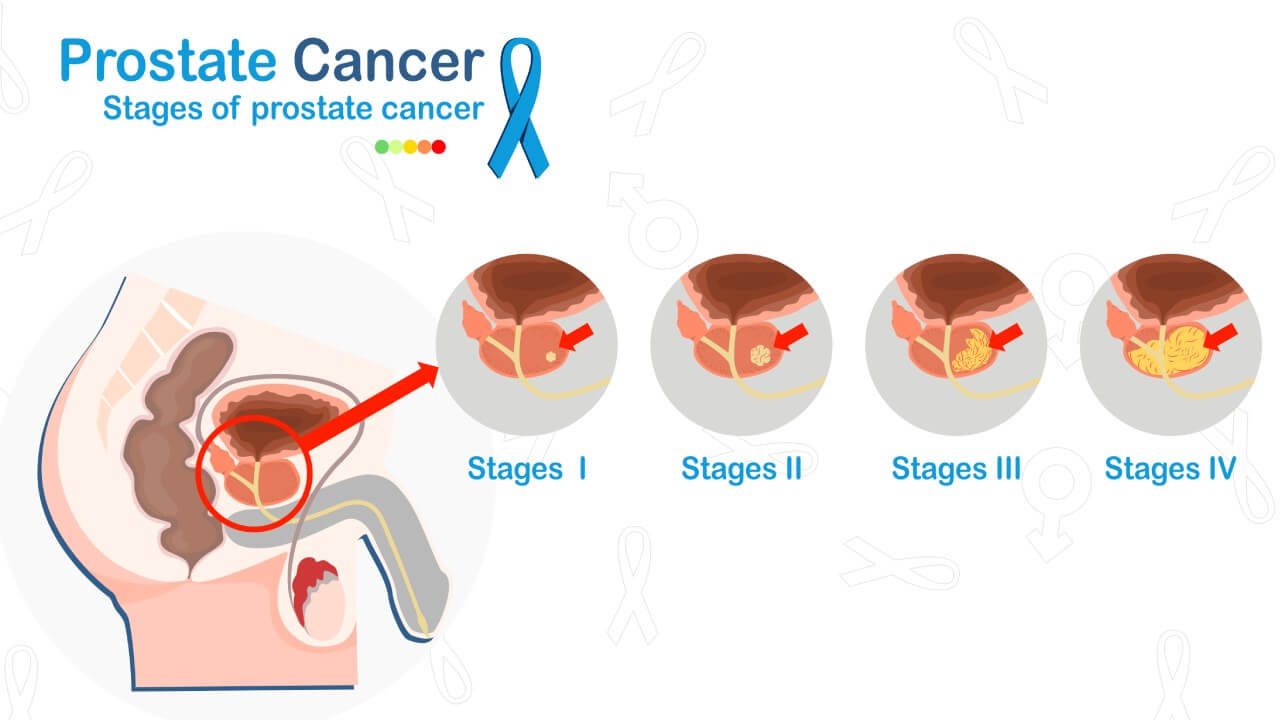
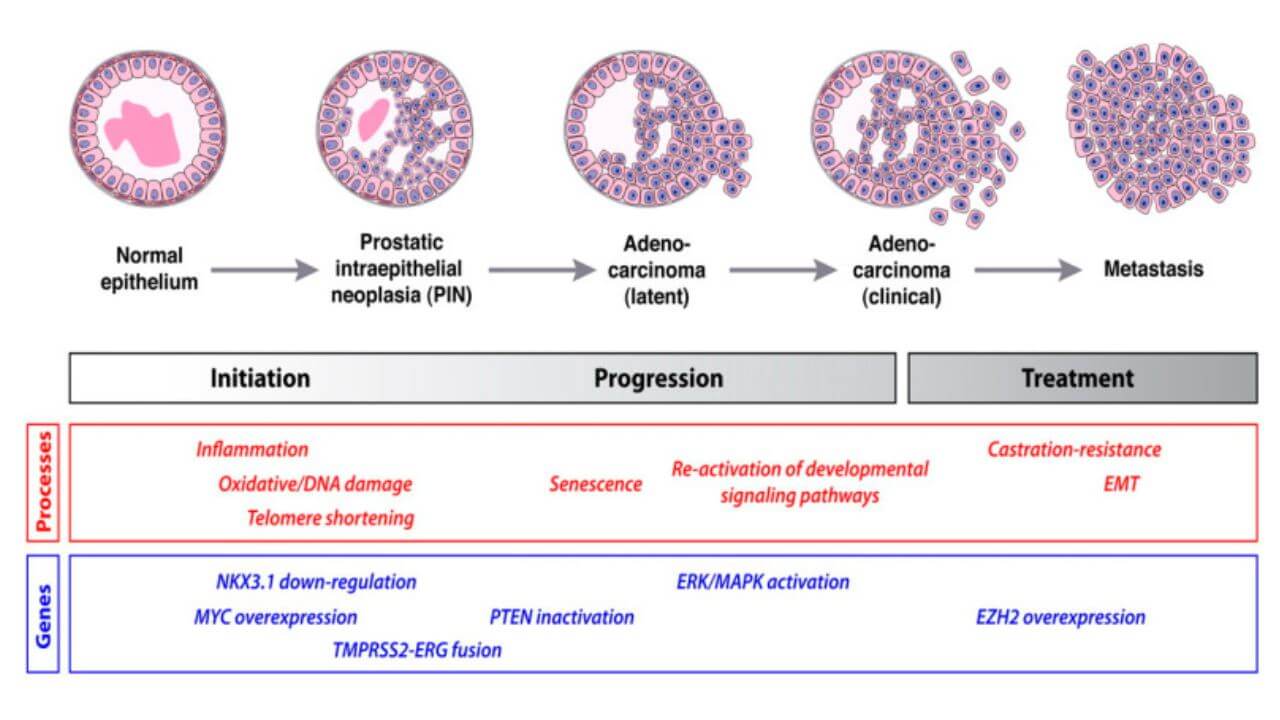
Staging
A complete prostate cancer diagnosis cannot be made without establishing the stage of prostate cancer. The stage is determined based on the characteristics of the tumor, the presence of regional lymph nodes or distant cancer spread, the prostate cancer grade according to the Gleason scale, and PSA test results [3].
Stage 1. Thanks to diagnostic tests, it is possible to detect prostate cancer at the first stage even without a palpable tumor. This corresponds to Grade Group 1 (Gleason score 6 or less) and a PSA level below 10 ng/ml. This is considered a low-risk cancer.
Stage 2. At this stage, the tumor can be palpated, and an ultrasound may detect prostate cancer. The tumor is located on one or both sides of the prostate gland, with prostate cancer grade 1, 2, or 3, and PSA levels between 10–20 ng/ml.
Stage 3. The tumor reaches a large size and begins to invade surrounding organs and tissues. Symptoms may appear, such as urination problems or discomfort. No distant cancer spread is observed yet. PSA levels vary, and prostate cancer grade can range from 1 to 4 or 5.
Stage 4. This stage is determined regardless of prostate cancer grade or PSA levels. If metastases are found in nearby lymph nodes, it is classified as stage 4A. Stage 4B is established if distant cancer spread is detected.
Various imaging tests are used to assess tumor spread, including transrectal ultrasound, CT scan, magnetic resonance imaging (prostate MRI), chest X-ray, and skeletal scintigraphy. Metastatic prostate cancer may be confirmed via biopsy of pelvic lymph nodes or seminal vesicles, especially if prostate cancer grade is 8 or higher, whereas for low-risk cancer with Gleason 7 or less, the probability of detecting metastases is only about 3%.
Clinical Signs of Prostate Cancer
We have already discussed which diagnostic tests detect prostate cancer even in the early stages. The PSA test can establish a prostate cancer diagnosis long before the first clinical signs appear. Symptoms usually indicate that the tumor has grown significantly and may correspond to stage 3, when the prostate cancer spreads into surrounding organs and tissues.
Some symptoms of prostate cancer may appear during stage 2, but their occurrence depends largely on the location of the tumor within the prostate gland.
The First Signs of Prostate Cancer
Most prostate cancer patients want to know which symptoms appear first. Early detection allows timely consultation and treatment, but in most cases, there are no noticeable clinical signs. Adenocarcinoma often develops in the peripheral parts of the prostate tissue, so even when the tumor becomes palpable, it may not compress surrounding organs.
However, depending on the tumor’s location, it can affect:
- Urethra
- Nerves
- Ureters
- Rectum
- Bladder
At the initial stage, the symptoms of prostate cancer and benign prostatic hyperplasia are similar, arising mainly from compression of the urethra. Patients may experience:
- Difficulty during urination
- Weak urine stream
- Feeling of incomplete bladder emptying
Additional signs appear when the tumor involves other prostate tissue, such as the rectum or seminal vesicles. In these cases, patients may suffer from constipation, and blood may appear in the ejaculate when prostate cancer spreads to the seminal vesicles.
How does prostate cancer develop in the 3rd stage?
When prostate cancer reaches a large size, it is usually accompanied by pronounced symptoms depending on the location of the tumor.
- Ureter involvement–The patient may develop kidney inflammation, pain in the lower back caused by urine reflux, and, in cases of complete obstruction, an acute pain syndrome similar to renal colic. Pain occurs because the kidney capsule stretches, as it contains many sensitive nerve endings.
- Bladder involvement–The tumor reduces bladder capacity, causing frequent urination. Hematuria, urinary incontinence, or urgent uncontrollable urination may also appear, reflecting the spread of prostate cancer cells to the bladder.
- Nerve involvement–Pain syndrome develops, often localized in the perineum, scrotum, or rectum, sometimes radiating to the penis. Erectile dysfunction may occur. Pain may be diffuse, making it difficult for the patient to determine its exact location.
Symptoms of Prostate Cancer in Stage 4
At stage four, the disease is usually marked by cancer spread, often starting with the lymph nodes, which may cause leg swelling. Metastatic prostate cancer can also appear through fractures of the spine or long bones. Bone tissue is the most common site for secondary tumors. Remote metastases usually occur only in the last phase, and sometimes there are no clear clinical signs of prostate cancer until this point.
It is important for every prostate cancer patient to know that such symptoms often indicate a late stage with an unfavorable prognosis. This makes timely testing essential. Regular prostate cancer screening, including blood tests for prostate-specific antigen (PSA) and an exam by a urologist, is considered the most reliable way to detect developing prostate cancer at an early stage.
For a deeper insight into modern urology in Germany, including advanced diagnostics, surgical techniques, and patient-centered care, we recommend watching an informative interview with Dr. Daniel Kaminski. He explains how contemporary urological treatments are applied, how late-stage prostate cancer is managed, and what international patients can expect when seeking care in German clinics.
Hospitals and The Cost of Treatment
In case of suspected prostate cancer, it is better to undergo examination in specialized hospitals or departments of multidisciplinary university hospitals. Since this disease affects the male reproductive system, accurate diagnostics is crucial. Modern clinics not only confirm the diagnosis but also evaluate the role of the immune system in controlling tumor growth. If the diagnosis is confirmed, doctors can immediately treat prostate cancer with advanced methods, including targeted therapies designed to destroy cancer cells more effectively. The use of innovative technologies, such as prostate-specific membrane antigen imaging, helps detect even small lesions and choose the best treatment strategy. The leading hospitals for the diagnostics and treatment of prostate cancer are:
- Helios Hospital Berlin-Buch
- University Hospital of Ludwig Maximilian University of Munich
- University Hospital Ulm
- Urology Hospital Munich-Planegg Munich
- Urology Clinic Wiener Platz
- University Hospital Erlangen
- University Hospital Jena
- University Hospital Greifswald
| Procedure | Average Cost (€) |
|---|---|
| Diagnostics of prostate cancer | 4,750 |
| Diagnostics of prostate cancer with PSMA PET-CT | 5,500 - 5,700 |
| PSMA therapy with Lutetium-177 for metastatic prostate cancer | 22,700 – 26,400 |
| Brachytherapy (implantation of radioactive gold "seeds") | 13,600 – 17,400 |
| High-intensity focused ultrasound (HIFU) ablation | 19,100 - 21,400 |
| Radiation therapy for prostate cancer | 27,100 – 30,700 |
| Intensity-modulated radiation therapy (IMRT) | 24,200 - 31,000 |
| Proton therapy | 56,900 – 90,500 |
| Transurethral electroresection of the prostate or laparoscopic tumor removal | 10,000 – 10,800 |
| Nerve-sparing radical prostatectomy | 15,700 – 21,500 |
| Rehabilitation after the main course of treatment | 1,580 per day |
The exact cost of the examination or treatment is determined after the first consultation with a doctor.
A Medical Journey: Every Step of the Way With Booking Health
Finding the best treatment strategy for your clinical situation is a challenging task. Being already exhausted from multiple treatment sessions, having consulted numerous specialists, and having tried various therapeutic interventions, you may be lost in all the information given by the doctors. In such a situation, it is easy to choose a first-hand option or to follow standardized therapeutic protocols with a long list of adverse effects instead of selecting highly specialized innovative treatment options.
To make an informed choice and get a personalized cancer management plan, which will be tailored to your specific clinical situation, consult medical experts at Booking Health. Being at the forefront of offering the latest medical innovations for already 12 years, Booking Health possesses solid expertise in creating complex management programs in each individual case. As a reputable company, Booking Health offers personalized treatment plans for prostate cancer with direct clinic booking and full support at every stage, from organizational processes to assistance during treatment. We provide:
- Assessment and analysis of medical reports
- Development of the medical care program
- Selection of a suitable treatment location
- Preparation of medical documents and forwarding to a suitable clinic
- Preparatory consultations with clinicians for the development of medical care programs
- Expert advice during the hospital stay
- Follow-up care after the patient returns to their native country after completing the medical care program
- Taking care of formalities as part of the preparation for the medical care program
- Coordination and organization of the patient's stay in a foreign country
- Assistance with visas and tickets
- A personal coordinator and interpreter with 24/7 support
- Transparent budgeting with no hidden costs
Health is an invaluable aspect of our lives. Delegating management of something so fragile yet precious should be done only to experts with proven experience and a reputation. Booking Health is a trustworthy partner who assists you in pursuing stronger health and a better quality of life. Contact our medical consultant to learn more about the possibilities of personalized treatment with innovative methods for prostate cancer with leading specialists in this field.
Advanced Cancer Treatment: Patient Success Stories with Booking Health
FAQ: Prostate Cancer Diagnosis
Send request for treatmentProstate cancer diagnosis in Germany combines PSA testing, DRE Germany, imaging tests like MRI of prostate in Germany, and prostate biopsy procedure in Germany to detect prostate cancer cells accurately. Advanced labs and expert urologists ensure reliable diagnostic tests for all prostate cancer patients.
Early detection relies on prostate cancer screening with PSA screening, usually starting at age 50. Blood tests, digital rectal examination, and periodic imaging tests help identify developing prostate cancer, even when symptoms are absent.
Before biopsy, CT scan, transrectal ultrasound, and MRI of the prostate in Germany are standard imaging tests. These methods locate suspicious prostate tissue and guide transrectal biopsy for accurate prostate cancer diagnosis.
PSMA PET‑CT diagnosis is used to detect metastatic prostate cancer and identify cancer spread to lymph nodes or distant organs. It provides high accuracy in locating prostate cancer cells before surgery or radiation therapy.
The prostate biopsy procedure in Germany involves taking multiple prostate biopsy samples using a transrectal or transperineal approach. Tissue samples are analyzed for prostate cancer grade, Gleason score, and presence of aggressive cancer.
The Gleason score for prostate cancer measures tumor aggressiveness. It sums the two most common patterns of prostate cancer cells in prostate tissue, guiding treatment decisions such as radical prostatectomy, radiation therapy, or hormone therapy.
Prostate cancer diagnostics cost in Germany depends on PSA tests, imaging, and biopsy. Prices vary by clinic, complexity, and whether internal radiation therapy or external beam radiation therapy is required for advanced prostate cancer.
Yes, Booking Health diagnostics support coordinates prostate cancer diagnosis, appointments, and treatments with German clinics, ensuring international patients have access to prostate biopsy procedures in Germany and follow-up cancer treatment.
International patients' prostate diagnosis in Germany is possible. Clinics provide diagnostic tests, imaging like MRI, PSMA PET‑CT diagnosis, and timely prostate cancer treatment, with support for travel and documentation.
For post-diagnosis prostate cancer in Germany, patients may undergo prostate cancer surgery, radiation therapy, hormone therapy, or active surveillance for low-risk cancer. Treatment depends on the Gleason score, cancer spread, and overall prostate cancer grade.
Choose treatment abroad and you will for sure get the best results!
Authors:
This article was edited by medical experts, board-certified doctors Dr. Nadezhda Ivanisova, and Dr. Bohdan Mykhalniuk. For the treatment of the conditions referred to in the article, you must consult a doctor; the information in the article is not intended for self-medication!
Our editorial policy, which details our commitment to accuracy and transparency, is available here. Click this link to review our policies.
Sources:
[1] Prashanth Rawla. Epidemiology of Prostate Cancer. World J Oncol. 2019 Apr;10(2):63-89. doi: 10.14740/wjon1191. Epub 2019 Apr 20. [DOI]
[2] Saimaitikari Abudoubari, Ke Bu, Yujie Mei at al. Prostate cancer epidemiology and prognostic factors in the United States. Front Oncol. 2023 Oct 12;13:1142976. doi: 10.3389/fonc.2023.1142976. [DOI]
[3] Oskar Bergengren, Kelly R Pekala, Konstantina Matsoukas at al. 2022 Update on Prostate Cancer Epidemiology and Risk Factors—A Systematic Review. Eur Urol. Author manuscript; available in PMC: 2024 Aug 1. Published in final edited form as: Eur Urol. 2023 May 16;84(2):191–206. doi: 10.1016/j.eururo.2023.04.021. [DOI]
[4] Trevor K Wilson, Oliver T Zishiri. Prostate Cancer: A Review of Genetics, Current Biomarkers and Personalised Treatments. Cancer Rep (Hoboken). 2024 Oct 16;7(10):e70016. doi: 10.1002/cnr2.70016. [DOI]
[5] Mamello Sekhoacha, Keamogetswe Riet, Paballo Motloung at al. Prostate Cancer Review: Genetics, Diagnosis, Treatment Options, and Alternative Approaches. Molecules. 2022 Sep 5;27(17):5730. doi: 10.3390/molecules27175730. [DOI]
Read:
A Comprehensive Guide to Getting Prostate Cancer Treatment
Stage 4 Prostate Cancer Treatment in Germany: What You Need to Know
Article menu:
- How is Prostate Cancer Diagnosed?
- How is the Prostate Cancer Test Called?
- Differential Diagnostics
- Biochemical Recurrence of Prostate Cancer
- Clinical Diagnosis
- Can Prostate Cancer Be Seen on the Ultrasound?
- Confirmation of Diagnosis
- Staging
- Clinical Signs of Prostate Cancer
- How does prostate cancer develop in the 3rd stage?
- Symptoms of Prostate Cancer in Stage 4
- Hospitals and The Cost of Treatment
- A Medical Journey: Every Step of the Way With Booking Health
- FAQ: Prostate Cancer Diagnosis
Don't know where to start?
Contact Booking Health












